CHAPTER 15 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 15 – Coracoid Transfer: The Modified Latarjet Procedure for the Treatment of Recurrent Anterior Inferior Glenohumeral Instability in Patients with Bone Deficiency
Stephen S. Burkhart, MD
Traumatic anterior inferior glenohumeral instability is a frequent problem in an active youthful population. Fortunately, primary surgical stabilization of the patient with recurrent traumatic dislocations, whether arthroscopic or open, has been predictably gratifying for both the patient and the surgeon. The best results have been obtained with accurate identification and treatment of the pathologic lesions without alteration of normal anatomy. In most cases, this involves repair of the avulsed anterior inferior labrum and inferior glenohumeral ligament to the glenoid rim. This “essential lesion” or Bankart lesion is present in as many as 97% of traumatic dislocations.[18] Successful correction of recurrent instability has been reported in more than 90% of patients by surgeons using both arthroscopic and open techniques to repair the Bankart lesion. However, the most frequently reported complication after both arthroscopic and open surgery for traumatic anterior instability is recurrent instability. [12] [16] Undoubtedly a significant number of treatment failures are related to a failure to recognize and to treat the full extent of the pathologic process.
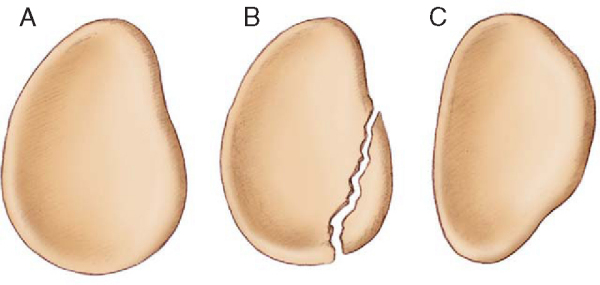
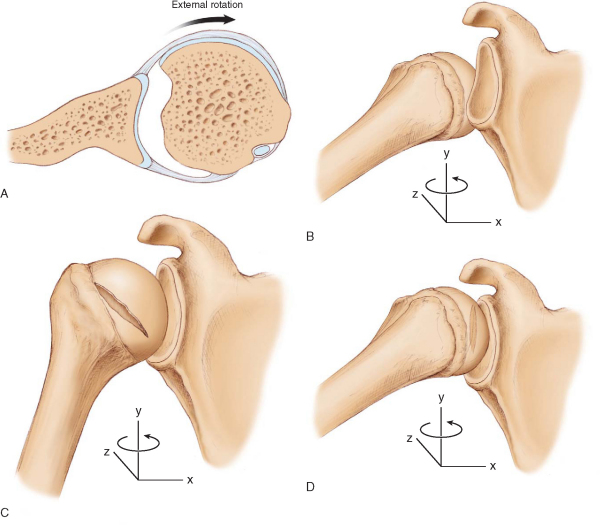
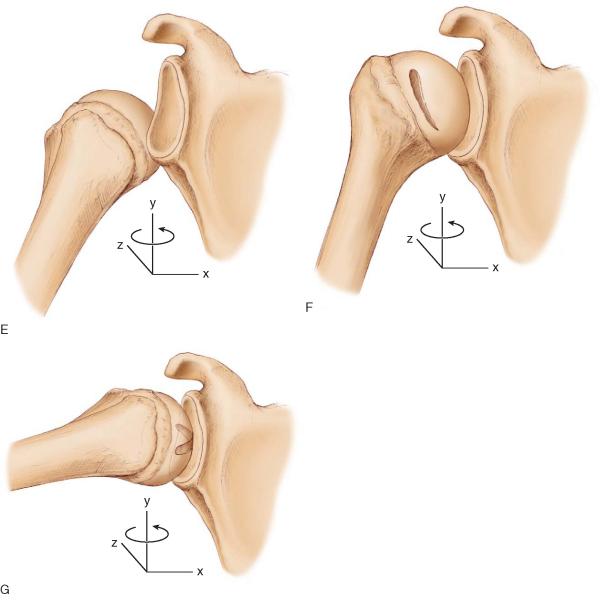
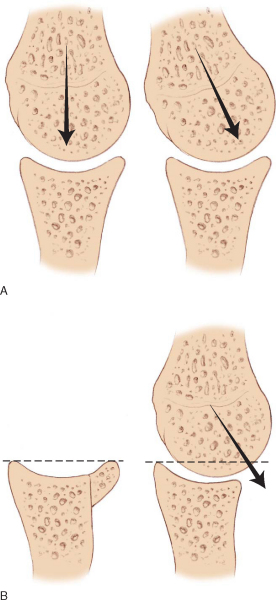
In the senior author’s experience, arthroscopic treatment of patients with recurrent traumatic anterior instability has been successful in all patients except those with significant bone deficiency. Problematic bone deficiency may occur on either the glenoid or humeral side of the shoulder joint. We believe that loss of more than 25% of the inferior glenoid diameter (inverted pear) or an engaging Hill-Sachs lesion (a Hill-Sachs lesion that engages the anterior glenoid rim in the position of overhead athletic function, that is, 90 degrees of abduction and 90 degrees of external rotation) constitutes problematic bone deficiency (Figs. 15-1 to 15-3 [1] [2] [3]). In a series of 194 patients, Burkhart and De Beer reported a 4% recurrence rate for arthroscopic suture anchor Bankart repair in patients without significant bone deficiency. However, 67% of the 21 patients with significant bone deficiency (by the preceding criteria) had recurrent instability after an arthroscopic Bankart repair.[3] This clinical dilemma, the young active patient with recurrent traumatic anterior instability and a significant bone deficiency, presents the orthopedist with a difficult therapeutic challenge. We have found a modified Latarjet reconstruction to be the most effective form of treatment. The original Latarjet procedure, developed and reported in 1954, transfers a large segment of the coracoid (2.5 to 3 cm in length) as bone graft to the anterior inferior glenoid rim.[11] We have incorporated several modifications to the original Latarjet procedure that we believe will improve the long-term results.
The modified Latarjet coracoid transfer is a technically demanding operation that can provide a safe and reliable solution with lasting positive results in a challenging population of patients. We recommend this treatment for young active patients with recurrent anterior inferior shoulder instability associated with the inverted-pear configuration of glenoid bone deficiency or an engaging Hill-Sachs lesion. Graft placement and orientation are critical to both the short-term and long-term success of this operation.
|
|
|
|
Figure 15-1 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
|
|
|
|
Figure 15-2 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
|
|
|
|
Figure 15-3 |
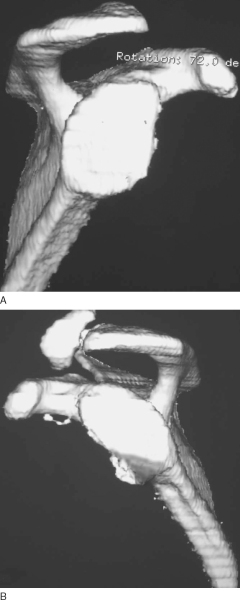
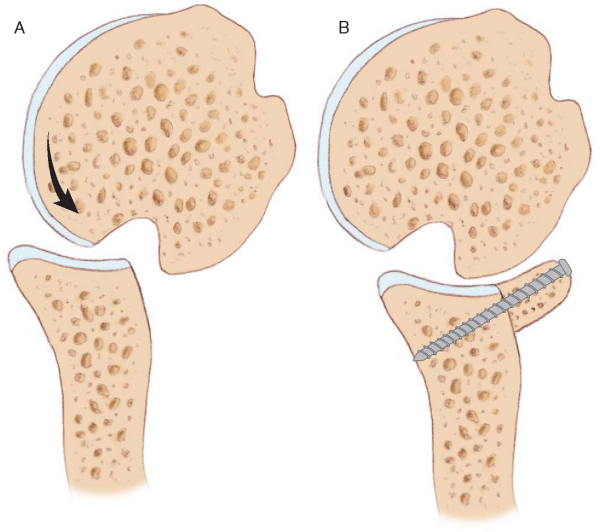
The efficacy of this procedure can be explained by the combination of four main effects. First, the large bone graft replaces glenoid bone loss and augments the concavity of the glenoid articular arc. This effect diminishes the shoulder’s propensity for dislocation during off-axis loads (
Fig. 15-4
). Second, in the case of the engaging Hill-Sachs lesion, the extended articular arc provided by the coracoid graft prevents engagement of the humeral bone defect. The shoulder is not able to externally rotate to the degree necessary for engagement over the front of the graft (
Fig. 15-5
). Third, the transferred conjoined tendon acts as a tether, restricting external rotation to some extent, and the posterior capsule restricts anterior translation of the humeral head over the augmented glenoid concavity. Finally, the transferred conjoined tendon forms a sling across the anterior inferior capsule when the shoulder is abducted and externally rotated, serving as an additional constraint to anterior inferior translation.
|
|
|
|
Figure 15-4 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
|
|
|
|
Figure 15-5 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
A thorough history is essential and should elicit the mechanism of injury and prior treatments received. Previous operative reports should be obtained and reviewed; they often yield valuable information about areas of bone deficiency, tissue quality, and fixation devices used. The physical examination determines the position and direction of instability as well as identifies or eliminates factors that contribute to instability.
Essential Components of the History
Preoperative radiographs give valuable information about various areas of bone deficiency. However, quantification of bone loss based on plain radiographs is difficult. Three-dimensional computed tomographic scans of bilateral shoulders have been extremely valuable in allowing accurate quantification of glenoid and humeral bone loss (see
Fig. 15-3
). The magnetic resonance imaging scan is also essential to allow accurate identification of the spectrum of pathologic lesions responsible for instability (Bankart, SLAP, humeral avulsion of the glenohumeral ligament, capsular redundancy, and bone defects).
Indications and Contraindications
Surgery is indicated for active patients with recurrent anterior inferior instability and bone deficiency defined by at least one of the following:
| • | Active infection in or around the shoulder joint | |
| • | Intentional and voluntary dislocations (relative contraindication) |
The procedure is usually performed under a combination of general anesthesia with endotracheal intubation or laryngeal mask ventilation and regional anesthesia through an interscalene nerve block. The patient is positioned in the beach chair or lateral decubitus position for the arthroscopic part of the procedure. The coracoid transfer is best performed in the beach chair position.
Surgical Landmarks, Incisions, and Portals
Similar to standard arthroscopy, the anatomic landmarks should be drawn out. Diagnostic arthroscopy uses the standard anterior and posterior portals; the coracoid transfer is performed through a standard deltopectoral approach.
Examination Under Anesthesia and Diagnostic Arthroscopy
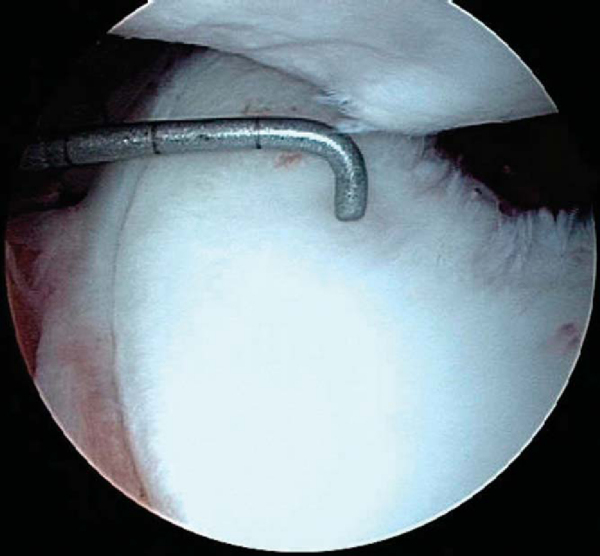
Accurate identification of the full extent of the pathologic process is the first major goal. Examination under anesthesia should confirm the degree and position of laxity. We believe it is essential to begin with diagnostic arthroscopy so that any bone deficiency can be identified and quantified and concomitant pathologic lesions (SLAP lesions) may be treated arthroscopically before the open coracoid transfer.
The posterior, anterior, and anterior superior portals are generally used for diagnostic arthroscopy. Glenoid bone deficiency is evaluated by viewing from the anterior superior portal while using a calibrated probe through the posterior portal. The shape of the glenoid is assessed, and the probe is used to quantify the amount and location of bone loss (
Fig. 15-6
). The normal inferior glenoid has an average anterior-posterior diameter of 23 mm, and the bare spot normally lies in the center of this measurement.[5] This information gives the surgeon a simple method of quantifying the percentage of glenoid bone deficiency (
Box 15-1
). Our data have shown that 25% or greater glenoid bone loss is significant, and in this scenario, the glenoid assumes the shape of an inverted pear.
|
|
|
|
Figure 15-6 |
| Estimation of Glenoid Bone Deficiency | ||||||
|
To assess the humerus for a significant bone defect, previously defined as an engaging Hill-Sachs lesion, we sequentially view from the posterior portal and then the anterosuperior portal with the arm removed from traction. The arm is placed in the position of apprehension, usually 90 degrees of abduction and 90 degrees of external rotation, and we observe whether the humeral head defect slides onto or engages the anterior rim of the glenoid (see
Fig. 15-2
). If the humeral head defect is oriented such that it is oblique to and does not engage the anterior glenoid rim in the 90-90 position, it is a nonengaging and less significant lesion.
If a significant bone deficiency is identified on either the glenoid or humerus, we proceed with the modified Latarjet procedure, after first treating other concomitant pathologic lesions (such as a SLAP lesion) arthroscopically. However, if the bone defect does not meet these criteria for significance, we treat identified intraarticular disease including the Bankart lesion arthroscopically.
The Modified Latarjet Procedure
Specific Steps (
Box 15-2
)
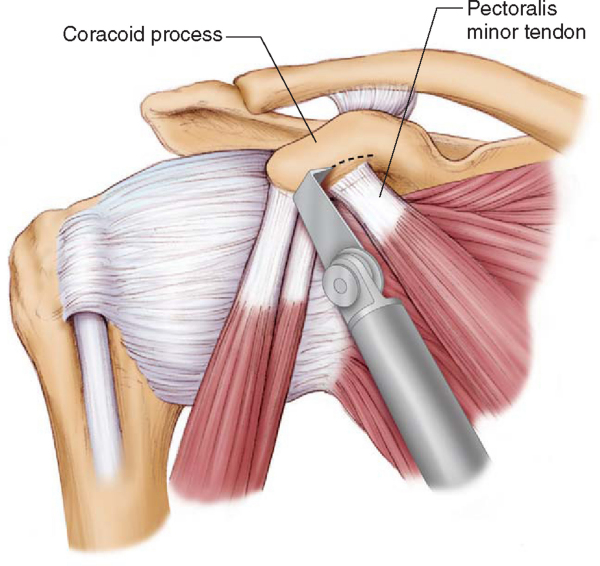
A standard deltopectoral approach is used to begin the modified Latarjet procedure. The cephalic vein is carefully dissected and generally retracted laterally, preserving the major branches to the deltoid. The clavipectoral fascia is divided and the coracoid is exposed to its base where the coracoclavicular ligaments insert. The coracoacromial ligament is released from the lateral tip of the coracoid, and the pectoralis minor tendon is sharply dissected free from the medial surface of the coracoid (
Fig. 15-7
). It is this medial surface of the coracoid that will later be approximated to the anterior glenoid neck.
|
|
|
|
Figure 15-7 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
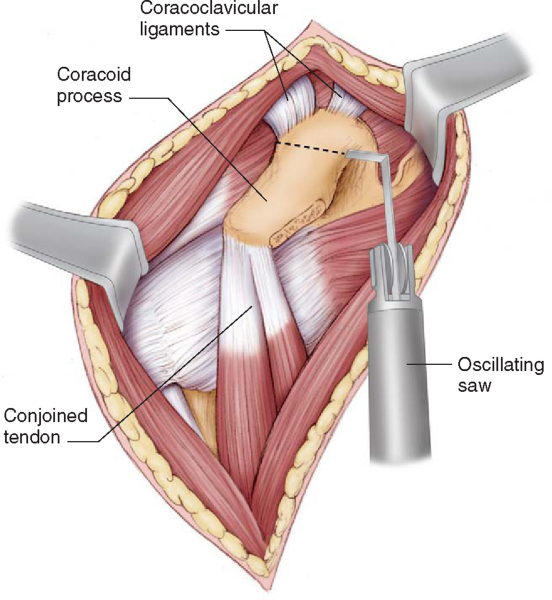
Next, a 70-degree angled sagittal saw blade is used to osteotomize the coracoid at its base, just distal to the insertion of the coracoclavicular ligaments (
Fig. 15-8
). In general, 2.5 to 3 cm of coracoid graft is obtained. We think that use of an angled saw simplifies the osteotomy by allowing an easier angle of approach and makes scapular or glenoid fracture much less likely. Neurovascular structures are protected with Chandler elevators placed medially and inferiorly.
|
|
|
|
Figure 15-8 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
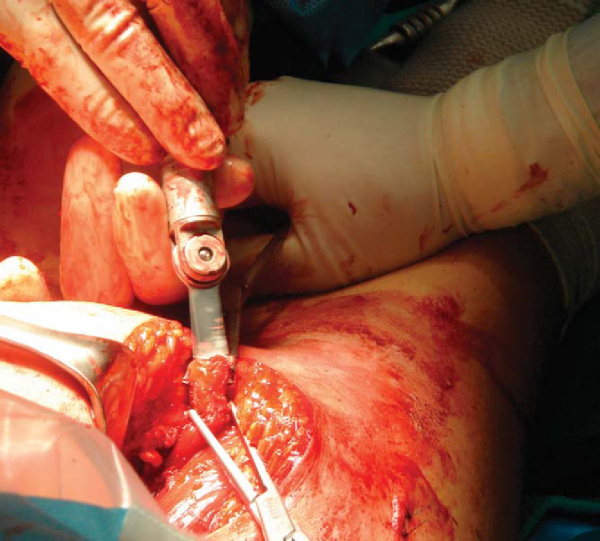
3. Graft Mobilization and Preparation
It is crucial that the conjoined tendon be left attached to the coracoid graft. This preserves some blood supply to the graft (a vascularized graft) and, we believe, speeds consolidation. The transferred coracoid graft will continue to serve as a stable attachment for the short head of the biceps and coracobrachialis muscles. The conjoined tendon and graft must be mobilized for transfer to the anterior glenoid neck. Great care must be maintained during this step so as not to cause stretch injury to the musculocutaneous nerve, which enters the coracobrachialis muscle a variable distance (approximately 5 cm) distal to the coracoid attachment.[7] Next, the medial coracoid surface (pectoralis minor insertion site) is prepared to a bleeding cancellous surface by shaving off the thin cortical layer with the sagittal saw (
Fig. 15-9
). The graft is tucked in the medial tissue for later use.
|
|
|
|
Figure 15-9 |
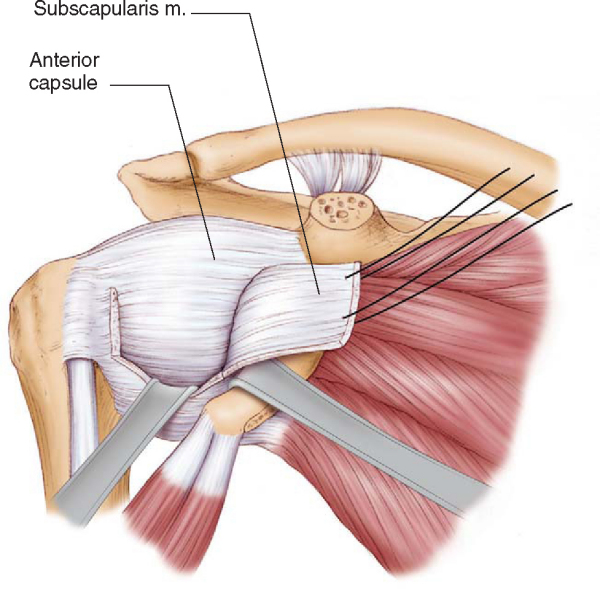
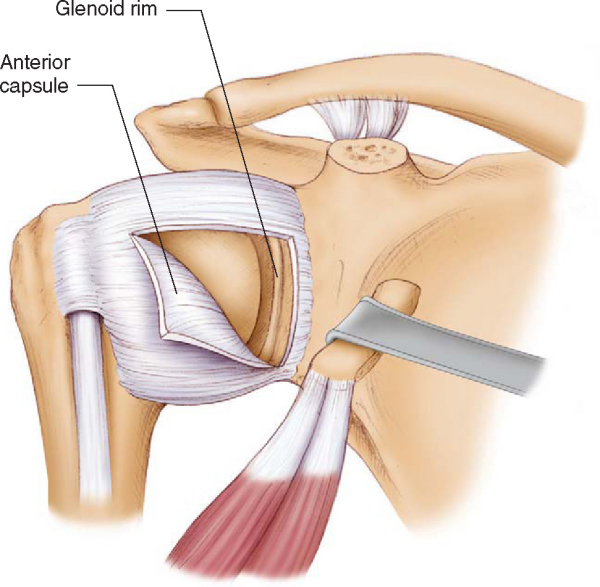
An excellent exposure of the anterior shoulder is obtained once the coracoid has been osteotomized. The superior half of the subscapularis tendon is detached distally from just medial to the biceps tendon while preserving the underlying capsule (
Fig. 15-10
). Tagging sutures (No. 2 FiberWire; Arthrex, Inc., Naples, Fla) are placed in the superior half of the subscapularis with a grasping stitch and are used to assist with dissection between tendon and capsule as well as for later repair. This portion of the subscapularis tendon is reflected medially, and the lower half of the tendon is preserved intact throughout. (Although it is conceptually tempting to perform this operation through a simple split in the subscapularis, the exposure gained by reflecting the superior half of subscapularis is much more reproducible for glenoid preparation, graft orientation, and fixation.) Next, the plane between the remaining lower subscapularis and capsule is developed, and a vertical capsular incision is made 1 cm medial to the glenoid rim. The capsule and underlying labrum are reflected laterally by sharp subperiosteal dissection (
Fig. 15-11
). Maximal length of the capsular flap is necessary for later repair.
|
|
|
|
Figure 15-10 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
|
|
|
|
Figure 15-11 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
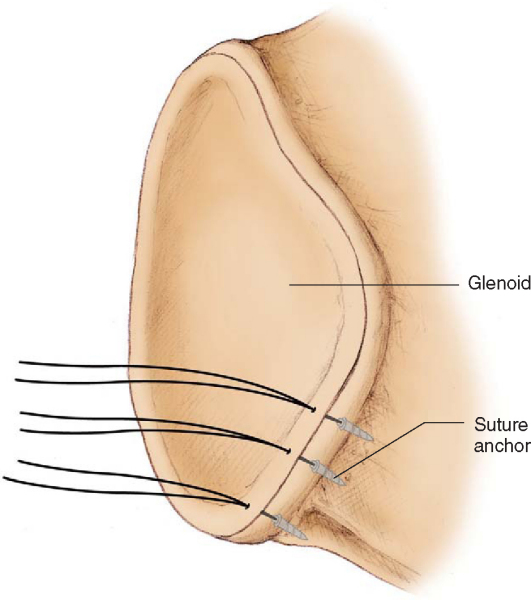
The anterior glenoid neck and rim are prepared as the recipient bone bed for grafting by use of curets and high-speed bur (a light dusting). The goal here is to establish a bleeding bone surface devoid of fibrous tissue while removing as little bone structure as possible. Three suture anchors (3.0 mm Bio-Suture Tak; Arthrex, Naples, Fla) are placed at the native glenoid rim at the 3-, 4-, and 5-o’clock positions (right shoulder) and are used later for capsular repair (
Fig. 15-12
).
|
|
|
|
Figure 15-12 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
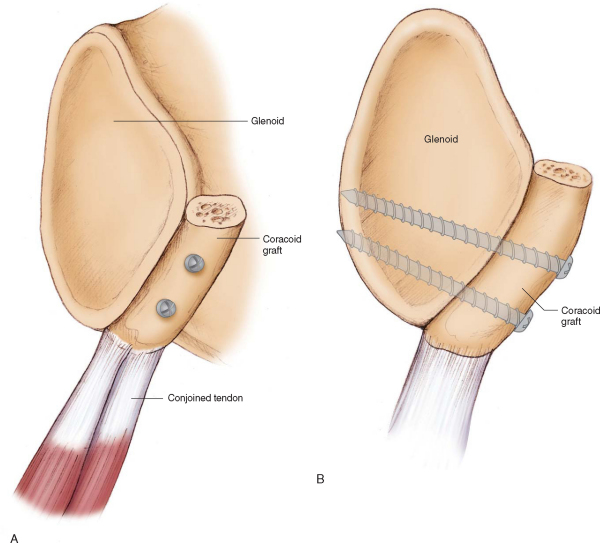
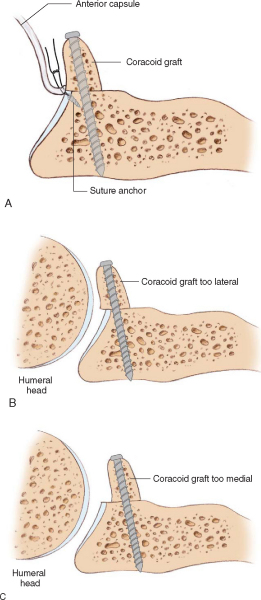
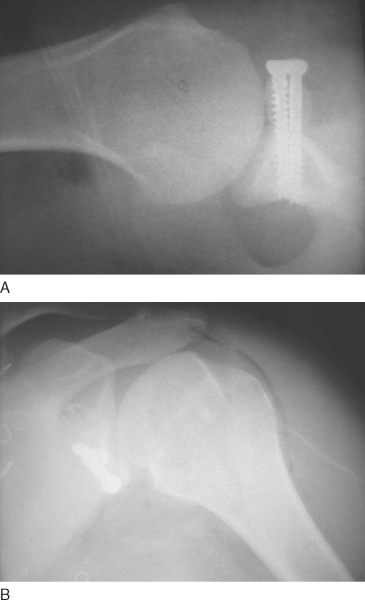
6. Graft Placement, Orientation, and Fixation
The coracoid seems perfectly formed for placement as an anterior glenoid bone graft. The curved contour of the coracoid bone (original inferior surface) seems to perfectly match the radius of curvature of the anterior inferior glenoid. The prepared medial surface of the coracoid graft is placed against the recipient anterior inferior glenoid neck with the long axis of the graft oriented superior to inferior (
Fig. 15-13
). Minor graft rotation and trimming are performed as necessary for best fit. Proper positioning of the coracoid graft relative to the glenoid rim is critically important for success in preventing recurrent dislocation and for the avoidance of late degenerative arthritis (
Fig. 15-14
). The graft is placed not as a bone block but rather so that it functions as an extension of the glenoid articular arc. The graft is temporarily fixed in place with guide pins for the 4.0-mm cannulated screws. If the graft is sufficiently large, we prefer to use the 4.5-mm cannulated screw set as the guide pin is considerably more robust. When the surgeon is satisfied with orientation and fit, the graft is permanently secured with two cannulated screws, achieving purchase in the far glenoid cortex. Screw lengths have been remarkably consistent at 36 and 34 mm, although intraoperative radiographs are always obtained to confirm graft position and fixation (
Fig. 15-15
). At this point, before capsular closure, we generally irrigate the joint copiously and take the shoulder through range of motion to assess stability. Once the coracoid graft has been secured, we have found that dislocation is virtually impossible even in the most provocative position. Finally, the previously reflected capsule is repaired by means of the suture anchors to the native glenoid rim. This places a synovium-lined tissue layer between the coracoid graft and humeral head, preventing the humeral articular surface from abrading against the coracoid graft.
|
|
|
|
Figure 15-13 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
|
|
|
|
Figure 15-14 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
|
|
|
|
Figure 15-15 |
The superior half of the subscapularis tendon is repaired to its insertion by means of the previously placed FiberWire tagging sutures. The conjoined tendon, remaining attached to the coracoid graft, now passes through the remaining horizontal split in the subscapularis tendon (
Fig. 15-16
). Finally, the wound is thoroughly irrigated, and standard closure of the subcutaneous and subcuticular layers is performed. The patient is placed in a sling with a small pillow. A consistent postoperative rehabilitation protocol is followed.
|
|
|
|
Figure 15-16 (Redrawn with modification from Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-694.) |
| • | A padded sling is worn for the first 4 weeks. It is removed three times daily for passive external rotation to neutral. | |
| • | The immobilizer is discontinued at 4 weeks, and passive overhead motion is encouraged. | |
| • | Gentle external rotation stretching is initiated at 6 weeks. | |
| • | The surgically repaired shoulder should have 50% of the normal shoulder’s external rotation at 3 months. | |
| • | Strengthening exercises are delayed until there is radiographic evidence of early graft consolidation (usually 3 to 4 months). | |
| • | Heavy labor and sporting activity are generally allowed at 6 months. |
The majority of the reported complications are related to the coracoid graft harvest and the position of graft fixation along the glenoid.
| • | Instability can recur if the graft is secured too medial on the glenoid neck. | |
| • | Scapula fracture has been reported during graft harvest with the osteotome. | |
| • | Late graft fracture and recurrent dislocation have occurred after traumatic athletic injury. | |
| • | Fibrous union or nonunion of the graft may result. | |
| • | Postoperative infection has occurred in 0% to 5% of patients. | |
| • | Significant glenohumeral arthritis developed in 20% of patients at 14 years of followup. |
| PEARLS AND PITFALLS | |||||||||
|
To date, there have been only four reports of the Latarjet procedure in the English language literature (
Table 15-1
), [1] [3] [4] [19] although there are many reports of the Bristow procedure (often called the Latarjet-Bristow procedure), which is a significantly different procedure that transfers only the coracoid tip to the glenoid neck. Regarding the Latarjet procedure, Burkhart et al[3] reported the results of 104 patients an average of 39 months after reconstruction. Six complications were reported, including one hematoma that required evacuation, one fibrous union with loose screws, and four recurrent dislocations and one recurrent subluxation (4.9% recurrence rate). All recurrent dislocations were related to violent trauma in the early postoperative period and occurred with graft dislodgement. Patients achieved an average of 179.6 degrees of forward elevation (2.4 degrees improved from preoperative range) and an average of 48.1 degrees of external rotation with the arm at the side (7.3 degrees less than preoperative range). The authors concluded that this is a safe and effective procedure for a challenging clinical problem.
| Author | Followup | Outcome | Conclusion |
|---|---|---|---|
| Allain et al[1] (1998) | 14.3 years mean (range: 10-23) | 88% good and excellent results by grading system of Rowe 1 of 58: persistent instability |
Precise graft placement is critical to avoid recurrent instability and late glenohumeral arthritis. |
| Burkhart and De Beer[4] (2000) | 39 months (range: 12-88) | 5 of 104: recurrent instability 4 of 5 failures related to violent trauma with graft dislodgement |
Modified Latarjet procedure is a safe and reliable treatment of patients with recurrent instability and bone deficiency. |
Allain et al[1] retrospectively reviewed 56 patients an average of 14.3 years after the Latarjet procedure for recurrent anterior instability. The primary purpose of this research was to determine the prevalence of glenohumeral arthritis and factors related to its development. At the latest followup, there were no cases of postoperative dislocation despite presence of the apprehension sign in six patients. Eleven patients (20%) were thought to demonstrate significant glenohumeral arthritis. The authors concluded that the development of glenohumeral arthritis is most closely related to a preoperative tear of the rotator cuff and too lateral placement of the coracoid graft.
1.
Allain J, Goutallier D, Glorion C: Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder.
J Bone Joint Surg Am 1998; 80:841-852.
2.
Bigliani LU, Newton PM, Steinmann SP, et al: Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder.
Am J Sports Med 1998; 26:41-45.
3.
Burkhart S, De Beer J, Barth J, et al. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy; in press.
4.
Burkhart SS, De Beer JF: Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion.
Arthroscopy 2000; 16:677-694.
5.
Burkhart SS, De Beer JF, Tehrany AM, Parten PM: Quantifying glenoid bone loss arthroscopically in shoulder instability.
Arthroscopy 2002; 18:488-491.
6.
Churchill RS, Moskal MJ, Lippett SB, Matsen III FA: Extracapsular anatomically contoured anterior glenoid bone grafting for complex glenohumeral instability.
Tech Shoulder Elbow Surg 2001; 2:210-218.
7.
Eglseder Jr WA, Goldman M: Anatomic variations of the musculocutaneous nerve in the arm.
Am J Orthop 1997; 26:777-780.
8.
Helfet AJ: Coracoid transplantation for recurring dislocation of the shoulder.
J Bone Joint Surg Br 1958; 40:198-202.
9.
Itoi E, Lee SB, Berglund LJ, et al: The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study.
J Bone Joint Surg Am 2000; 82:35-46.
10.
Kim SH, Ha KI, Kim YM: Arthroscopic revision Bankart repair: a prospective outcome study.
Arthroscopy 2002; 18:469-482.
11.
Latarjet M: Apropos du traitement des luxations récidivantes de l’epaule.
Lyon Chir 1954; 49:994-1003.
12.
Lazarus M, Harryman D: Complications of open anterior stabilization of the shoulder.
J Am Acad Orthop Surg 2000; 8:1222.1132
13.
Lo IK, Parten PM, Burkhart SS: The inverted pear glenoid: an indicator of significant glenoid bone loss.
Arthroscopy 2004; 20:169-174.
14.
Maynou C, Cassagnaud X, Mestdagh H: Function of subscapularis after surgical treatment for recurrent instability of the shoulder using a bone-block procedure.
J Bone Joint Surg Br 2005; 87:1096-1101.
15.
Mazzocca AD, Brown FM, Carreira DS, et al: Arthroscopic anterior shoulder stabilization of collision and contact athletes.
Am J Sports Med 2005; 33:52-60.
16.
Stein DA, Jazrawi L, Bartolozzi AR: Arthroscopic stabilization of anterior shoulder instability: a review of the literature.
Arthroscopy 2002; 18:912-924.
17.
Tauber M, Resch H, Forstner R, et al: Reasons for failure after surgical repair of anterior shoulder instability.
J Shoulder Elbow Surg 2004; 3:279-285.
18.
Thomas S, Matsen III FA: An approach to the repair of avulsion of the glenohumeral ligaments in the management of traumatic anterior glenohumeral instability.
J Bone Joint Surg Am 1989; 71:506-513.
19.
Walch G, Boileau P: Latarjet-Bristow procedure for recurrent anterior instability.
Tech Shoulder Elbow Surg 2000; 1:256-261.