Cervical Trauma
cause of morbidity and mortality throughout the world. Most patients
with closed spinal column injury are young men, whose injury often
results from motor vehicle accidents, falls, or sports injuries. A
second peak in prevalence exists in adults age 50 and older. Injuries
in this age group are related predominantly to falls. Categorizing
these injuries has allowed spine care specialists to evaluate more
adeptly and treat affected patients.
cervical spine is essential for accurate injury identification and
treatment planning. Although the anatomy of the subaxial cervical spine
is largely consistent, the anatomy of the upper cervical spine is
unique at each level. Bony restraints of the occipitocervical junction
involve the convex occipital condyles articulating with the lateral
masses of the atlas (C1). Children younger than 12 years old have more
unrestricted motion and are predisposed to injury at the
occipitocervical junction. The posterior arch of C1 provides a bony
limit to occiput extension. Ligamentous restraints are formed primarily
by the alar ligaments, which course from the superolateral aspect of
the odontoid process to the medial occipital condyle. Motion at this
segment approximates 21 degrees of extension, 3 degrees of flexion, 7
degrees of rotation to each side, and 5 degrees of lateral bending to
each side.
skull and the axis. It relies on two lateral masses for weight bearing.
Embryologically the caudal part of the C1 somite joins with the cranial
C2 somite to form the odontoid process. By 3 to 6 years of age, the
dens fuses with the body. In the absence of a disc between the occiput
and C1, the anatomic relationship is maintained by ligamentous
relationships. The atlantooccipital membrane attaches to a tubercle at
the base of the skull and is confluent with the anterior longitudinal
ligament. The apical ligament attaches the tip of the dens to the
anterior edge of the foramen magnum. The posterior longitudinal
ligament continues superiorly as the tectorial membrane. The most
important ligamentous restraint to anterior translation of the C1-2
complex is the transverse ligament, which traverses posterior to the
odontoid to attach to the C1 lateral masses. Secondary restraint comes
from the alar ligaments, which arise along the medial aspect of the
occiptal condyles and lateral masses of C1 and insert onto the lateral
aspect of the odontoid. Approximately 15 degrees of flexion/extension
occurs at the occipitoatlantal junction. The muscular attachments to
the cervical spine include the longus colli, which attach to the
anterior and inferior portions of the arch of C1. The rectus capitis
medialis and lateralis and the trapezius insert posteriorly.
(50%) contribute equally to rotation, most of the flexion and extension
in the cervical spine occurs from C3 to C7. At each motion segment of
the subaxial spine, 17 degrees of sagittal plane motion can occur.
Coronal motion ranges from 4 to 11 degrees per motion segment in this
region. The anterior longitudinal ligament and anulus fibrosus act as a
tension band limiting extension. Posteriorly the supraspinous and
interspinous ligaments and the ligamentum flavum resist flexion. The
cross-sectional area of the spinal canal is largest at C2 and smallest
at C7. Anterior radicular arteries supply the anterior spinal artery
(and the spinal cord) and posterior radicular arteries supply the
posterior spinal arteries. In the cervical spine, the radicular artery
originating from the deep cervical artery accompanying the left C6
spinal nerve root is the most significant.
have an initial evaluation according to standard advanced trauma and
life support protocols. The patient should be logrolled carefully and
the spine palpated for tenderness or step-off. A thorough neurologic
exam should be performed, focusing on key motor groups as suggested by
the American Spinal Injury Association classification. The Frankel
scale (A through E) is part of spinal injury classification, with A
representing complete motor and sensory function loss below the level
of injury and E representing normal motor and sensory function.
cervical spine shows 85% of injuries. The cervicothoracic junction
should be visible. If the lateral view is not sufficient, a swimmer’s
view is obtained. If still unclear, a computed tomography (CT) scan of
C7-T1 is obtained. In patients without significant clinical findings,
there is a 3.1% incidence of occult cervical trauma at the
cervicothoracic junction. Up to 16% of patients have noncontiguous
spinal fractures. Frequently, fractures at C1-2 are associated with a
remote subaxial fracture. The Power’s ratio is useful to evaluate
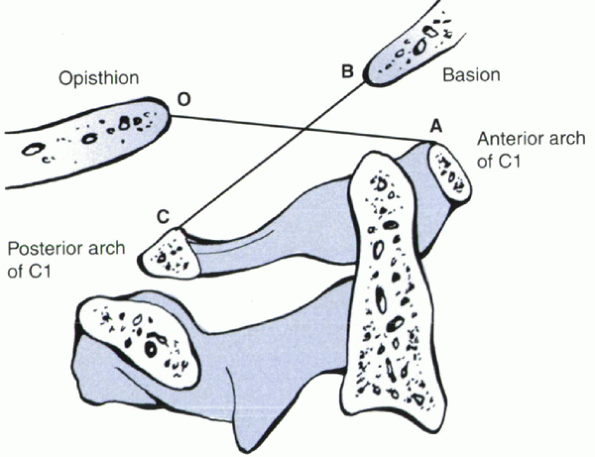
occipitocervical alignment (Fig. 4-1).
The ratio of a line drawn from the basion to the posterior arch of the
atlas over the line from the opisthion to the anterior arch of the
atlas should be less than 1. A ratio greater than 1 suggests an
anterior occipitoatlantal dislocation. Flexion/extension films normally
should reveal less than 1 mm of translation between the occiput and C1.
Greater than 1 mm indicates occipitoatlantal instability. The
atlantodental interval (ADI) is used to determine the stability of the
atlantoaxial segment. Values greater than 3 mm in an adult and 4 mm in
a child suggest rupture of the transverse ligament. Soft tissue shadows
often indicate undiagnosed cervical trauma. The normal prevertebral
soft tissue shadow anterior to C1 should be less than 10 mm, less than
7 mm at C3, and less than 20 mm at C6 in the noninjured cervical spine.
continue to evolve. Angulation greater than 11 degrees compared with
adjacent normal segments or translation greater than 3.5 mm are
guidelines developed by serial sectioning studies in cadavers to
simulate flexion injuries. Extension injuries can be subtle,
necessitating evaluation for anterior disc space widening or increase
in soft tissue density in the retropharyngeal space.
CT may help define the extent of bone damage. CT also is helpful when
the lower cervical spine cannot be visualized adequately on plain
radiographs.
 |
|
Figure 4-1
Power’s ratio. The ratio of BC to AO normally equals 1. If the ratio is greater than 1, an anterior occipitoatlantal dislocation may exist. |
-
Patients with neurologic deficits, particularly when CT does not show a reason for the deficit.
-
Patients with deteriorating neurologic status.
-
Cases of suspected posterior ligamentous injury not evident by plain radiographs or CT reconstructions.
radiographs were found to have disc or soft tissue injuries by MRI.
Controversy exists regarding the timing of obtaining these studies in
the acute trauma setting. We favor early restoration of cervical
alignment and protection, with traction, in an alert and cooperative
patient before obtaining an advanced imaging work-up, which can result
in delay or repeated transfers.
increasingly prevalent as improved trauma care has decreased acute
mortality. Injuries occur primarily by three mechanisms: compression,
distraction, and lateral rotation. Fractures are organized according to
CT morphology and potential instability. Occipital condyle fractures
may result from axial loading or distraction forces on the atlas as
classified by Anderson and Montesano. A type I injury is a comminuted fracture due to impaction of the occipital condyle into the lateral mass of the atlas. It is usually stable. A type II injury
is an occipital condyle fracture associated with a basilar skull
fracture, usually from a direct blow. Stability is compromised when the
entire condyle is separated from the occiput. Rotation or lateral
bending may result in an avulsion fracture of the occipital condyle by
the alar ligament; this is a type III injury.
Any anteroposterior displacement or incongruent articulation may be an
indication of underlying instability in type III patterns. Rigid collar
immobilization for 6 to 8 weeks is recommended for type I and most type
II injuries. Type III injuries are unstable and require posterior
fusion.
-
Type II
injury is a distraction injury with vertical separation of the occiput
from the atlas. These injuries should not be placed in traction because
this may exacerbate the deformity and result in further neurologic
compromise. -
Type III injury is a rare posterior displacement of the occiput with respect to the atlas.
|
TABLE 4-1 CLASSIFICATION OF OCCIPITOCERVICAL INSTABILITY
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
traction initially. If intubation is necessary, it should be
nasotracheal. Halo vest immobilization usually is recommended for 3
months with subsequent flexion and extension radiographs to assess
stability. Type II injuries usually require occipitoatlantal fusion.
been reported. Fusion can be achieved using posterior wiring from the
outer table of the occiput to the atlas as described by Cone and
Bohlman. Modifications include addition of a contoured rod and passage
of sublaminar wires to achieve fixation. Occipitocervical plating with
reconstruction plates also is an option with screw fixation of the
occiput and transarticular C1-2 screw placement. C2 pedicle screws also
may be placed as an alternative.
spine fractures. Five distinct fracture patterns can be recognized, as
follows:
-
The most common injury is the posterior arch fracture, which usually occurs at the junction of the lateral masses.
-
A second pattern involves fractures
anterior to the lateral mass on one side and posterior on the
contralateral side, creating a free-floating lateral mass. -
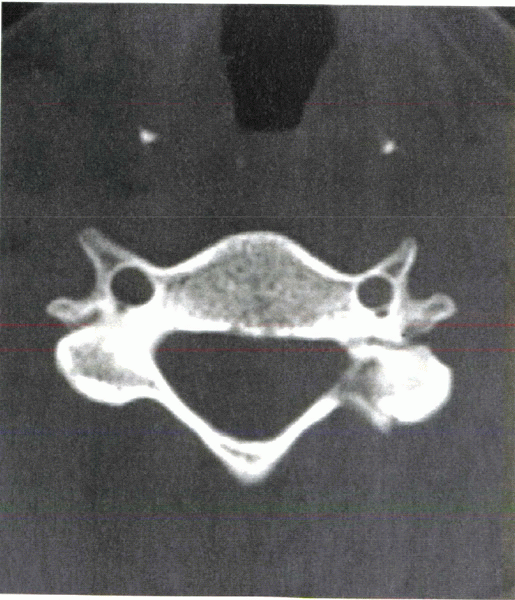
Simultaneous fractures of the anterior
and posterior rings are characteristic of Jefferson’s fracture, which
tends to displace laterally. -
Horizontal fractures can occur through the anterior tubercle of C1.
-
Transverse process fractures of C1 may be unilateral or bilateral.
from hyperextension. Associated injuries of C2, such as an anterior
teardrop fracture and spondylisthesis of the axis, should be ruled out
if this mechanism of injury is suspected. Lateral mass fractures are a
result of combined axial loading and lateral bending. Associated
fractures include lower cervical facet fractures. Combined displacement
of the lateral masses (Jefferson’s fracture) greater than 6.9 mm can be
associated with failure of the transverse ligament. The alar and apical
ligaments and the C1-2 capsule usually are spared, however. Severe
hyperflexion movements disrupt the transverse, alar, and apical
ligaments. Hyperextension results in an avulsion; this may be due to
forceful contraction of the superior oblique portion of the longus
colli. Transverse process fractures are usually from a forced lateral
compressive (ipsilateral) injury with a contralateral avulsion
fracture. This pattern may be associated with laminar fractures in the
lower cervical spine as well.
includes a cervical orthosis, Minerva cast, or halo fixator. If the
transverse ligament is ruptured, early C1-2 arthrodesis may be
considered. Surgery usually is indicated for the associated spine
injuries. Commonly associated injuries are fractures of the dens and
traumatic spondylolisthesis (hangman’s fracture) of the axis. Fractures
of the posterior arch of the atlas by themselves are stable injuries
and amenable to closed treatment with a cervical orthosis. Lateral mass
fractures with minimal displacement may be treated with rigid orthoses
or halo immobilization. Displaced fractures with greater than 7 mm
usually are associated with rupture of the transverse ligament. Some
authors have recommended attempted reduction with axial traction
through a halo ring as the initial step in treatment of this injury.
This is followed by 1 to 2 weeks of bed rest with traction. Halo vest
immobilization should be maintained for 3 months.
of cervical spine fractures. Motor vehicle accidents account for most
injuries in patients age 16 to 34 years. Falls account for most
injuries in patients older than age 55 and younger than age 15.
-
Type I
odontoid fractures involve the tip of the dens. This may result from a
severe rotational or lateral bending force that causes an avulsion of
bone through the alar and apical ligaments. Other distraction injuries
must be ruled out. -
Type II
fractures occur through the “waist” of the dens without involvement of
the C2 body and have nonunion rates of 11% to 100%. Risk factors for
nonunion are (1) age greater than 60, (2) more than 5 mm displacement
and 9 degrees of angulation, and (3) smoking. -
Type III
fractures are through the body of C2. In marked contrast, this has a
union rate that may approach 100%, a consequence of larger surface
areas and more vascular cancellous bone.
in the absence of occipitocervical instability. Type III fractures and
type II fractures with less than 10 degrees of angulation and 5 mm of
displacement can be treated with a halo fixator. Greater displacement
should be treated with initial traction for a better reduction followed
with early conversion to a halo vest. Displaced or significantly
angulated type II fractures often are treated with posterior
atlantoaxial arthrodesis using autogenous bone graft or osteosynthesis
with an anterior odontoid screw, which theoretically preserves more
motion.
of the transverse ligament. This disruption can result from trauma and
congenital, infectious, and inflammatory processes. The transverse
ligament functions primarily as restraint
against
anterior subluxation of C1 on C2. Fielding reported that an intact
transverse ligament allows a maximum of 3 mm of anterior translation of
C1 on C2. Failure of the ligament is inferred with greater than a 3 mm
ADI. High-resolution CT or MRI can be used to evaluate a midsubstance
tear or avulsion fracture. Axial gradient-echo MRI is the best modality
to visualize the transverse ligament. Treatment is aimed at restoring
stability when the ADI measures more than 5 mm. Posterior C1-2
arthrodesis is preferred. Children may be managed with a trial of rigid
halo fixation for 2 to 3 months. C1-2 arthrodesis is performed in the
presence of persistent pain or an anterior ADI greater than 5 mm in
flexion. The best healing rates with nonoperative treatments are with
bony avulsion fractures.
lower cervical spine. The superior articular facets of C2 lie anterior
to the neural elements and in line with the C1-2 lateral masses,
whereas the inferior facets are posterior to the canal and are in line
with the lower cervical lateral masses. The transitional nature of this
vertebra places greater stresses on the pars interarticularis with
loading. Injury occurs with a combination of extension, axial
compression, and flexion. A fracture line results that propagates
through the C2 pars interarticularis; this can result in
anterolisthesis of the C2 body on C3. Patients rarely have neurologic
deficit owing to the large size of the canal at this level. The
fracture displacement tends to increase the effective canal size.
 |
|
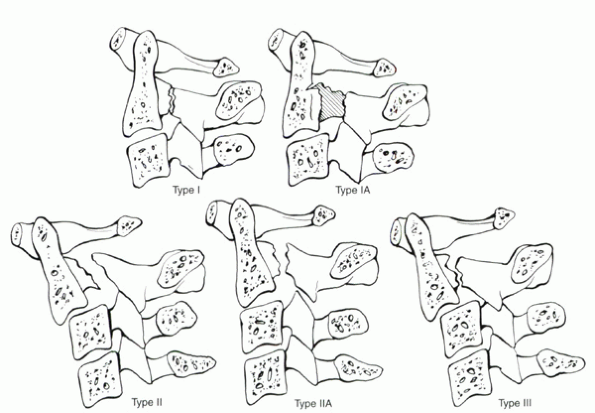
Figure 4-2
Classification of hangman’s fractures. Type I—minimal separation of the fragments, without significant angulation or translation. Type IA—oblique fracture through posterior portion of vertebral body may be difficult to visualize on lateral radiograph. There may be apparent elongation of the vertebral body and pars. Type II—relatively vertical fracture with separation of the fragments, angulation, and translation of C2 on C3. Type IIA—oblique fracture line by failure of pars in tension, no translation, but significant angulation of C2 on C3. Type III—combined injury, with type I fracture of pars and C2-3 facet dislocation. |
-
Type I
fractures occur through the neural arch at the base of the pedicle and
show less than 3 mm of translation and no angulation at the fracture
site. They result from a hyperextension and axial load and do not
include significant injury to the disc, longitudinal ligaments, or
adjacent body of C3. Type IA injuries are
less evident on lateral plain films because of the obliquity of the
fracture line across the body of C2 (often through the foramen
transversarium). There may be apparent elongation of
P.39C2
by 2 or 3 mm of translation of the anterior aspects of the C2 body with
relative anatomic alignment of the posterior elements. A CT scan often
is necessary to delineate this pattern. Type I and IA injuries (without
neurologic deficit) can be treated with immobilization in a cervical
orthosis. -
Type II
injuries are characterized by translation greater than 3 mm and
significant angulation at the fracture site. The anterosuperior portion
of the C3 body can show some compression. The pars fracture line is
usually vertical, close to the body-pedicle junction in the coronal
plane. The anterior longitudinal ligament is stripped off the superior
one third to one half of the front of the C3 body, but it is still in
continuity. The mechanism of injury is one of an initial hyperextension
and axial loading followed by hyperflexion. Disruption of the C2-3 disc
often occurs. Traction reduction followed by halo immobilization is the
usual treatment. Type IIA fractures have
significant angular deformity but only minimal translation. Angulation
can exceed 15 degrees, whereas translation rarely exceeds 2 or 3 mm.
Type IIA injuries most commonly are a result of flexion/distraction
injury resulting in failure of the neural arch in tension with rupture
of the posterior aspects of the disc. Traction is contraindicated in
this injury and would result in an increase in deformity and widening
of the disc space. Type IIA injuries should be reduced with extension
and compression. Image intensification may be helpful during halo
positioning. -
Type III
fractures have facet dislocations at C2-3 in addition to a displaced
pars fracture. The mechanism of injury is flexion and distraction
followed by hyperextension. They have a higher rate of neurologic
injury. The distinguishing feature is the free-floating inferior facets
of C2. It usually requires open reduction of the facet dislocation and
posterior C2-3 fusion.
for fractures and dislocations of the lower cervical spine does not
exist, classifications based on mechanism of injury generally have been
found useful. Allen et al’s classification is one of the most widely
used. It is based on a retrospective evaluation of 165 cases. The
authors proposed six categories, each named for the presumed position
of the cervical spine at the moment of injury and the initial principal
mechanism of load to failure. Categories include the following:
-
Vertical compression
-
Compressive flexion
-
Distractive flexion
-
Lateral flexion
-
Compressive extension
-
Distractive extension
motor vehicle accidents, diving injuries, and blows to the vertex of
the skull. Vertical compression stage 1 injuries have central cupping
of one vertebral end plate. Vertical compression stage 2 has disruption
of both end plates. Stage 1 injuries often are treated with a rigid
cervical or cervicothoracic orthosis. Vertical compression stage 2
injuries without neurologic injury can be treated with halo vest
immobilization for 8 to 12 weeks. Vertical compression stage 3 injuries
show fragmentation of the vertebral body with displacement of the
fragments peripherally into the canal (burst fracture). In the setting
of neurologic injury, most surgeons favor anterior corpectomy to
decompress the spinal cord followed by strut fusion and instrumentation
to reestablish anterior column integrity. Posterior instrumentation and
fusion may be added.
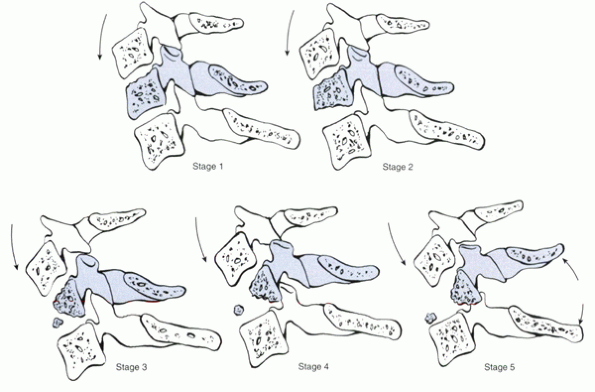
-
Stage 1 consists of blunting at the anterosuperior margin of the vertebral body.
-
Stage 2 has
further loss of anterior height, producing a beaklike appearance
anteroinferiorly. Rigid collar immobilization is usually sufficient to
allow healing and prevent development of late deformity. -
Stage 3
results from greater force application, producing a fracture line
passing from the anterior surface obliquely to the subchondral plate
(the so-called “teardrop fragment”). These often can be managed
successfully in a halo vest if minimally displaced or minimally
kyphotic. -
Stage 4 has a similar fracture pattern accompanied by less than 3 mm of displacement of the posterior body into the canal.
-
Stage 5 is characterized by more severe displacement and failure of the posterior ligamentous complex.
with instrumentation (with or without possible adjuvant posterior
arthrodesis) (Fig. 4-4). Biomechanical studies
of anterior plating (without structural bone graft) led to concern
regarding the adequacy of anterior surgery alone for this injury.
Clinical data of anterior structural grafting with a rigid plate have
shown good results, however, even without postoperative halo
immobilization.
subaxial cervical injuries. The distractive flexion stages include the
following:
-
Stage 2 is a unilateral facet dislocation that may be associated with a fracture of the articular process or pedicle.
-
Stage 3 is a bilateral facet dislocation, which usually shows 50% anterior displacement.
-
Stage 4 is a bilateral facet dislocation with full width (100%) vertebral body displacement.
 |
|
Figure 4-3
Compressive flexion injuries. Stage 1—blunting of anterosuperior vertebral margin. Stage 2—additional loss of height, involvement of inferior end plate. Stage 3—oblique fracture from anterosuperior surface to subchondral plate. Stage 4—posterior displacement (<3 mm) into neural canal. Stage 5—further disruption of posterior ligamentous complex and posterior displacement of vertebral body (>3 mm). |
bilateral facet dislocation in that the former shows less than 25%
translation of the vertebral body. The incidence of complete neurologic
injury is more frequent with bilateral facet dislocation. Some authors
recommend routine prere-duction MRI to identify concomitant herniated
nucleus pulposus because of the risk of disc fragment displacement
during a reduction. The clearest indication for prereduction MRI is in
the situation of an intubated and anesthetized patient; awake and
cooperative patients have been reduced safely by closed means.
Reduction usually is achieved by sequential addition of increasing
weights to cervical tongs until the facets are perched, followed by
careful manipulation. Many times, the facets reduce spontaneously with
sufficient weight. Definitive stabilization and fusion is required.
Posterior instrumented fusion and anterior discectomy and interbody
fusion with a plate may be successful for definitive treatment (Fig. 4-5).
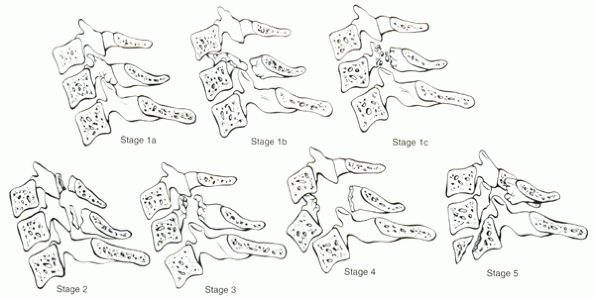
-
Stage 1
lesions involve a unilateral posterior arch fracture, usually
accompanied by failure of the anterior portion of the disc in tension (Fig. 4-6).
The posterior element fracture may consist of a linear fracture through
the articular pillar, an ipsilateral pedicle and laminar fracture
resulting in the “horizontal facet” appearance (Fig. 4-7),
or a combination of an ipsilateral articular process and pedicle
fracture (i.e., lateral mass fracture). Rotational instability around
the contralateral intact lateral mass may result. Retrospective data on
patients treated in either a hard collar or a halo brace have shown
P.41that
such management was frequently unsuccessful. Posterior surgery
traditionally has been advocated. Alternatively, anterior discectomy
and plated interbody fusion also seems to be effective and may lead to
better radiographic results (i.e., maintenance of kyphosis correction). -
Stage 2
lesions involve bilaminar fractures without evidence of failure of
anterior constraints. Multiple contiguous levels often are involved.
Neurologic injuries are unusual with this injury. Immobilization in a
rigid cervical orthosis or halo vest usually is sufficient. -
Stages 3, 4, and 5
lesions involve progressively severe circumferential disruption, with
stage 5 characterized by vertebral arch fractures and 100% anterior
displacement of the vertebral body. These are true
fracture-dislocations. Given the extreme disruption of both columns,
combined anterior and posterior fusion with instrumentation is the best
approach to surgical management.
 |
|
Figure 4-4 (A) Lateral radiograph of a patient with a compressive flexion injury involving C5. (B)
Sagittal reconstruction showing posterior displacement of vertebral body into the neural canal, which resulted in spinal cord injury. (C) Lateral radiograph after anterior decompression and circumferential stabilization. |
 |
|
Figure 4-5 (A) Lateral radiograph of a patient with a distractive flexion injury at C4-5. (B) MRI was performed before reduction because the patient had a concomitant head injury with altered consciousness. (C) Lateral radiograph after posterior fusion.
|
 |
|
Figure 4-6
Compressive extension injuries. Stage 1 involves unilateral fracture through the articular process, pedicle, or lamina. Stage 2 involves bilaminar fracture, which often occurs at multiple contiguous levels. Stages 3 and 4 are hypothetical stages, not seen in Allen’s initial observations. Stage 5 involves three contiguous levels, anterior displacement, and shear injury through the adjacent inferior centrum. |
 |
|
Figure 4-7 CT scan of a patient with ipsilateral pedicle and lamina fracture resulting in a “floating facet.”
|
-
Stage 1
lesions involve failure of the anterior ligamentous complex (anterior
longitudinal ligament and intervertebral disc) or a transverse failure
through the bony centrum. In the stage 1 lesion, there is no
translation or posterior displacement. Lesions that involve largely
bony injury may be managed best in a halo vest. Conversely, operative
treatment and nonoperative treatment have been recommended for stage 1
lesions that involve only soft tissues. This category represents a
spectrum of injuries that involve disruption of the anterior restraints
from the anterior anulus and longitudinal ligament to the posterior
anulus and posterior longitudinal ligament. If an initial nonsurgical
route is chosen, immobilization in either a rigid orthosis or a halo
should be accompanied by frequent serial radiographic follow-up. If
surgical treatment is elected, either primarily or after failed
nonoperative treatment, anterior reconstruction with a plate acting as
a tension band can be effective. -
Stage 2
lesions, in addition to the features seen in stage 1, involve failure
of the posterior ligamentous complex. The resultant instability may
allow displacement of the upper vertebral body posteriorly into the
spinal canal. Because these injuries involve disruption of the anterior
and the posterior columns, circumferential stabilization procedures may
ensure better long-term stability. Consideration
P.44may
be given to approaching the spine posteriorly initially to align the
spine in the sagittal plane adequately before anterior column
reconstruction. Many of these injuries occur in patients with
ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis. The
reduced capacity of the brittle spine to accommodate substantial
distraction/extension force vectors may be responsible for this
association.
injuries comprise ipsilateral fractures of the centrum and posterior
arch. Often CT scans are necessary to identify the posterior arch
fracture, which may be in the pedicle, lamina, or articular processes.
External immobilization may be adequate for most stage 1 injuries, if
the articular process injury is not one that is predisposed to
rotational instability (see under Compressive Extension). Stage 2
injuries result in fracture of the vertebral body with contralateral
bony or ligamentous failure in tension. These injuries usually require
traction for reduction and operative stabilization.
patients in all age groups. Careful clinical evaluation and judicious
use of imaging studies identify the spinal injury pattern and
associated neurologic deficits. The upper cervical spine has a unique
anatomy that leads to discrete injury patterns. Classifying subaxial
cervical injuries by their mechanism of injury may be helpful in
outlining operative and nonoperative treatment strategies.
M, Mohler J, Zach G, Morscher E. Indication, surgical technique and
results of 100 surgically treated fractures and fracture dislocations
of the cervical spine. Clin Orthop 1986;203:244-257.
JW, Cochran GVB, Lawsing JF, et al. Tears of the transverse ligament of
the atlas. J Bone Joint Surg Am 1974;56:1683-1691.
TA, Eismont FJ, Roberti LJ. Anterior decompression, structural bone
grafting, and Caspar stabilization for unstable cervical spine
fractures and/or dislocations. Spine 1992;17(10 Suppl):S431-435.
CH, Rock MG, Hawkins AJ, Bourne RB. Unilateral facet dislocation of the
cervical spine: an analysis of the results of treatment in 26 patients.
Spine 1987;12:23-27.
DM, Flanders AE, Osterholm J, et al. Prognostic significance of
magnetic resonance imaging in the acute phase of cervical spine injury.
J Neurosurg 1992;76:218-223.
