Miscellaneous Neurologic Signs
signs—some of them reflexes, some closely related to the defense and
postural reflex mechanisms, and others more varied in nature—are
elicited in certain diseases of the nervous system.
meninges are inflamed—from infection (e.g., bacterial meningitis) or
from the presence of a foreign material (e.g., blood in the
subarachnoid space). Meningismus is a term that refers to the presence
of nuchal rigidity and other clinical signs of meningeal inflammation.
Meningism is sometimes used synonymously with meningismus, but it is
also used to refer to a syndrome characterized by neck stiffness
without meningeal inflammation, seen in patients with systemic
infections, particularly young children.
varied and depend on the severity of the process. Accompaniments depend
on etiology but commonly include headache, pain and stiffness of the
neck; irritability; photophobia; nausea and vomiting; and other
manifestations of infection, such as fever and chills. The various
maneuvers used to elicit meningeal signs produce tension on inflamed
and hypersensitive spinal nerve roots, and the resulting signs are
postures, protective muscle contractions, or other movements that
minimize the stretch and distortion of the meninges and roots.
frequently encountered sign of meningeal irritation, and the diagnosis
of meningitis is rarely made in its absence. It is characterized by
stiffness and spasm of the neck muscles, with pain on attempted
voluntary movement as well as resistance to passive movement. The
degree of rigidity varies. There may be only slight resistance to
passive flexion, or marked spasm of all the neck muscles. Nuchal
rigidity primarily affects the extensor muscles, and the most prominent
early finding in meningeal irritation is resistance to passive neck
flexion. The physician is unable to place the patient’s chin on his
chest, but the neck can be hyperextended without difficulty; rotatory
and lateral movements may also be preserved. With more severe nuchal
rigidity there may be resistance to extension and rotatory movements as
well. Extreme rigidity causes retraction of the neck into a position of
opisthotonos, the body assuming a wrestler’s bridge or arc de cercle
position, with the head thrust back and the trunk arched forward.
Rigidity may be absent in meningitis when the disease is fulminating or
terminal, when the patient is in coma, or in infants.
conditions. A common problem is to distinguish restricted neck motion
due to cervical spondylosis or osteoarthritis from nuchal rigidity.
Patients with osteoarthritis typically have difficulty with rotation
and lateral bending of the neck; these motions are usually preserved in
patients who have meningismus, unless the meningeal irritation is
extremely severe. Restricted neck motion may also occur with
retropharyngeal abscess, cervical lymphadenopathy, neck trauma, and as
a nonspecific manifestation in severe systemic infections.
Extrapyramidal disorders, particularly progressive supranuclear palsy,
may also cause diffuse rigidity of the neck muscles. Meningeal signs
may occur with increased spinal fluid pressure, and nuchal rigidity may
be a manifestation of cerebellar tonsillar (foramen magnum) herniation.
Meningeal irritation may also cause resistance to movement of the legs
and back, with the patient lying with his legs drawn up and resisting
passive extension.
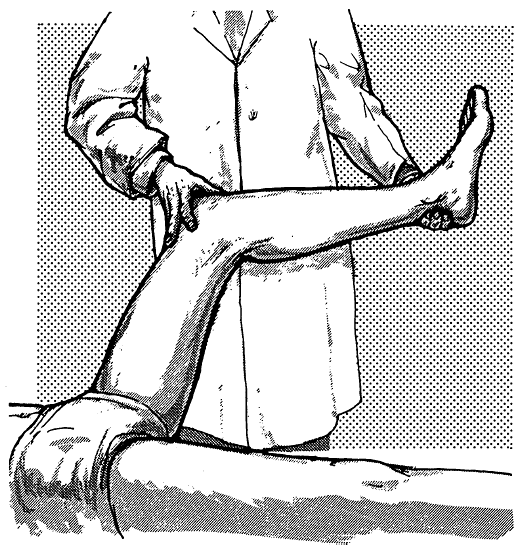
elicit a Kernig sign. Kernig described an involuntary flexion at the
knee when the examiner attempted to flex the hip with the knee
extended. The more common method is to flex the hip and knee to right
angles, and then attempt to passively extend the knee. This movement
produces pain, resistance, and inability to fully extend the knee;
another definition of Kernig sign is inability to extend the knee to
over 135 degrees while the hip is flexed (Figure 36.1).
There is some overlap between Kernig sign and the Lasègue (straight leg
raising) sign. The technique is similar, but Lasègue sign is used to
check for root irritation in lumbosacral radiculopathy. Both Kernig
sign and straight leg raising are positive in meningitis because of
diffuse inflammation of the nerve roots and meninges, and positive with
acute lumbosacral radiculopathy because of focal inflammation of the
affected root. In radiculopathy the signs are usually unilateral, but
in meningitis they are bilateral.
 |
|
FIGURE 36.1 • Method of eliciting Kernig sign.
|
the neck while holding down the chest with the other hand causes
flexion of the hips and knees bilaterally. With severe meningismus, it
may not be possible to hold the chest down, and the patient may be
pulled into a sitting position with only the examiner’s hand behind the
head. Occasionally there may be extension of the hallux and fanning of
the toes, and sometimes arm flexion. The leg may fail to flex on one
side when meningeal irritation and hemiplegia coexist.
sit in bed with the hands placed far behind, the head thrown back, the
hips and knees flexed, and the back arched (Amoss, Hoyne, or tripod
sign).
tonic contractions of the skeletal muscles, principally the distal
muscles of the extremities. There may be carpopedal spasm, with tonic
contraction of the muscles of the wrists, hands, fingers, feet, and
toes. There is hyperexcitability of the entire peripheral nervous
system, as well as the musculature, to even minimal stimuli. Sensory
nerve involvement may cause paresthesias in the hands, feet, and
perioral region. Tetany is related to a disturbance of calcium
metabolism or alkalosis, causing a decrease in the ionized calcium
level. Certain neurologic signs may be present that aid in making a
diagnosis on the basis of the clinical examination alone. They are more
easily obtained if the patient first hyperventilates for a few minutes
(latent tetany). Severe tetany may cause seizures, laryngospasm,
stridor, and respiratory arrest.
cramplike contraction of some or all of the facial muscles. Two points
of stimulation have been described: just below the zygomatic process of
the temporal bone, in front of the ear (Chvostek sign) and midway
between the zygomatic arch and the angle of the mouth. Sometimes the
response may be elicited merely by stroking the skin in front of the
ear. The sign is minimal if only a slight twitch of the upper lip or
the angle of the mouth results; moderate if there is movement of the
ala nasi and the entire corner of the mouth; maximal if the muscles of
the forehead, eyelid, and cheek also contract. When the response is
marked, even muscles supplied by the trigeminal nerve may respond.
Chvostek sign is the result of a hyperexcitability of the motor nerves,
in this instance the facial nerve, to mechanical stimulation. It is an
important sign in tetany, but may occur in other conditions in which
there is hyperreflexia, such as in lesions of the corticospinal tract.
It is present in a majority of neonates and disappears during childhood.
excitability and causes spontaneous discharges. Compression of the arm
by manual pressure, a tourniquet, or a sphygmomanometer cuff is
followed first by distal paresthesias that progress centripetally, then
twitching of the fingers, and finally by cramping and contraction of
the muscles of the fingers and hand with the thumb strongly adducted
and the fingers stiffened, slightly flexed at the metacarpophalangeal
joints, and forming a cone clustered about the thumb (obstetrician’s or
accoucheur’s hand, main d’accoucheur). There may be a latent period of
30 sec to 4 minutes. Similar pressure around the leg or thigh will
cause pedal spasm. A modification is to keep a moderately inflated
sphygmomanometer cuff on one arm for about 10 minutes, and then remove
it and have the patient hyperventilate; typical tetanic spasm occurs
earlier in the previously ischemic arm.
paresthesias, can provide localizing information in suspected CR.
Radiating pain on coughing, sneezing, or straining at stool (Dejerine
sign) is significant but seldom elicited. Increased pain on shoulder
motion suggests nonradicular pathology. Relief of pain by resting the
hand atop the head (hand on head sign) is reportedly characteristic of
CR, but the author has seen this phenomenon with a Pancoast tumor. Hand
paresthesias at night suggest carpal tunnel syndrome, but carpal tunnel
syndrome can occur in association with CR (“double crush syndrome”), so
nocturnal acroparesthesias do not exclude coexistent radiculopathy.
should include an assessment of the range of motion of the neck and
arm, a search for root compression signs, detailed examination of
strength and reflexes, a screening sensory examination, and probing for
areas of muscle spasm or trigger points. Patients with either weakness
or reduced reflexes on physical examination are up to five times more
likely to have an abnormal electrodiagnostic study. A normal physical
examination by no means excludes CR (negative predictive value 52%).
informative. Patients should be asked to put chin to chest and to
either shoulder, each ear to shoulder and to hold the head in full
extension; these maneuvers all affect the size of the intervertebral
foramen. Pain produced by movements that narrow the foramen suggest CR.
Pain on the symptomatic side on putting the ipsilateral ear to the
shoulder suggests radiculopathy, but increased pain on leaning or
turning away from the symptomatic side suggests a myofascial origin.
Radiating pain or paresthesias with the head in extension and tilted
slightly to the symptomatic side is highly suggestive of CR (Spurling
sign or maneuver, foraminal compression test); brief breath holding or
gentle Valsalva in this position will sometimes elicit the pain if
positioning alone is not provocative. The addition of axial compression
by pressing down on the crown of the head does not seem to add much.
The Spurling test is specific, but not very sensitive. Light digital
compression of the jugular veins until the face is flushed and the
patient is uncomfortable will sometimes elicit radicular symptoms:
unilateral shoulder, arm, pectoral or scapular pain, or radiating
paresthesias into the arm or hand (Viets sign). A slight cough while
the face is suffused may increase the sensitivity. In the past,
clinicians sometimes went so far as to put a blood pressure cuff around
the patient’s neck to occlude the jugular veins (Naffziger sign). The
two eponyms are often used interchangeably, and more often Naffziger
sign is used for both techniques. Jugular compression is thought to
engorge epidural veins or the cerebrospinal fluid (CSF) reservoirs,
which in the normal individual is harmless. But when some element of
foraminal narrowing and nerve root pressure exists, the additional
compression causes the acute development of symptoms. The same
mechanism likely underlies the exacerbation of root pain by coughing,
sneezing, and straining. Like the Spurling test, the Viets/Naffziger
sign is specific but insensitive. It is less useful in lumbosacral than
in cervical radiculopathy. An occasional CR patient has relief of pain
with manual upward neck traction, particularly with the neck in slight
flexion (cervical distraction test). Some patients have a decrease in
pain with shoulder abduction (shoulder abduction relief test); this
sign is more likely to be present with soft disc herniation. The
mechanism is uncertain but probably related to the hand on the head
sign. Flexion of the neck may cause Lhermitte sign in patients with
cervical spondylosis or large disc herniations. Pain or limitation of
motion of any upper-extremity joint should signal the possibility of
nonradicular pathology. The differentiation of CR from primary shoulder
disease (e.g., bursitis, capsulitis, tendinitis, rotator cuff disease,
or impingement syndrome) can be particularly difficult.
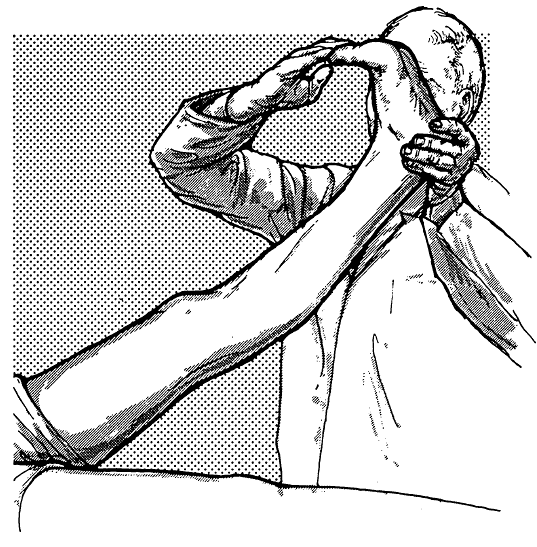
examination findings has been studied. The straight leg raising (SLR,
Lasègue) test remains the mainstay in detecting radicular compression.
The test is performed by slowly raising the symptomatic leg with the
knee extended (Figure 36.2). Pain
caused by flexing the hip with the knee bent is suggestive of hip
disease. During SLR tension is transmitted to the nerve roots between
about 30 degrees and 70 degrees, and pain increases. Pain at less than
30 degrees raises the question of nonorganicity, and some discomfort
and tightness beyond 70 degrees is routine and insignificant. There are
various degrees or levels of positivity. Ipsilateral leg tightness is
the lowest level, pain in the back more significant, and radiating pain
in the leg highly significant. When raising the good leg produces pain
in the symptomatic leg (crossed straight leg raising, Fajersztajn
sign), the likelihood of a root lesion is very high. Rarely, SLR may
even cause numbness and paresthesias in the distribution of the
affected nerve root. The buckling sign is knee flexion during SLR to
avoid sciatic nerve tension. Kernig sign is an alternate way of
stretching the root. Various SLR modifications may provide additional
information; all of these variations are referred to as root stretch
signs. The pain may be more severe, or elicited sooner, if the test is
carried out with the thigh and leg in a position of adduction and
internal rotation (Bonnet phenomenon). The SLR can be enhanced by
passively dorsiflexing the patient’s foot (Bragard sign) or great toe
(Sicard sign) just at the elevation angle at which the increased root
tension begins to produce pain (Figure 36.3).
The term Spurling sign is also used for either of these. A quick snap
to the sciatic nerve in the popliteal fossa just as stretch begins to
cause pain (bowstring sign, or popliteal compression test) accomplishes
the same end, and may cause pain in the lumbar region, in the affected
buttock, or along the course of the sciatic nerve. In severe cases,
pain may be elicited merely by dorsiflexion of the foot or great toe as
the patient lies supine with legs extended. A similar modification may
be carried out by flexing the thigh to an angle just short of that
necessary to cause pain, and then flexing the neck; this may produce
the same exacerbation of pain that would be brought about by further
flexion of the hip (Brudzinski, Lidner, or Hyndman sign). Occasionally,
the pain may be brought on merely by passive flexion of the neck when
the patient is recumbent with legs extended. The pain with SLR should
be the same with the patient supine or seated. Failure of a patient
with a positive supine SLR to complain or lean backward when the
extended
leg is brought up while in the seated position (e.g., under the guise
of doing the planter response) suggests nonorganicity. In the sitting
position, the patient may be able to extend each leg alone, but
extending both together causes radicular pain (Bechterew test).
 |
|
FIGURE 36.2 • Method of eliciting the Lasègue sign.
|
 |
|
FIGURE 36.3 • Accentuation of the Lasègue sign by dorsiflexion of either the foot or the great toe.
|
of eliciting root stretch in the evaluation of high lumbar
radiculopathy. The patient lies prone, and the knee is pulled into
maximum flexion; or the examiner pulls upward on the extended knee to
passively extend the hip. In the bent knee pulling test the patient’s
knee is flexed and the examiner pulls upward on the ankle while pushing
the buttock forward (in the same way as for eliciting the psoas sign
used in the diagnosis of appendicitis). In all these variations, the
normal individual should complain only of quadriceps tightness. With
disc disease there is pain in the back or in the femoral nerve
distribution on the side of the lesion.
posture, deformities, tenderness, and muscle spasm. With radiculopathy,
there may be loss of the normal lumbar lordosis because of involuntary
spasm of the paravertebral muscles. In addition, there is often a
lumbar scoliosis, with a compensatory thoracic scoliosis. Most
commonly, the list of the body is away from the painful side, and the
pelvis is tilted so that the affected hip is elevated. The patient
attempts to bear weight mostly on the sound leg. The list and scoliosis
may sometimes be toward the painful side, and the patient’s body may be
bent forward and toward that side to avoid stretching the involved
root. With very severe sciatic pain, the patient will avoid complete
extension at the knee, and may place only the toes on the floor, since
dorsiflexion of the foot aggravates the pain by stretching the nerve.
The patient may walk with small steps and keep the leg semi-flexed at
the knee. In bending forward, she flexes the knee to avoid stretching
the nerve (Neri sign). When sitting, she keeps the affected leg flexed
at the knee and rests her weight on the opposite buttock. She may rise
from a seated position by supporting herself on the unaffected side,
bending forward, and placing one hand on the affected side of the back
(Minor sign). There may be areas of tenderness in the lumbosacral
region, and manipulation or percussion over the spinous processes, or
pressure just lateral to them, may reproduce or exacerbate the pain. A
sharp blow with a percussion hammer, on or just lateral
to
the spinous processes, while the patient is bending forward, may bring
out the pain. There may be not only spasm of the paravertebral muscles,
but also the hamstrings and calf muscles. Flexion, extension, and
lateral deviation of the spine are limited; the pain is usually
accentuated with passive extension of the lumbar spine toward the
affected side while the patient is standing erect. There may be
localized tenderness at the sciatic notch and along the course of the
sciatic nerve. Pelvic and rectal examination may be necessary in some
instances.
power in the major lower-extremity muscle groups, but especially the
dorsiflexors of the foot and toes, and the evertors and invertors of
the foot. Plantar flexion of the foot is so powerful that manual
testing rarely suffices. Having the patient do 10 toe raises with
either foot is a better test. As the patient is standing on one leg,
look for the Trendelenburg sign. Normally the pelvis slants upward
toward the unsupported leg. With a positive Trendelenburg the hip moves
up and the shoulder moves down on the weight-bearing side, and the
pelvis sags toward the unsupported leg. The Trendelenburg sign may
occur when there is weakness of the hip abductors, as in L5
radiculopathy, but it may also occur with musculoskeletal disease, such
as hip dislocation, fracture of the femoral head, or coxa vara. In
addition to assessing power, it is important to look for atrophy and
fasciculations. Sensation should be tested in the signature zones of
the major roots. The status of knee and ankle reflexes reflects the
integrity of the L3-L4 and S1 roots, respectively. There is no good
reflex for the L5 root, but the hamstring reflexes are sometimes
useful. An occasional L5 radiculopathy produces a clear selective
diminution of the medial hamstring reflex.
evaluation of LBP. Pain during simulated spinal rotation, pinning the
patient’s hands to the sides while rotating the hips (no spine rotation
occurs as shoulders and hips remain in a constant relationship)
suggests nonorganicity. Also useful are a discrepancy between the
positivity of the SLR between the supine and seated position, pain in
the back on pressing down on top of the head, widespread and excessive
“tenderness” (touch-me-not or Waddell sign), general overreaction
during testing, and nondermatomal/nonmyotomal neurologic signs. The
presence of three of these signs suggests, if not nonorganicity, at
least embellishment.
