Anterior Instability of the Shoulder
the human body. With 6 degrees of freedom, the shoulder has the unique
ability of positioning the hand in space and gives us the mobility of
performing many tasks, from activities of daily living to high-end
sports activities. The shoulder needs normal “laxity” to function.
Laxity refers to the translation of the humerus within the glenoid
fossa. Many individuals are extremely lax on physical examination but
are asymptomatic in terms of shoulder complaints. It is when this
laxity causes abnormal shoulder function that we refer to instability
of the shoulder. Therefore, laxity does not equate to instability, and
instability refers to the symptomatic complaint of instability and dysfunction.
reported incidence is difficult to estimate because of the large range
in variability of presentation. Instability should be viewed as a
spectrum of pathology from unidirectional traumatic instability on one
end of the spectrum to atraumatic multidirectional instability at the
other end. The three basic categories of instability are traumatic,
acquired, and atraumatic.
-
Anterior instability
usually results from a fall with the arm in an abducted and externally
rotated position or an anterior force with the arm in abduction and
external rotation (i.e., arm tackling in football, falling while
skiing). -
Posterior instability
results from a posteriorly directed force with the arm forward elevated
and adducted (motor vehicle accident or pass blocking in football). A
grand mal seizure or electrical shock can also produce a traumatic
posterior dislocation.
subtle and is associated with pain in a throwing athlete or associated
with rotator cuff tendinosis/dysfunction. The instability can occur
from repetitive stretching of the shoulder ligaments from activity or
sports requirements.
patients have symptomatic glenohumeral subluxation or dislocations in
more than one direction. Many patients will present with severe pain as
an initial complaint and not overt instability. For treatment purposes,
it is important to differentiate atraumatic multidirectional
instability by the primary direction of instability.
-
Primary anterior: pain associated with the arm in an abducted, externally rotated position.
-
Primary posterior: pain when pushing open a heavy door.
-
Primary inferior: pain associated with carrying heavy objects at the side.
-
Degree of instability—Patients
can complain of the feeling of apprehension about the shoulder,
subluxation episodes, or full dislocation of the shoulder. -
Chronology of instability—It
is important to elucidate in the medical history of the patient
complaining of shoulder instability whether the instability is
congenital, acute (usually less than 3 weeks from injury), chronic
(usually more than 3 weeks from injury), recurrent, or some
combination. The importance of this classification system relates to
the treatment options available to the patient. -
Direction of instability—anterior, posterior, inferior, and superior.
lesions that are observed in patients with traumatic anterior
instability will facilitate repair of these lesions, which is essential
for a successful clinical outcome.
passive and active mechanisms. Passive or static factors include joint
conformity, adhesion/cohesion, finite joint volume, and ligamentous
restraints, including the labrum. The ligaments and capsule are aided
by receptors that provide proprioceptive feedback. When
capsuloligamentous structures are damaged, alterations in
proprioception occur that are partially restored with operative repair.
Static stabilizers are also affected by congenital factors that include
glenoid hypoplasia and disorders of collagen structure that result in
excessive joint laxity. The active mechanisms involved with
glenohumeral stability are primarily provided by the rotator cuff
muscles. The severity of the instability pattern may be influenced by
patient age, seizure disorder, and psychological or secondary gain
factors.
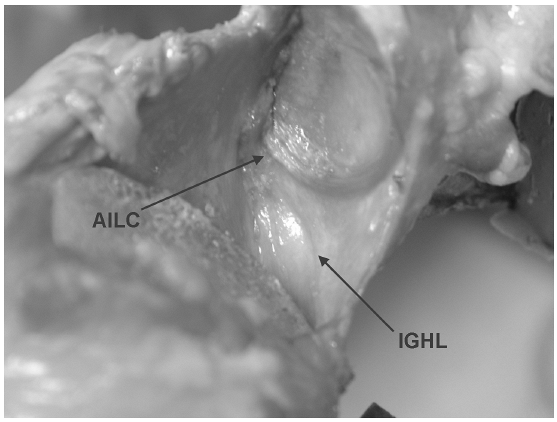
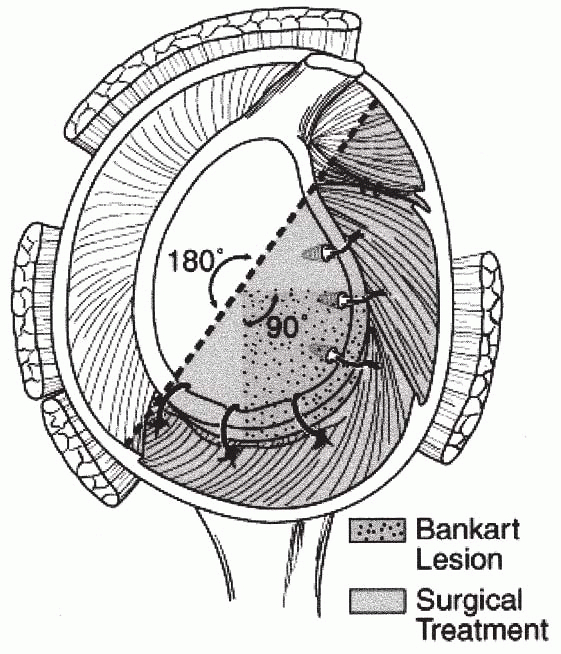
primary ligamentous restraint to anterior glenohumeral translation,
specifically with the arm in an abducted and externally rotated
position (Fig. 17-1). The specific anatomy of
the IGHL has been described as having anterior and posterior bands with
an intervening axillary pouch. Detachment of the anterior-inferior
labrum and capsule (comprising the anterior band of the IGHL as a
capsulolabral complex) is considered one of the major pathoanatomical
features of traumatic anterior shoulder instability. In fact, up to 85%
of traumatic anterior shoulder dislocations can be associated with
detachment of the anterior-inferior labrum and capsule. Broca and
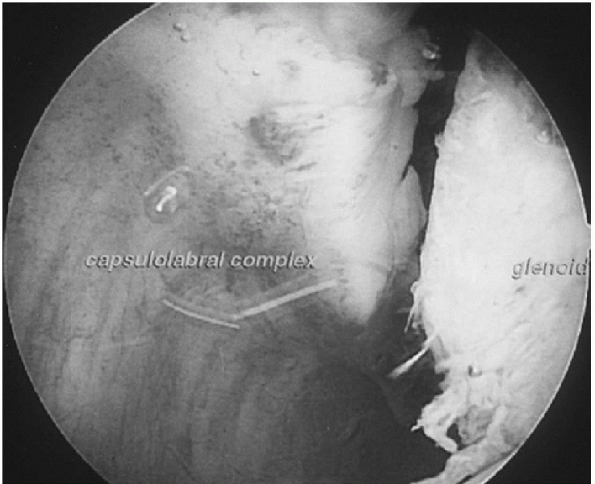
Hartman first described the lesion in 1890, followed by Perthes in 1906, and Bankart in 1923. This lesion has subsequently been named the Perthes-Bankart lesion (Fig. 17-2).
 |
|
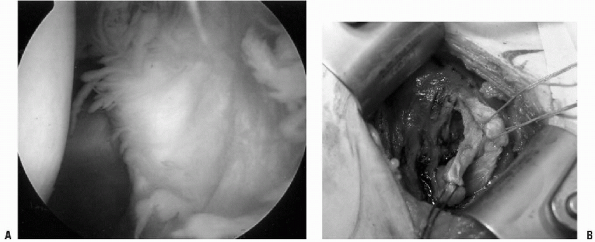
Figure 17-1 Cadaveric image of the inferior glenoid humeral ligament (IGHL) and anterior-inferior labral complex (AILC).
|
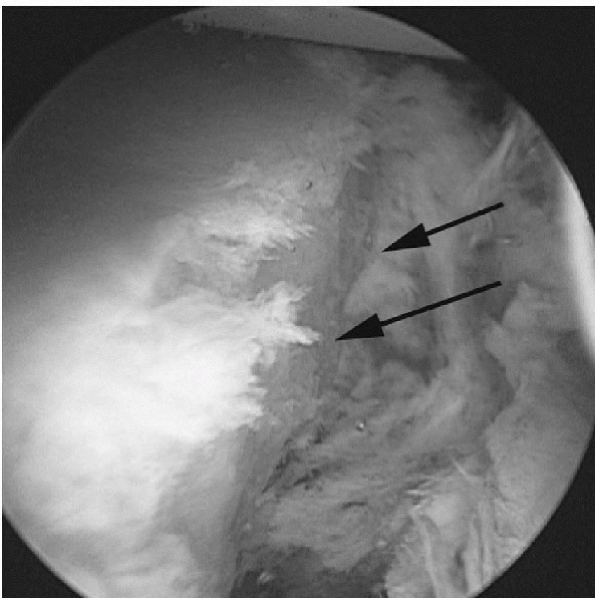
instability has been studied extensively. The detachment of the labrum
from the anterior-inferior glenoid is the essential lesion leading to
anterior instability. By displacing the anterior labrum, glenoid depth
is decreased by up to 50% and
passive restraints, such as the concavity-compression mechanism discussed earlier, are also lost.
 |
|
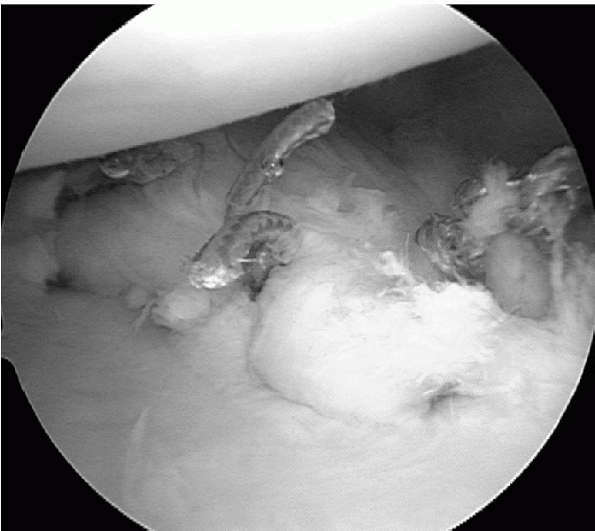
Figure 17-2 Arthroscopic view of a Bankart lesion, left shoulder, sitting position viewed from posteriorly.
|
 |
|
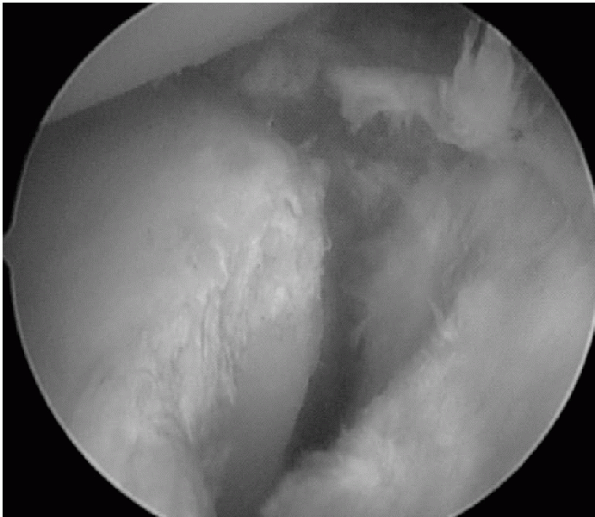
Figure 17-3
Arthroscopic view of an anterior labrum periosteal sleeve avulsion lesion. Anterior view of the left shoulder with the lesion being mobilized. |
from the glenoid has been shown to nearly double anterior translation.
Performance of Bankart repair, repairing the anterior IGHL and labrum
back to the glenoid, restores glenohumeral stability. Plastic
deformation of the capsule is a fundamental component of anterior
instability. This is an important concept in treatment of anterior
instability, because in addition to repair of the glenoid labrum, a
capsular plication must be performed.
type of pathology seen with anterior dislocations. IGHL detachment
tends to occur in young shoulders, and the capsular ligaments tend to
tear in the older ones. Avulsion of the anterior glenoid labrum has
been found in 100% of young patients and 75% of those older than 50.
Associated fractures, tears of the rotator cuff, and capsular injuries
are more common in those patients more than 50 years of age. Literature
states a 30% incidence of rotator cuff tears in patients greater than
40 years old, increasing to 80% in patients greater than 60 years old
with associated anterior dislocation.
 |
|
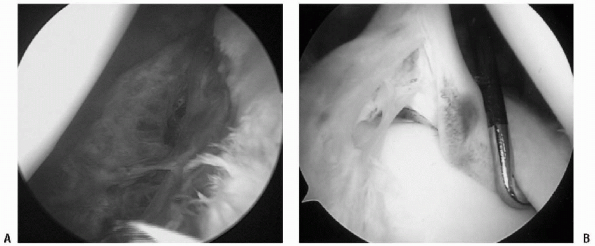
Figure 17-4 A: Arthroscopic capsular repair. B: Sitting position, left shoulder, viewed from posterior. Arthroscopic SLAP lesion, type IV.
|
lesion and an anterior labral ligamentous periosteal sleeve avulsion
lesion (ALPSA) (Fig. 17-3). In both acute and
chronic anterior dislocations, the anterior scapular periosteum does
not rupture as in a Bankart lesion, but the anterior IGHL, labrum, and
the anterior scapular periosteum are stripped and displaced in a
sleeve-type fashion medially on the glenoid neck. This is an important
diagnostic variant to recognize because in a chronic situation, a
cursory inspection of the anterior-inferior quadrant of the glenoid may
not reveal evidence of trauma. However, closer inspection more medially
will show a large, medially displaced scarred labrum on the anterior
portion of the glenoid neck.
observations of additional lesions associated with anterior
instability. Occasionally, the injury may extend inferiorly into the
capsule or the axillary pouch (Fig. 17-4A).
Injuries may also extend superiorly into the attachment of the biceps
tendon, producing a concomitant superior labrum anterior-posterior
(SLAP) lesion (Fig. 17-4B). This lesion is generally observed when the dislocation involves an extreme type of trauma.
the anterior supraspinatus can have partial or complete tears resulting
in various amounts of instability. This has been called the superior
labrum, anterior cuff (SLAC) lesion. This can be caused by both acute
and chronic trauma.
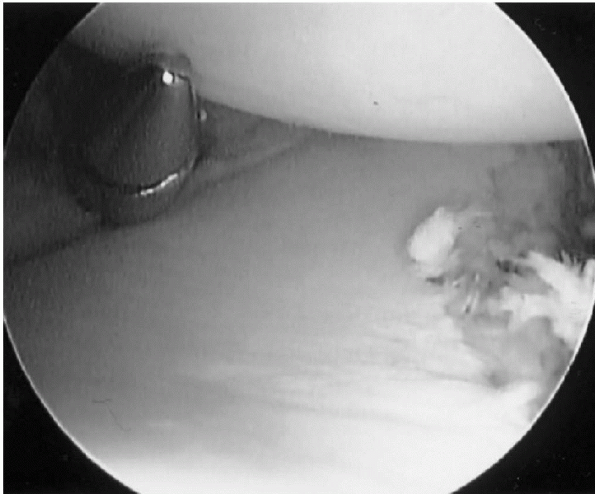
detachment of the IGHL from the humeral neck. This was subsequently
described as a humeral avulsion of glenohumeral ligament (HAGL) lesion (Fig. 17-5). Continued forced abduction
(i.e., a force started in abduction of 90 to 105 degrees) supplemented
by impaction tears the capsule from the neck of the humerus. Both open
and arthroscopic repair techniques have been described. In arthroscopic
repair, a standard anterior-inferior portal is made, and the bone at
the anterior-inferior aspect of the humeral neck is burred through this
portal. An anterior-lateral portal is created 2 cm lateral and 2 cm
inferior to the coracoid process. A suture hook is used to place
monofilament absorbable suture through the capsule, and these are tied
through the anterior-lateral portal over the subscapularis tendon.
Although relatively rare, this lesion must be sought on any anterior
instability arthroscopic examination. HAGL lesions have also been seen
after acute anterior dislocations.
 |
|
Figure 17-5 A:
Arthroscopic view of a humeral avulsion glenohumeral ligament lesion (HAGL), sitting position, posterior left shoulder. The subscapularis muscle is seen as a shadowed area in the background. B: Open example of HAGL lesion, right shoulder. The subscapularis is tagged with a suture to the right. The HAGL lesion is tagged with sutures inferiorly. |
The anatomy of the glenoid and proximal humerus is consistent. The
articular surface of the proximal humerus is similar to that of a
sphere. It is composed of cartilage and subchondral and trabecular bone
that is relatively soft, even in young athletes. The glenoid has a
consistent morphology as well. It is pear-shaped with the inferior
portion approximating that of a true circle. The average
superior/inferior glenoid diameter range is 30.4 to 42.6 mm in males
and 29.4 to 37.0 mm in females. Bony lesions of the glenoid or humeral
head place greater demand on the integrity of soft-tissue repairs and
have been shown to cause recurrent anterior instability of the shoulder.
 |
|
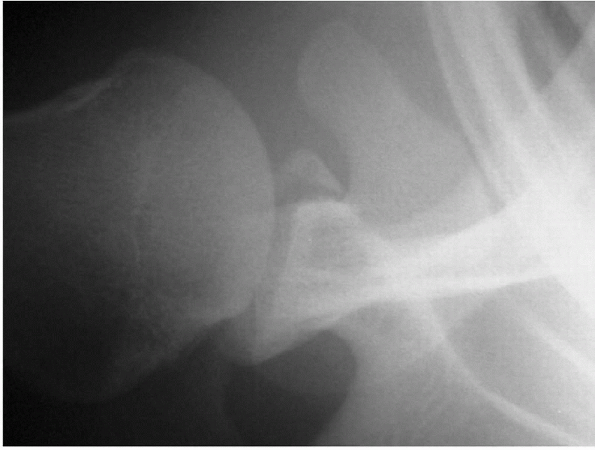
Figure 17-6 Radiograph of a bony Bankart lesion.
|
impression fracture caused by the humeral head being dislocated
anteriorly and impacting on the anterior glenoid. This is generally
located at the posterior-superior portion of the humeral head. An
“engaging” Hill-Sachs lesion, which catches and locks the humeral head
in a functional position of abduction and external rotation, has also
been reported. The long axis of the Hill-Sachs lesion is parallel to
the glenoid and engages its anterior corner. A nonengaging Hill-Sachs
lesion is when the impression fracture from the anterior dislocation
catches and locks the humeral head with the arm in a nonfunctional
position (i.e., shoulder abduction of less than 70 degrees). The
nonengaging Hill-Sachs lesion passes diagonally across the anterior
glenoid with external rotation so there is continual contact between
the articular surfaces. These shoulders are reasonable candidates for
arthroscopic Bankart repair. It is important to realize, however, that
the Hill-Sachs lesion is created by the position of the arm when the
dislocation occurs. A Hill-Sachs lesion that develops with the arm at
the side with some extension of the shoulder will be located more
vertically and superiorly than the lesion that occurs with the shoulder
abducted and externally rotated. The Hill-Sachs lesion that develops
with the arm at the side is generally a nonengaging lesion.
Hill-Sachs lesion. The first is an open capsular shift procedure that
restricts external rotation, thus not allowing the lesion to engage.
The second approach, which is reserved for large defects of the humeral
head, is filling the impression fracture with a size-matched humeral
osteoarticular allograft. The third is a proximal rotational humeral
osteotomy that internally rotates the articular surface of the humerus
and effectively prevents the impression fracture from engaging the
glenoid rim.
anterior-inferior glenoid: the impression fracture or the avulsion
fracture. The compression Bankart lesion is secondary to compression of
the anterior-inferior bony articulation of the glenoid by the humeral
head. Repeated episodes of instability create the “inverted pear”
lesion, as well as a typical bony Bankart. Investigators in the past
have recommended a coracoid transfer if the glenoid rim fracture
comprised 25% of the anterior-posterior diameter of the glenoid. Burkhart et al. (2002)
described the containment of the humeral head by the glenoid as a
result of two geometric variables: (a) the deepening effect of a wire
glenoid due to the longer arc of its concave surface and (b) the arc
length of the glenoid itself. They caution that if the bony fragment is
excised or if there is an inverted pear-shaped glenoid, arthroscopic
techniques without a bone augmentation procedure may be predisposed to
failure (Fig. 17-7).
the arthroscope in the anterior-superior portal, looking inferiorly at
the glenoid. The bare spot of the glenoid is roughly in the center of
the glenoid and with a calibrated probe, the distance from the anterior
rim of the glenoid to the bare spot is measured, as well as the
distance from the bare spot to the posterior glenoid rim. A bone
augmentation procedure is indicated when there is a 25% reduction in
the length from the anterior glenoid to the bare spot compared with the
posterior glenoid to the bare spot.
 |
|
Figure 17-7
Arthroscopic example of an inverted pear-shaped glenoid. Left shoulder, anterior-superior viewing portal, lateral posterior. Note the bony deficiencies of the anterior-inferior glenoid to the right. |
shoulder instability in the general population to be approximately
1.7%. After an anterior shoulder dislocation, the risk of recurrent
shoulder instability has been related to the following factors:
-
Age at primary dislocation—There
is a significantly higher rate of recurrent anterior shoulder
instability in younger patients with acute traumatic anterior shoulder
dislocations. The majority of the recurrent instability episodes occur
in the first 2 years after the primary incident. -
Number of anterior shoulder instability recurrences, with a positive correlation between a higher number of recurrences and an increased risk of instability.
-
Future athletic participation—For
first-time contact sport athletes, an 80% recurrence rate was seen with
conservative treatment and return to contact sport. On the other hand,
there was a 16% recurrence rate with arthroscopic treatment of the
Bankart lesion and return to contact sport. -
Bone loss (glenoid or Hill-Sachs lesion).
not been found to be related to the type and duration of
immobilization. One long-term (10-year follow-up) study on
immobilization outcomes after anterior shoulder dislocations found no
effect on recurrence rates related to the length of immobilization. Of
the primary anterior shoulder dislocators, 50% had a recurrent
dislocation at 10 years out. Of the recurrent dislocators, 50% had
surgery, and of those with surgery, 50% were stable at 10-year
follow-up. Interestingly, degenerative joint disease was found in both
surgical and nonsurgical candidates, with 11% of the patients who
underwent surgery having mild secondary degenerative joint disease at
the 10-year follow-up.
-
A comprehensive evaluation of anterior
shoulder instability should start with a focused but detailed history
of the instability episode. -
The onset, circumstances, direction of
dislocation, frequency of dislocations/subluxations, and magnitude of
the instability episodes should be delineated. -
The patient should be asked about the
location of the shoulder pain because this will give clues with regard
to the type of pathology present.-
Pain at the anterior-lateral deltoid may represent supraspinatus tendon injury.
-
Pain at the posterior joint line may represent injury to the posterior labrum or infraspinatus pathology.
-
Anterior joint line pain or pain over the
coracoid points to a subscapularis tendon injury, a biceps tendon
injury, or a capsulolabral tear. -
Pain can also be referred from other
sites in the body and be perceived as shoulder pain. Referred areas of
pain to the shoulder that should be remembered include cervical
radiculopathy, cardiac ischemia or pericarditis, thoracic outlet
syndrome, and bone or soft-tissue tumors.
-
-
A thorough review of symptoms may reveal other medical conditions that manifest as shoulder pathology.
-
Patients with diabetes mellitus have an increased risk of frozen shoulder and infection.
-
Renal failure predisposes to avascular necrosis.
-
A significant alcohol or seizure history may point to a posterior shoulder dislocation.
-
-
Before physical examination, a
differential diagnosis of shoulder pathology should be formulated. The
differential diagnosis of traumatic injury to the shoulder can be
divided into three categories:-
Osseous lesions include clavicle
fractures, proximal humerus fractures, fracture dislocations of the
greater tuberosity, and scapular fractures (glenoid, coracoid, and
acromial). -
Soft-tissue lesions include contusions of
the deltoid or trapezius muscles (i.e., myositis ossificans),
acromioclavicular joint sprain, glenohumeral dislocations, and
traumatic rotator cuff tears (rare in athletes <35 years old). -
Nerve lesions include injury to the
axillary nerve, suprascapular nerve traction injury, and long thoracic
nerve injury. The axillary nerve has been found to be injured in
approximately 9% to 18% of anterior shoulder dislocations. The
sensation is usually preserved, and motor weakness must be sought for
the diagnosis. Injury to the long thoracic nerve causes scapular
winging from the weakened serratus anterior muscle.
-
-
The physical examination of the shoulder should follow a systematic approach to avoid missing concurrent pathology.
-
The shoulder should be inspected for
muscular atrophy or asymmetry from a posterior viewpoint. For example,
atrophy of the infraspinatus fossa may be secondary to disuse or
suprascapular neuropathy. -
The cervical spine should be palpated posteriorly for bony tenderness along the spinous processes.
-
Cervical range of motion should be noted,
and a neurovascular examination of the upper extremities should be
performed. Reflexes and long-tract signs should be evaluated when
necessary. -
Spurling’s test should be checked to rule out referred shoulder pain from cervical spinal nerve impingement.
-
-
All bony prominences about the shoulder should be palpated.
-
Coracoid or acromioclavicular joint tenderness should be noted in the initial physical examination.
-
The soft tissues about the shoulder should be palpated for tenderness.
-
Specific locations of pathology include
pain over the bicipital groove anteriorly (i.e., biceps tendon
pathology) and pain at the greater tuberosity area.
-
-
Overall ligamentous laxity should be sought in patients with shoulder instability complaints.
-
Thumb or finger hyperextension can be tested, and a sulcus sign might be seen.
-
Patients with ligamentous laxity have an increased risk of multidirectional instability.
-
-
Active and passive range of motion in all
scapular planes (forward flexion, extension, abduction, external
rotation with the arm at the side and in 90 degrees of abduction, and
internal rotation up the back and with the arm in 90 degrees of
abduction) should be recorded.-
Increased external rotation in the dominant shoulder may be a normal finding.
-
Loss of internal rotation may be secondary to a contracture of the posterior capsule/cuff.
-
-
Strength testing should include the
supraspinatus (empty beer can sign), infraspinatus (resisted external
rotation with the arm at the side), subscapularis (lift-off test),
trapezius/rhomboids (shoulder shrug), deltoid (resisted abduction with
arm at the side), and the serratus anterior (check for scapular
winging). -
One of the most important tests for documentation of anterior shoulder instability is the apprehension and relocation test (see Fig. 15-15 in Chapter 15).
-
The patient is told to lie supine with
the affected arm and shoulder hanging off the edge of the examining
table. The arm is brought into 90 degrees of abduction and slowly
externally rotated.-
With a positive test, the patient will experience pain or the feeling that the shoulder is about to dislocate.
-
-
In the second part of the examination, the relocation test (see Fig. 15-16 in Chapter 15), the examiner applies an anterior force to the proximal humerus (i.e., in an attempt to center the humeral head).
-
With a positive relocation test, the
patient either has a decrease in the anterior shoulder pain or a
decrease in the sense that the arm is about to dislocate.
-
-
-
Anterior to posterior translation of the humerus should also be documented using the load and shift test (see Fig. 15-20 in Chapter 15).
-
In the same position as the apprehension
test (supine with affected shoulder hanging off the side of the exam
table), the shoulder is abducted to 70 degrees, forward flexed to 45 to
50 degrees, and axially loaded so that a compressive force is applied
across the glenohumeral joint. The humeral head is then
P.220grasped
anteriorly and posteriorly by the examiner between the index and thumb,
and the humeral head is translated anteriorly and posteriorly. The
amount of translation is recorded and a grade assigned (Table 17-1).-
Patients with a grade 2+ or 3+ anterior
translation, compared with the contralateral normal extremity, are good
candidates for arthroscopic stabilization.
-
-
Posterior instability of the shoulder
should be examined by forward flexing the arm to 90 degrees, with
approximately 20 to 30 degrees of adduction. By applying a posteriorly
directed force to the arm, the posterior labrum and capsule are
stressed.-
Any pain with this maneuver alerts the surgeon to posterior capsular pathology.
-
-
-
With any examination for instability,
rotator interval lesions must be sought. The sulcus sign tests for
rotator interval pathology (see Fig. 15-17 in Chapter 17).-
With the patient in the seated or
standing position and the arm hanging at the side, a downward force is
applied to the arm. The amount of inferior translation that occurs is
documented in comparison with the contralateral extremity. The grading
system is given in Table 17-2.-
The sulcus sign should decrease with external rotation of the arm.
-
If there is a sulcus sign at neutral
rotation that persists in external rotation or if there is a >2+
sulcus with 2+ to 3+ anterior shoulder translation on the load and
shift test, there is an increased risk of a large rotator interval
lesion.
-
-
The biceps anchor should also be examined for a SLAP tear. This can be evaluated with O’Brien’s test (see Fig. 15-21 in Chapter 15).
-
A positive test reproduces the shoulder
pain with resistance of a downward force when the arm is forward flexed
to 90 degrees, adducted, and internally rotated. The pain is reduced
with resistance to a downward force with the arm forward flexed to 90
degrees, adducted, and externally rotated. -
A false-positive test may occur, however,
with acromioclavicular joint pathology because of the amount of
adduction that the arm is placed into for the test.
-
-
|
TABLE 17-1 GRADING SYSTEM FOR SHOULDER TRANSLATION
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||
|
TABLE 17-2 GRADING OF THE SULCUS SIGN
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||
-
Radiographic evaluation is required in
the assessment of shoulder instability. Shoulder anatomy, as well as
any fractures associated with the dislocations, is critical to document
before treatment and may significantly change the overall treatment
plan. -
A standard anterior-posterior view of the
arm in slight internal rotation is used to identify a fracture of the
greater tuberosity. -
A true scapular anterior-posterior radiograph permits evaluation of a glenoid fossa fracture, if present.
-
The West Point axillary view is used to
assess bony avulsions of the attachment of the IGHL, bony Bankart
lesions, or anterior-inferior glenoid deficiency. -
The Hill-Sachs lesion can be quantified and evaluated by examining the Stryker notch view.
-
A computed tomography (CT) scan can be an
accurate means of determining glenoid version and overall glenoid
morphology. It has the ability to reconstruct the anatomy of the
glenoid in three dimensions and it can also isolate the glenoid for
viewing by subtracting the humerus from the image. -
The shape of the articular surface can aid the surgeon in preoperative planning.
-
Substantial bone loss may be a contraindication to arthroscopic stabilization.
-
Magnetic resonance imaging (MRI) is used for assessment of associated pathology.
-
Contrast enhancement improves the
diagnostic ability to detect labral tears (both superior and
anterior-inferior), rotator cuff tears (both partial and full
thickness), and articular cartilage lesions. -
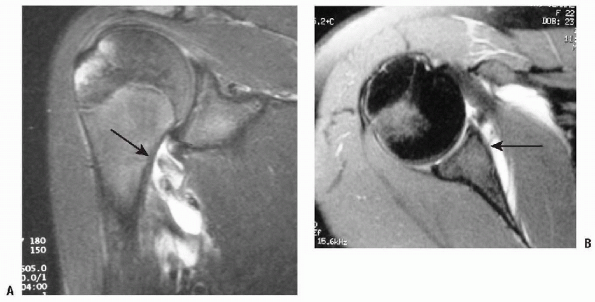
In identification of HAGL lesions, MRI in
the midsagittal coronal oblique plane shows the detachment of the
inferior glenoid labrum (IGL) and that the axillary pouch is converted
from a full distended U-shaped structure to a J-shaped structure, as
the IGL drops inferiorly (Fig. 17-8).P.221-
The appearance of a HAGL lesion with MRI
has been described as an avulsion fracture from the neocortex in the
humeral neck. A thin radiolucency is observed inferior to the anatomic
neck of the humerus, and once again the fluid-filled distended U-shaped
axillary pouch is converted into a J-shaped structure by the
extravasation of contrast material. The presence of this lesion may
also be a relative contraindication to an arthroscopic shoulder
stabilization procedure.
-
-
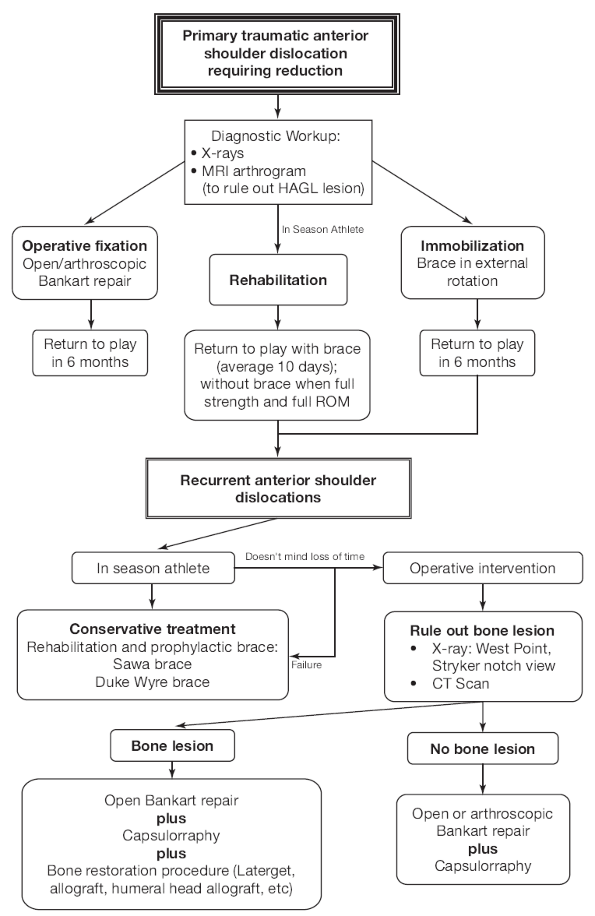
Algorithm 17-1 summarizes the diagnostic workup of shoulder instability.
 |
|
Figure 17-8 A: MRI example of the HAGL lesion. B: MRI example of a Bankart lesion.
|
techniques for anterior labral stabilization is almost 20 years old.
Both open and arthroscopic procedures have involved the use of bone
tunnels, staples, transglenoid sutures, rivets, bioabsorbable tacks,
and suture anchors. Initial studies reported recurrence rates of
arthroscopic techniques from 0% to 44%. Earlier arthroscopic techniques
with higher failure rates were attempted on many types of instability
patterns and used techniques that did not follow the principals of
established open methods.
shoulder instability is the ability to accurately identify and treat
the specific pathoanatomy found in the glenohumeral joint. Other
advantages of arthroscopic repair include less iatrogenic damage to
normal tissues (subscapularis), reduced postoperative pain, and
improved cosmesis. Easier functional recovery and improved range of
motion than with the open repair method have also been reported.
Decision making for arthroscopic versus open techniques can be
variable, depending on the surgeon’s experience. Ideal indications for
arthroscopic stabilization include a traumatic unidirectional
anterior
shoulder dislocation with a Bankart lesion, a first-time dislocator,
minimal sulcus sign, no generalized laxity, thick robust ligaments,
minimal plastic capsular deformation, and an exam under anesthesia
revealing a grade 2+ to 3+ pure anterior translation deformity.
 |
|
Algorithm 17-1 Diagnosis and management of anterior instability of the shoulder.
|
Hill-Sachs lesion involving greater than 20% to 30% of the articular
surface that engages the glenoid rim with the arm in a position of
abduction and external rotation, a bony abnormality such as an
“inverted pair” glenoid, or a glenoid rim defect >25% of the
articular surface. A multiple dislocator (i.e., greater than 5
dislocations or subluxations) is a relative contraindication to
arthroscopic repair. Some surgeons still advocate an open procedure in
high-demand athletes. An argument can be made that as arthroscopic
techniques continue to improve and closely mimic what is done in open
procedures, arthroscopic recurrence rates will equal or surpass those
of open procedures.
This involves an inferior capsular plication, an anterior shift, a
Bankart lesion repair with suture anchors, and a rotator interval
closure. In operative treatment of an acute anterior dislocation within
3 weeks, only the Bankart lesion or the anterior-inferior glenoid
labrum tear is repaired with suture anchors. The inferior capsular
plication and rotator interval closure are reserved for the late repair
of a recurrent dislocator.
dislocation), capsular imbrication and rotator interval closure will be
required, because it is thought that there is capsular plastic
deformation associated with the repetitive microtrauma of subluxation.
With any type of capsular failure, there is a significant amount of
elongation, suggesting that plastic deformation of the capsule has
occurred. Therefore, some type of capsular shortening is required to
return the capsule to its anatomic configuration.
 |
|
Figure 17-9
Illustration of a surgical reconstruction with an 180-degree arthroscopic repair with three inferior plication sutures, three anchors repairing the labrum, and a rotator interval closure. |
-
The beach chair or lateral decubitus position can be used for instability surgery.
-
The beach chair position offers the
advantage of being able to convert to an open procedure easily. When
the beach chair position is used, a sterile arm holder is helpful for
both holding a desired arm position and for applying a distraction
force to the arm. -
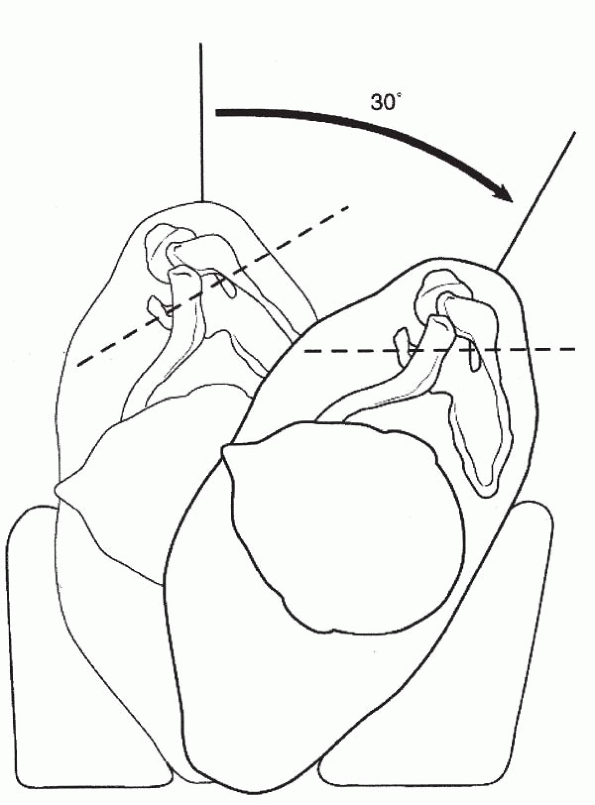
For the lateral decubitus position, a
three-point distraction device is used that allows both longitudinal
and vertical traction and enables the humeral head to be lifted
reproducibly from the glenoid (Fig. 17-10). A
beanbag is used to stabilize the patient, with a hip-holder also used
just below the scapula posteriorly to stabilize the beanbag, in case
air is accidentally liberated. The patient is positioned in a 30-degree
backward tilt, which places the glenoid in a parallel orientation to
the floor.
-
-
In most cases, general endotracheal intubation is used for anesthesia with an interscalene block for pain control.
-
Preoperative antibiotics are administered intravenously before skin incision.
-
An examination under anesthesia of both
shoulders in the supine position is performed documenting forward
elevation, external and internal rotation with the arm at the side, as
well as external and internal rotation with the arm abducted to 90
degrees.-
The examination under anesthesia is used to confirm and add further information and/or other pathology that may be present, not to make the diagnosis.
-
An anterior load and shift, a posterior
“jerk” test, and a sulcus test are performed to assess instability.
When performing the load and shift test, care should be taken to
compare both shoulders for the amount of humeral head translation. -
The amount of translation should be noted
for each arm position with respect to the degree of humeral rotation
and the position of the arm in relation to the plane of the scapula.
Arm rotation and position will influence the degree of translation
because of the changes that they have on ligament length.
-
-
A standard posterior portal should be
placed slightly more laterally than the joint line. If the portal is
placed medial to the joint line, this will require the surgeon to lever
the arthroscope against the glenoid, making the stabilization procedure
quite difficult.-
An 8- to 10-mm incision is made, and the
blunt arthroscope sheath and trocar are inserted atraumatically into
the space between the glenoid rim and humeral head.
-
-
The anterior series of portals are then made using spinal needles for localization.
-
The first anterior portal made is
superior and lateral in the rotator interval, as high in the
anterior-superior quadrant of the shoulder as possible, while still
allowing the cannula to be placed anterior to the biceps tendon. Medial
placement of the cannula will compromise access to the glenoid. Care
should be taken to prevent placement of the cannula posterior to the
biceps tendon to avoid entrapment of the tendon with sutures. In
general, a 7 mm × 7 cm cannula, smooth or ridged, is placed for suture
shuttling. -
The second portal is the
anterior-inferior portal; because of the instruments used through this
portal, it is usually an 8.25 mm × 7 cm cannula. Two different portal
types can be made.-
The first type is a transsubscapular
portal at the 5 o’clock position. Although this allows accurate and
easy anterior-inferior anchor placement, it can be difficult to place
because it is going through subscapularis tendon. In this case, to
accomplish this as atraumatically as possible, a pointed switching
stick is used to pierce the subscapularis tendon first, followed by a
dilator system. -
The second type of anterior-inferior
portal is made at the superior rolled edge of the subscapularis and
angled inferiorly. Once again, this is also made with spinal needle
localization but avoids the trauma of going through the subscapularis
tendon. Potential difficulties with this portal placement involve
inferior anchor placement because the angle for placing the anchor is
more oblique. To overcome this, a stab incision can be made at the 5
o’clock position and the anchor placed through the subscapularis tendon
without a cannula. The sutures from the anchor are then shuttled
through the anterior-inferior cannula located above the rolled edge of
the subscapularis.
-
-
The final portal that is made is the 7
o’clock portal. This is a posterior-inferior portal, allowing inferior
capsular plication. This portal is made roughly 2 cm lateral and 1 cm
inferior to the standard posterior portal. An 18-gauge spinal needle is
used under direct visualization to assess the position, and an 8.25 mm
× 9 cm cannula is then placed. This portal allows a very accurate
inferior capsular plication under direct visualization, because the
arthroscope is kept in the posterior portal, and suture shuttling
devices are used and placed through the large 7 o’clock cannula (Fig. 17-11).
-
-
Care should be exercised in creating portals and in evaluating pump pressure.
-
Shoulder overdistention is compounded by improper portal development and a lengthy procedure.
-
It is important always to establish
accurate and small portals, to use cannulas at all times to create a
seal in the glenohumeral joint, and to monitor the amount of fluid
pressure to decrease the amount of fluid extravasation. An ideal
pressure to perform arthroscopic stabilization has not been reported.
However, analysis and evaluation of pressure and
P.224shoulder distension as the procedure progresses are critical.
-
 |
|
Figure 17-10 Positioning of the patient with the lateral traction device and a 30-degree posterior tilt.
|
 |
|
Figure 17-11 Portals that can be used for the “180-degree” repair technique.
|
-
Preparation of the capsule before
plication has been advocated to “excite the synoviocytes.” This has not
been scientifically proven but makes logical sense and can be
accomplished with either a shaver or a hand-held burr from the anterior
or poster inferior (7 o’clock position) portals. -
Preparation of the glenoid bed for the
labrum is also critical. A sharp elevator combined with an arthroscopic
shaver or tissue ablation device is used to dissect and liberate the
entire labrum, IGHL, and periosteum of the glenoid neck off until the
subscapularis muscle is seen through this interval. -
The anterior-inferior labrum should be released so that it “floats” to the glenoid rim.
-
With the arthroscope in the posterior
portal, the soft tissue and cortical surface of the anterior glenoid
rim can be removed using a small burr to create a bleeding surface on
the anterior glenoid neck. -
To evaluate this preparation of the
glenoid bed, the arthroscope is placed in the anterior-superior or
anterior-inferior portal, allowing excellent visualization of the
labral complex and bone preparation (Fig. 17-12).
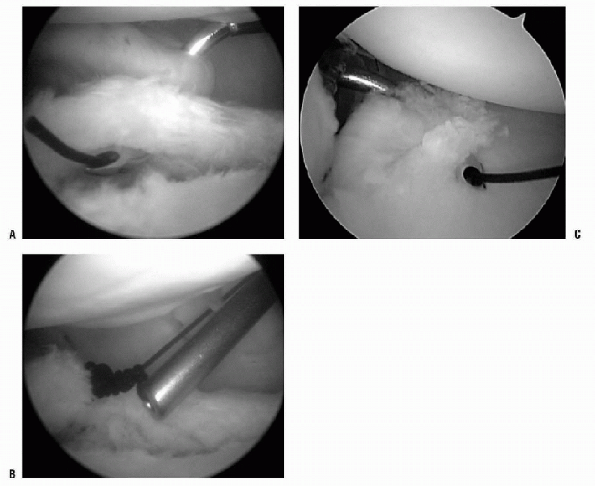
-
Inferior plication is accomplished by
imbricating the axillary pouch. As previously stated, capsular
plication (capsulorraphy) is necessary due to the irreversible plastic
deformation of the capsule that occurs during an anterior dislocation. -
Arthroscopically, the capsulorraphy can be completed with suture, suture anchors, or thermal energy.
-
There are multiple methods for
capsulorraphy. The pinch-tuck method involves a suture-passing device
in a “corkscrew configuration” that can penetrate the tissue
approximately 1 cm away from the labrum and then penetrate the labrum
itself (Fig. 17-13). When this knot is tied, it
creates a blind pouch that scars in. If the labrum is friable or an
adequate bite cannot be secured, a suture anchor can be placed into the
labrum. The suture can then be shuttled through the inferior capsule
and tied. Two to three of these inferior capsular plication sutures are
then placed from the posterior-inferior to the anterior-inferior
position (positions 8, 7, and 6 o’clock, respectively, on a right
shoulder). An accessory posterior portal can be used (7 o’clock portal)
or the camera can be changed to the anterior-superior portal and a
cannula placed in the posterior portal. -
Suture management at this stage is important.
-
The surgeon can tie each individual
suture sequentially after being placed, which makes suture management
more straightforward, but this can run the risk of “closing yourself
out.” -
The second method for suture management
involves shuttling the suture out the anterior cannula, removing the
cannula, and replacing it, thus removing the suture pair from within
and placing the suture pair on the outside of the cannula. All pairs
can then be shuttled back into the joint at the end of throwing all of
the plication stitches for tying.
-
-
Once two or three inferior capsular plication sutures are made, attention is turned to the anterior-inferior Bankart lesion.
 |
|
Figure 17-12
Arthroscopic example of anterior glenoid preparation, left shoulder, lateral position, viewed from the anterior-superior portal. |
-
Repair of the Bankart lesion is the critical step in this procedure.
-
The suture anchor repair is similar to the open repair technique and is extremely versatile and reproducible.
-
There are three variations of this
technique: the suture-first method, the anchor-first method, and the
Knotless Suture Anchor (Mitek, Inc., Norwood, MA) method. Clinically,
there have been no reported differences between any of these techniques
in the literature, and their use is based on surgeon preference. -
The anchors themselves can be either
metal or bioabsorbable. There are no differences reported clinically on
the basis of the material of the anchor.-
We recommend bioabsorbable anchors
because most instability patients are young, and we attempt to avoid
the theoretical possibility of migration.
-
-
Proper anchor placement is the most critical step, and no material can help an improperly placed anchor.
-
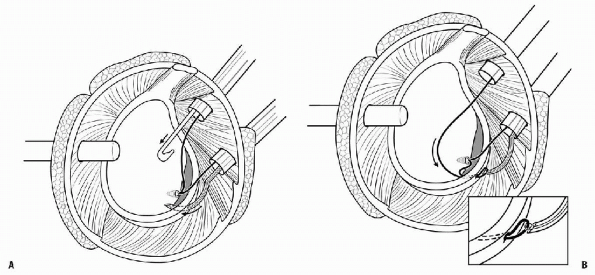
The anchor-first technique involves
placing an anchor through the anterior-inferior cannula first and then
shuttling the suture limb second (Fig. 17-14).
It is important to note at this time the position of the
anterior-inferior cannula and the position in which the anchor should
be placed into the glenoid. There are times when the position of the
cannula is appropriate for suture shuttling but not for placement of
the anchor. In this case, a percutaneous approach can be used to insert
an anchor into the glenoid at the 5:30 position.-
The advantage of this technique is a more
appropriate perpendicular placement of the anchor into the glenoid face
at approximately 2 to 3 mm over the articular service without
“bubbling” or causing articular damage.
-
-
After the anchor has been successfully
inserted, one of the suture limbs is passed out of the
anterior-superior cannula. This limb, if using a metal anchor or an
anchor with a fixed eyelet, is the limb on the tissue side of the
suture. The eyelet should be perpendicular to the labrum. A tissue
penetrator or suture shuttling device is used to place a passing suture
into the tissue inferior to the anchor. The end of the suture is then
grasped and pulled out the anterior-superior cannula. A small square
knot is tied in the passing suture, serving as a dilating knot. This is
followed by tying the nonabsorbable braided suture to the monofilament
suture line further distal and pulling the passing stitch through the
anterior-inferior cannula, hence shuttling the suture through labrum,
inferior-glenoid ligament, and scapular-periosteal complex. -
On tightening this suture with proper
arthroscopic knot-tying techniques, a shift of tissue from inferior to
superior should be observed. If the tissue bite was not placed inferior
enough to the anchor, then this step should be repeated before
continuing the operation. To tie the knot, the knot pusher is placed on
the suture limb that is on the tissue side. This will be the post. A
sliding or nonsliding (multiple half hitches) knot can be tied at this
time. It has been determined that after placement of a sliding knot or
multiple half hitches that three alternating half hitches, while
switching the post, are the most secure final fixation. The knot should
end up on the tissue side so that the labrum can create a bumper
effect. The next two or three anchors are then placed approximately 5
to 7 mm apart from each other in the same the fashion as previously
described. On completion of the procedure, a “bumper” should be
observed at the anterior-inferior glenoid between the 3 and 6 o’clock
positions.
 |
|
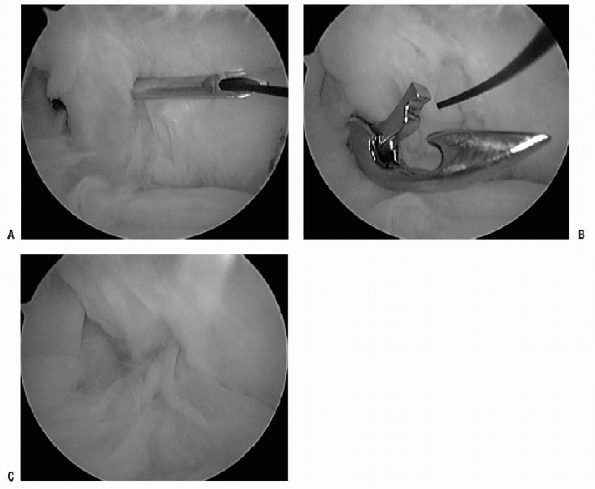
Figure 17-13 A: Suture-shuttling device demonstrating the pinch-tuck technique 1 cm from the labrum with an angled crescent hook. B: Suture has been shuttled for plication with monofilament suture. Nonabsorbable suture can be shuttled and tied for plication. C: Example of inferior plication from the posterior portal with viewing from the anterior-superior portal.
|
 |
|
Figure 17-14 A: Example of an anchor first shuttling technique with a tissue penetrator inferior to the anchor. B: Nonabsorbable suture shuttled through the inferior labrum and inferior glenohumeral ligament complex.
|
 |
|
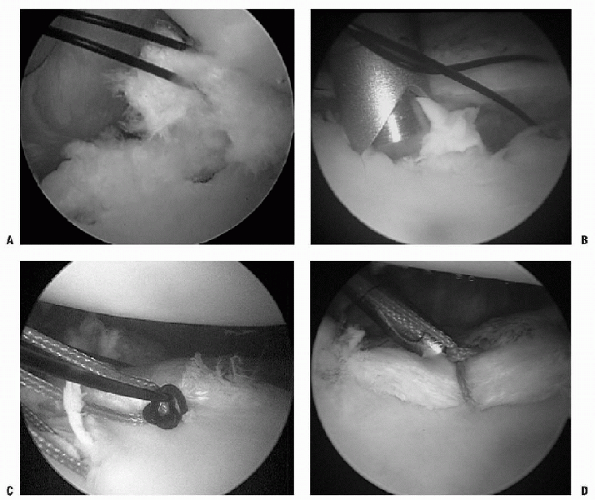
Figure 17-15 A: Arthroscopic view of suture-first technique. Zero PDS placed inferiorly and traction applied. B: Anchor placement more cephalic to suture, so that with eventual knot tying, the labrum and capsule are shifted superiorly. C: Nonabsorbable suture being shuttled with zero PDS. D: Knot-tying.
|
-
The suture-first technique involves
placing a passing suture initially to ensure adequate soft tissue
shift, followed by placement of the anchor (Fig. 17-15). A suture-passing device is placed through the anterior-inferior
P.227cannula. The capsular tissue is imbricated inferior to what would be
the 5 o’clock anchor position, thus enabling the tissue from
anterior-inferior glenohumeral ligament to be shifted superiorly. The
passing suture is passed through the tissue and shuttled through the
anterior-superior portal. The suture-passing device is removed, and the
suture limb that is in the anterior-inferior portal is switched to the
anterior-superior portal. Tension is placed on this suture to observe
the amount of shift that can be accomplished by placement of the anchor
at the appropriate position. -
If it is determined that this suture is not inferior enough, a second suture can be placed.
-
When an appropriate amount of tissue
tension is established, the anchor is placed through the
anterior-inferior portal and onto the glenoid rim. As was described
previously, once the anchor is placed, the two limbs of the suture are
separated—one through the anterior-superior cannula and the other limb
is shuttled through the tissue. -
The same steps are repeated two or three times, depending on the repair quality and amount of injury (Fig. 17-16).
-
If the labral tear extends from the
anterior-inferior glenoid up into the superior labrum, the same
anterior cannula can be used to continue placing suture anchors. -
We recommend two or three suture anchors
for superior labrum tears, with one placed in front of the biceps
tendon anchor and one or two suture anchors placed behind the biceps
tendon anchor, depending on the amount of biceps instability. -
The anchor placed in front of the biceps
tendon anchor is guided through the anterior-superior cannula. The one
or two anchors placed posterior to the biceps anchor can be placed
percutaneously via the “Port of Wilmington.” This portal is 1 cm
lateral and 1 cm anterior to the posterior-lateral corner of the
acromion, through the musculotendinous junction of the rotator cuff.
 |
|
Figure 17-16 Complete Bankart repair.
|
-
The rotator interval is an important
anatomic region with respect to anterior shoulder stability. This
anatomic region is defined as the articular capsule bounded superiorly
by the anterior portion of the supraspinatus tendon, inferiorly by the
superior portion of the subscapularis tendon, medially by the base of
the coracoid process, and laterally by the long head of the biceps
tendon. The capsular tissue is reinforced by the coracohumeral ligament
(CHL) and the superior glenohumeral ligament (SGHL). -
The rotator interval is of variable size
and is present in the fetus and in the adult. Sectioning the rotator
interval in cadaveric specimens has resulted in increased glenohumeral
translation in all planes tested. Imbrication of rotator interval
lesions results in decreased posterior and inferior glenohumeral
translation when compared with the intact state. Repair of the rotator
interval is a critical factor in shoulders treated arthroscopically for
anterior-inferior glenohumeral instability and may contribute to
improved clinical outcomes -
Many authors have reported techniques on
closing the rotator interval, but there is no literature comparing what
type of suture material will ensure success. One technique for rotator
interval closure involves removing the anterior-inferior cannula and
placing all instrumentation through the anterior-superior cannula. The
medial glenohumeral ligament and/or a small portion of the
subscapularis tendon is pierced with either a spinal needle or suture
shuttling device, and a monofilament suture is deployed (Fig. 17-17A). The SGHL/CHL complex is pierced with a penetrator and grasps the monofilament suture (Fig. 17-17B). This tissue then can be tied through a cannula internally or externally and cut with a guillotine knot cutter (Fig. 17-17C). -
The final repair for anterior traumatic
shoulder instability with a Bankart lesion involves capsular plication,
anterior-inferior labral repair, and rotator interval closure (see Fig. 17-9).
-
The first goal to postoperative success is maintenance of anterior-inferior stability.
-
The second goal is the restoration of adequate motion, specifically external rotation.
-
The third goal is a successful return to sports or physical activities of daily living in a reasonable amount of time.
-
The biological healing response of the
repaired and imbricated tissue must be respected. One observation that
may have led to some of the earlier arthroscopic failures for anterior
instability is that because of the significant reduction in
postoperative pain, these patients want to move their shoulders
earlier, imparting more stress to the repair site. This early cyclic
stress and motion eventually fatigues the plication stitches and causes
a failure of the repair. -
The University of Connecticut postoperative protocol
P.228for anterior-inferior shoulder instability treated by arthroscopic
means involves immobilization immediately postoperatively in an
abduction arthrosis.-
This allows the arm to be fixed in a
slight amount of external rotation. Codman exercises, combined with
pendulum exercises, are started immediately. Active assisted
range-of-motion exercises, external rotation (0 to 30 degrees), and
forward elevation (0 to 90 degrees) are also started at this time. This
regimen is maintained for the first 6 weeks. -
The use of cold therapy devices has been successful in reducing postoperative pain.
-
From weeks 6 to 12, active assisted as
well as active range-of-motion exercises are started with the goal of
establishing full range of motion. -
No strengthening exercises or any type of
repetitive exercises are started until after full range of motion has
been established. -
Early resistance exercises with
aggressive early postoperative rehabilitation do not appear to offer
substantial advantages and could compromise the repair. -
Strengthening is begun once there is
full, painless, active range of motion. Strengthening is begun at 12
weeks, with sports-specific exercises started at 16 to 20 weeks. -
Final contact athletic training is started between 20 and 24 weeks postoperatively.
-
-
Pagnani and Dome (2002)
reported on open stabilization in American football players. Their
postoperative program was quite similar to that previously described.-
At 0 to 4 weeks, the arm is immobilized
with a sling and internal rotation; double range-of-motion and pendulum
exercises are begun. -
From 4 to 8 weeks, passive and active assisted shoulder range of motion with external rotation limited to 45 degrees is done.
-
Rotator cuff strengthening and internal
and external rotation strengthening with the arm at low abduction
angles are begun when 140 degrees of active forward elevation is
obtained. -
From 8 to 12 weeks, deltoid isometric
exercises are started with the arm in low abduction angles, as well as
body blade exercises. Abduction is slowly increased during rotator cuff
and deltoid strengthening exercises. In addition, scapular stabilizer
strengthening and horizontal abduction exercises are also begun. -
After 18 weeks, conventional weight
training is begun, and rehabilitation is orientated toward return to
sports, progressing from field drills to contact drills. An abduction
harness can be used for selected football positions (linemen). -
Full-contact sports are instituted when abduction and external rotation strength are symmetrical on manual muscle testing.
-
 |
|
Figure 17-17 A: Suture shuttling device through the middle glenohumeral placing a monofilament suture into joint. B: Tissue penetrator through superior glenohumeral ligament and coracohumeral ligament retrieving monofilament suture. C: The rotator interval is closed extra-articularly.
|
-
Postoperative glenohumeral noise is an
inconsistent physical examination finding that occasionally plagues the
postoperative course. It is caused by a knot that rubs against the
humerus and glenoid with motion.
|
TABLE 17-3 RESULTS OF ARTHROSCOPIC BANKART REPAIR
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
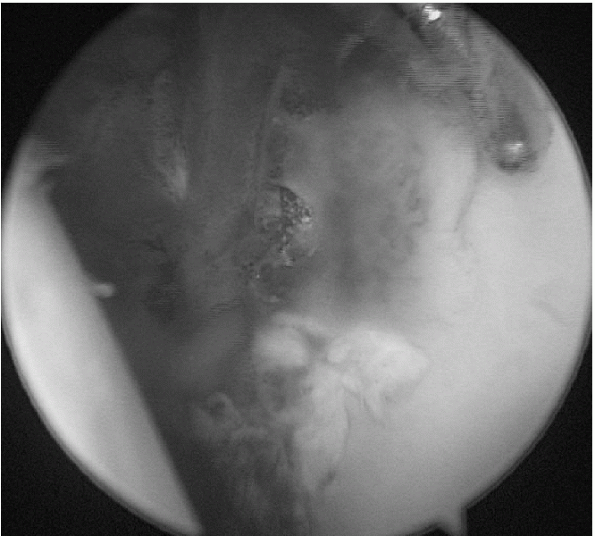
Figure 17-18 Example of labral repair 3 weeks after arthroscopic repair.
|
|
TABLE 17-4 RESULTS OF OPEN BANKART REPAIR
|
|||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Arthroscopic stabilization for
anterior-inferior instability has evolved over the past 25 years. It is
difficult to compare redislocation rates and subluxation rates with
techniques used in the past. This discussion will attempt to focus on
techniques that are similar to what have been described previously. -
It is important to note when evaluating
the literature whether recurrences are classified as subluxations that
prevent the athletes from returning to their sport versus
redislocations. Our definition of recurrence is any subluxation event
that causes the athlete to lose a day of practice. It is then noted if
the athlete required further stabilization or if they returned to play
unencumbered. -
Traumatic anterior instability treated by
suture anchor reconstruction has been associated with a stabilization
rate of 95% for 2 years. -
The recurrence rate after arthroscopic repair is about 15%.
-
Current arthroscopic stabilization
techniques use suture anchors, permanent suture, and address capsular
redundancy with plication techniques. The arthroscopic technique now
more closely mirrors the open method, and more recent reports
demonstrate results that are comparable with the open techniques. -
The rates of recurrence (dislocation and subluxation) in at-risk collision athletes are similar with both methods. Tables 17-3 and 17-4 are compilations of studies addressing the open versus arthroscopic issues.
RA, Wheeler JH, Ryan JB, et al. Arthroscopic Bankart repair versus
nonoperative treatment for acute, initial anterior shoulder
dislocations. Am J Sports Med 1994;22:589-594.
BR Jr, Warren RF, Fronek J. Disruption of the lateral capsule of the
shoulder: a cause of recurrent dislocation. J Bone Joint Surg Br
1988;702:274-276.
SS, DeBeer JF, Tehrany AM, et al. Quantifying glenoid bone loss
arthroscopically in shoulder instability. Arthroscopy 2002;18: 488-491.
DD, Lynch GP, Meyer CP, et al. Nonoperative management for in-season
athletes with anterior shoulder instability. Am J Sports Med
2004;32:1430-1433.
E, Hatakeyama Y, Kido T, et al. A new method of immobilization after
traumatic anterior dislocation of the shoulder: a preliminary study. J
Shoulder Elbow Surg 2003;12:413-415.
FA, Thomas SC, Rockwood CA, et al. Glenohumeral instability. In:
Rockwood CA, Matson FA, eds. The Shoulder, Vol. 2, 2nd ed.
Philadelphia: WB Saunders, 1990:633-639.
MJ, Dome DC. Surgical treatment of traumatic anterior shoulder
instability in American football players. J Bone Joint Surg Am
2002;84:711-715.
