SURGERY FOR KYPHOSIS DEFORMITY
Phoenix Spine Center, St. Luke’s Hospital Medical Center, Phoenix,
Arizona, 85006; and Department of Materials, Chemical and
Bioengineering, Arizona State University.
the spine in the sagittal plane. In the thoracic spine, the normal
kyphosis ranges from 20° to 40° as measured from the superior endplate
of the second thoracic vertebra to the inferior endplate of the twelfth
thoracic vertebra. In the adult cervical and lumbar spine, both of
which are normally lordotic, any posteriorly directed curvature of 5°
or greater is considered abnormal kyphosis.
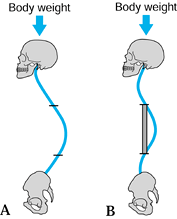
In rotational kyphosis, however, the vertebral bodies are rotated out
of the sagittal plane, as is commonly seen in paralytic curvatures and
kyphosis secondary to neurofibromatosis (Fig. 161.2).
In either situation, once the anterior vertebral column is no longer in
the sagittal plane, there is reduced resistance to kyphotic bending
moments and thus an increased propensity for a kyphosis to progress.
Most kyphotic deformities seem to fall within the sagittal kyphosis
category.
 |
|
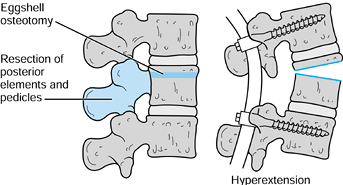
Figure 161.1. This 1-year-old child has a short-radius sagittal kyphosis secondary to radiation and laminectomy for neuroblastoma.
|
 |
|
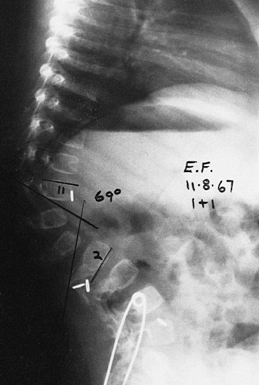
Figure 161.2. A: A 9-year-old child has a paralytic right thoracolumbar scoliosis of 125°. B: In addition to the paralytic scoliosis, a rotational thoracolumbar kyphosis of 107° is present. C: The rotational kyphosis corrects to 36° on supine hyperextension (a flexible kyphosis).
|
and a long-radius kyphotic deformity. A shortradius curve is one that
is more angular over a few vertebral
segments, and a long-radius kyphosis is a smooth curve of less acute angulation over many vertebral segments (Fig. 161.1, Fig. 161.3).
 |
|
Figure 161.3.
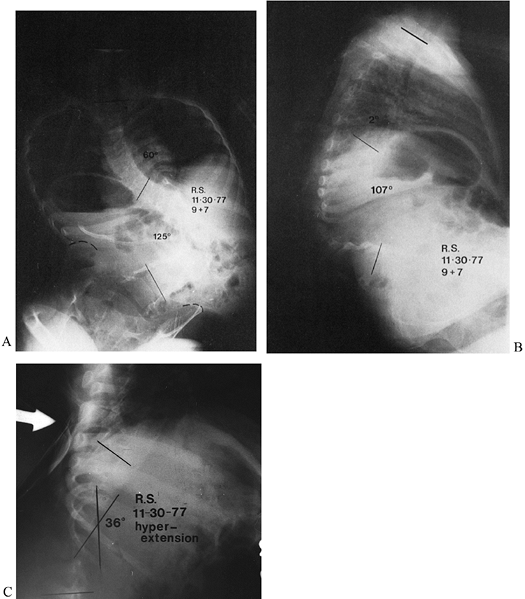
At age 17 years, this patient developed a long-radius thoracolumbar kyphosis of 70° as a result of radiation. This kyphosis corrects to 45° on a supine hyperextension lateral radiograph. |
rigidity and flexibility. Frequently there is an element of apical
rigidity with variable degrees of flexibility at the ends of the
curvature. The goal in correcting the kyphosis is to mobilize the rigid
apex or to correct the flexible ends of the curve to bring the apex
closer to the center of gravity, thereby placing the bone graft in the
area of fusion under maximum compression (Fig. 161.4).
 |
|
Figure 161.4. A: Diagram of kyphosis. B:
The apex has been corrected somewhat and the flexible ends of the kyphosis are corrected so that the anterior strut graft is now in line with the body weight (BW). |
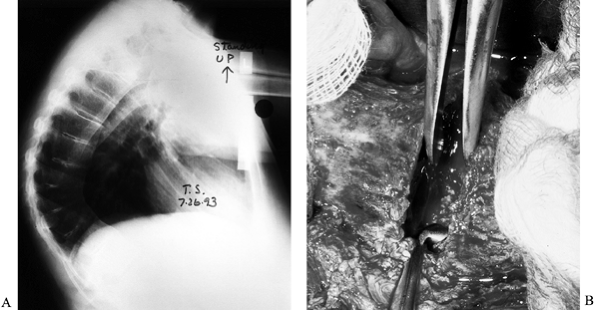
surgery by a supine hyperextension lateral radiograph of the spine
taken with a bolster placed under the apex of the kyphosis (Fig. 161.3)
in short-radius kyphosis, and by a lateral radiograph of the spine with
the patient in traction in long-radius paralytic curves.
gradually replaced by more aggressive anterior and posterior fusion and
segmental instrumentation, in some situations traction can be helpful.
Three traction techniques can be beneficial in the treatment of
kyphosis: halo-wheelchair
traction,
halo-femoral traction, and halo-hyperextension traction.
Halo-wheelchair traction provides longitudinal traction against gravity
and allows the patient mobility. Halo-femoral traction provides
stronger, steady axial forces if continuous traction is essential.
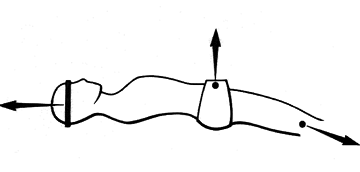
of heavy axial traction. If there is apical rigidity of the curve as
determined by hyperextension lateral radiographs, paraplegia can be a
complication because of the spinal cord’s stretching over the rigid
acute kyphotic apex. Mobilizing the apex of a kyphotic deformity is
essential before heavy traction is used. In large kyphotic deformities
that have a short radius (neurofibromatosis), axial traction is more
beneficial than three-point bending. In comparison, large kyphotic
deformities with a long radius (such as Scheuermann’s kyphosis) respond
more effectively to three-point bending. In short-radius kyphotic
deformities (such as spondylolisthesis), a combination of axial
traction and three-point bending is needed (Fig. 161.5) (13).
 |
|
Figure 161.5. Halo-femoral longitudinal and pelvic hyperextension traction for lumbosacral kyphosis from spondylolisthesis.
|
may need treatment. Any kyphosis that is increasing in magnitude may
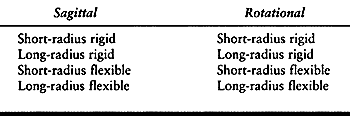
need surgical stabilization. It is helpful to classify the disorders by
the degree of rigidity and flexibility as well as the magnitude of
curve radius (Table 161.1).
 |
|
Table 161.1. Classification of Kyphoses
|
the diagnosis, the etiology of the kyphosis, the curve progression, the
location of the kyphosis, and the age of the patient. In general, the
kyphotic spine deformity that is increasing in magnitude in an adult
needs surgical stabilization. In the child, however, a brace may be
helpful, depending on the age of the child, the etiology of the
kyphosis, and the magnitude of the curve.
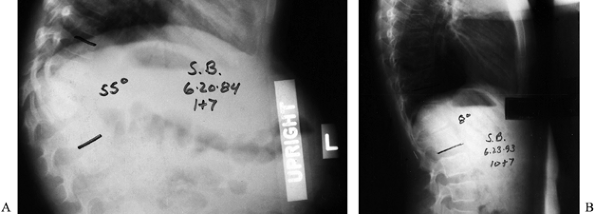
which there is incomplete vertebral formation, is usually diagnosed in
childhood and has an average progression of 5° yearly (26,27,29).
It usually involves only two to three vertebrae, and surgical
stabilization is usually recommended when progression has been
documented. There is a high incidence of spinal cord compression with
large degrees of kyphosis, and early stabilization in a young child
when the curve is small is ideal. An in situ posterior fusion before the age of 3 years will prevent late deformity. In situ
posterior fusion must include the normal vertebrae above and below the
congenital kyphosis. The posterior fusion will tether the posterior
growth of these normal vertebrae so that their anterior growth will
correct the deformity (these normal vertebrae will become trapezoidal
in shape with growth) (Fig. 161.6).
 |
|
Figure 161.6. A: This 1½-year-old girl has type II congenital kyphosis at T-12–L-1 of 55°. B: At age 10, after in situ posterior fusion that included the normal vertebra above and below the congenital kyphosis. The kyphosis has corrected to 8°.
|
thick posterior mass, thick enough to withstand the anterior growth
forces. When an angulation of 50° or more is present, an anterior
fusion is also needed. If the spinal cord is compressed anteriorly,
perform an anterior decompression concomitantly with the anterior strut
graft fusion. In the adult, I recommend a second-stage posterior fusion
with instrumentation after the anterior correction. Osteotomies for
deformity correction are not commonly used as in type II congenital
kyphosis.
failure of segmentation of the spine occurs anteriorly, progression of
the kyphosis usually averages 5° yearly (15).
The segmentation failure can involve only two vertebrae but also may
involve many contiguous vertebrae. For young patients, I recommend an in situ
posterior fusion to include one normal vertebral segment at each end of
the curve. In the young child, an augmentation posterior spinal fusion
may be necessary 6 months later to generate a thick fusion (Fig. 161.6).
In the adolescent patient with an unacceptable kyphosis greater than
50°, a staged correction is indicated, with anterior osteotomy and
anterior fusion using an intervertebral cage structural graft, followed
by posterior fusion and instrumentation (15,26,27,29). Spinal cord compression is usually not seen in type II congenital kyphosis.
fracture or dislocation usually requires reduction of the kyphosis,
with spinal fusion (14,19).
When the kyphosis occurs late and is increasing in magnitude, surgical
stabilization and fusion are indicated. Particularly if the kyphosis
spans multiple vertebral segments, a two-stage anterior and posterior
fusion and stabilization are frequently necessary. In late
posttraumatic kyphosis, the use of intervertebral structural cages with
anterior fusion maintains lumbar lordosis below the fracture more
effectively than an interbody fusion alone.
usually lumbosacral kyphotic deformities and require reduction,
stabilization, and fusion (4).
Posterior segmental instrumentation and fusion will be necessary along
with anterior fusion. Frequently, strut graft stabilization will be
needed in larger kyphotic deformities. The entire kyphotic deformity
must be instrumented and fused (11).
In older adolescents with little vertebral growth remaining, a kyphosis
of 70° or more usually requires surgical correction and fusion,
especially if associated with back pain. In the adult, back pain
associated with thoracic kyphosis greater than 75° to 80° is an
indication for surgical treatment. If the kyphosis is located in the
thoracolumbar spine, surgical treatment is indicated when the curve
magnitude is much less than 70° because of the acute lumbar
hyperlordosis below the kyphosis and associated problems with low back
pain in an adult. A staged anterior interbody fusion followed by a
posterior fusion with segmental instrumentation will effectively
correct and stabilize this kyphosis; intervertebral cages could be used
to maintain correction of the kyphosis and maintain lumbar lordosis (Fig. 161.7).
 |
|
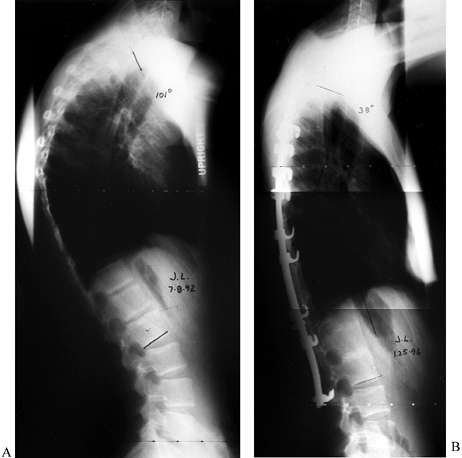
Figure 161.7. A: An 18-year-old man with 101° thoracic kyphosis from Scheuermann’s disease. B:
Four years after staged anterior interbody fusion and posterior fusion and segmental instrumentation. The kyphosis is corrected to 38°. |
is documented to be progressive despite adequate orthotic treatment. It
is also indicated when the kyphosis is too large for orthotic control,
or the deformity is cosmetically unacceptable. These curves are usually
rigid and the potential for correction is limited.
Surgical treatment of the kyphosis is usually planned when the child
has a skeletal age of 10–12 years, when most of the axial skeletal
growth has occurred. Until that age, orthotic treatment is recommended.
orthotic treatment, and surgery is indicated when the kyphosis is 50°
or more in a child or is documented to be increasing in magnitude (1,28). Anterior and posterior arthrodesis and instrumentation are usually necessary. Complications are common.
Thoracic and thoracolumbar kyphoses usually appears in the juvenile
years, is associated with scoliosis, and should receive early orthotic
treatment. If progression occurs despite orthotic treatment, surgical
treatment of the kyphosis is indicated.
may occur at an early age, but most kyphoses resolve. When apical
vertebral hypoplasia is present (achondroplasia) (25),
progression may occur and orthotic treatment is recommended. Surgical
treatment of the kyphosis is indicated if progression occurs despite
orthotic treatment or if anterior spinal cord compression occurs.
surgically when the kyphoscoliosis is progressing and if the scoliosis
is greater than 60° to 70° (19). Frequently,
the lumbar curve in kyphoscoliosis has rotational vertebral subluxation
and is relatively kyphotic. Adult scoliosis frequently requires
anterior and posterior arthrodesis and instrumentation. Structural
intervertebral cage grafts anteriorly are useful in creating and
maintaining lumbar lordosis.
lordosis and normal sacral slope. For patients with flatback syndrome
to stand, their trunks must remain bent forward. To maintain this
position, they are required to flex their knees, and they complain of
pain and fatigue (6,8,10).
This syndrome is frequently seen after posterior distraction
instrumentation in the lumbar spine, especially if the instrumentation
approaches L-5 or the sacrum without supplemental anterior support (Fig. 161.8).
 |
|
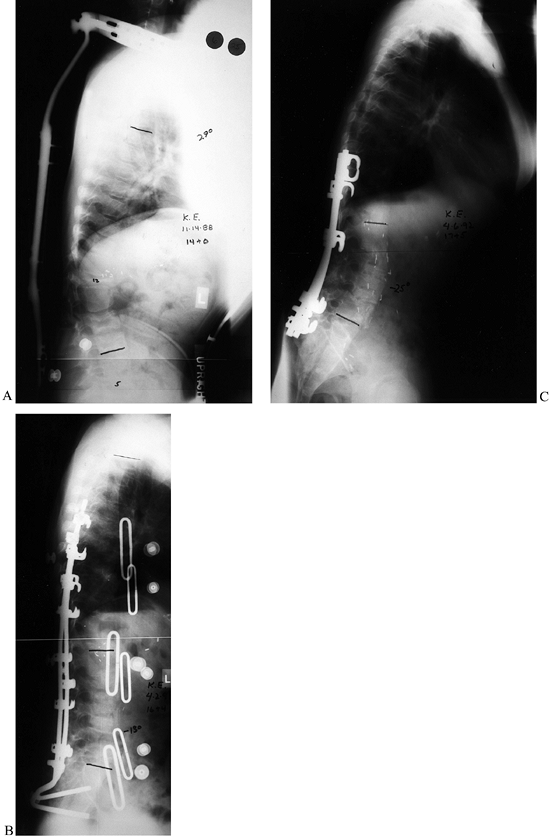
Figure 161.8. A:
This 14-year-old boy has Gauché’s disease with collapse of T-12, L-2, and L-5, with kyphosis and back pain. He has been treated for several years with an orthosis. B: Six months after posterior fusion and instrumentation to the sacrum, the lumbar lordosis was minus 13°. He had difficulty maintaining an upright posture (flatback syndrome). C: After anterior/posterior osteotomies, fusion, and instrumentation, the sagittal alignment is much improved. |
compression instrumentation cannot maintain correct sagittal alignment.
In this situation, intervertebral structural cage arthrodesis may be
helpful to correct and maintain lumbar lordosis, in conjunction with
posterior segmental instrumentation and arthrodesis. A flatback from a
previous fusion needs posterior osteotomies along with anterior and
posterior stabilization and arthrodesis.
(Marie-Strümpel Kyphosis) is common and requires surgical treatment to
maintain an upright head position. Usually, anterior and posterior
osteotomies with segmental instrumentation are necessary. Single-level
or multiple-level osteotomies may be utilized (5,7,9,21,22,24) (see Chapter 153, Chapter 154).
short-radius and a long-radius kyphosis, and determine whether the
curve is flexible or rigid. In short-radius curves, obtain a
hyperextension cross-table lateral radiograph with a bolster under the
apex of the kyphosis. Two interpretations should be made: the
correctability of the apex of the kyphosis and the correctability of
the ends of the kyphosis (Fig. 161.4) (13).
occurs in the more flexible ends of the kyphotic curve. When the ends
of the kyphosis are flexible, a long-radius, unstable kyphosis can be
converted to a short-radius stable curve. In this situation, use an
anterior strut and interbody fusion as a first stage to stabilize the
apical rigid component. Follow with a posterior approach to correct the
flexible ends of the kyphosis, usually with segmental instrumentation.
The goal at completion is to have the body weight in line with the
apical strut graft, a curve configuration that is biomechanically
stable (Fig. 161.4) (13).
with the patient in longitudinal traction, is more helpful,
particularly in paralytic curves. In general, rigid kyphotic
deformities require strut grafting and interbody fusion of the rigid
apical component in addition to posterior fusion and stabilization.
Some mobilization of the rigid apex can be accomplished with disc
excision and osteotomy, placing a strong strut graft in the corrected
position.
congenital kyphosis) is generally contraindicated because of the risk
of precipitating anterior spinal cord compression. Preoperative
traction for relatively inflexible long-radius curves is usually not
beneficial, but it can be beneficial after an anterior disc excision,
interbody fusion, and anterior release. In this situation,
halo-hyperextension traction for 2 weeks between an anterior spinal
release and fusion and a second-stage posterior fusion and
instrumentation can be useful.
spinal cord compression, careful and judicious halo-femoral traction
may provide enough correction to improve neurologic function before
surgical stabilization. Preoperative traction is useful in this
situation, because the apex of the kyphosis is frequently rotated and
inherently more flexible (28). A preoperative
myelogram and computed tomography (CT) scan are recommended in
neurofibromatosis because of the high incidence of dural ectasia and
intradural and extradural tumors.
and in thoracolumbar kyphosis in achondroplasia, obtain a CT scan to
verify the spinal-canal size and bony architecture before surgery.
Preoperative somatosensory, evoked potentials are useful for baseline
measurements in preparation for intraoperative spinal cord monitoring.
posterior instrumentation. To be mechanically sound, the posterior
instrumented end vertebrae should be close to the weight-bearing line.
Include the entire length of the kyphotic curve in the fusion and
instrumentation.
-
Strut graft (fibula or rib)
-
Inlay rib graft
-
Interbody fusion
-
Vascularized rib or fibular graft
-
Anterior vertebral osteotomy
-
Interbody screw and rod instrumentation for rotational kyphosis
-
Intervertebral structural cages
-
Posterior spinal fusion with Moe facet fusion
-
Posterior segmental instrumentation
-
Posterior vertebral osteotomy
-
Eggshell technique
exposure of the spine is recommended for maximal bone exposure for
arthrodesis.
-
Note the end vertebrae of the kyphosis
and perform complete discectomies at each disc space between the end
vertebrae. Incise the annulus fibrosus with a knife and excise the
annulus with a narrow Luxsell rongeur. -
Incise the periphery of the cartilaginous
endplate down to bone with a knife and peel it off the bony vertebral
endplate with a narrow Cobb elevator. -
Remove the endplates with rongeurs, and remove the remaining disc with straight and angled curets.
-
Pack the disc space with thrombin-soaked Gelfoam.
annulus, curet the endplates and interior of the bodies of the end
vertebrae to create a seating hole for the strut.
-
Correct the kyphosis by pushing on the apex of the curve and measure the length of strut required in the corrected position.
-
Cut the graft (rib or fibula) longer than measured and round the ends with bone cutters.
-
Insert one end of the strut in the end
vertebra. Cut a trough in the lateral aspect in the other end vertebra.
Correct the kyphosis by pushing on its apex, and impact the strut
through the side trough and into the undercut end vertebra (Fig. 161.9). The intervening vertebra may have to be fashioned to allow the strut graft to fit. Figure 161.9. Intraoperative picture of an anterior strut graft.
Figure 161.9. Intraoperative picture of an anterior strut graft. -
Pack the intervertebral disc spaces solidly with morselized rib graft.
-
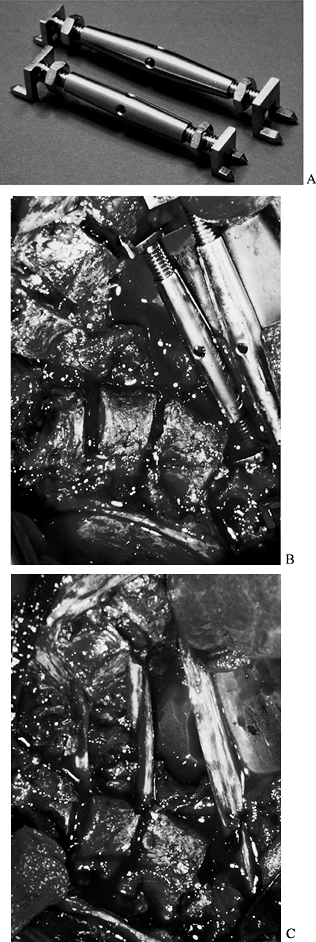
If the kyphosis is larger and angular,
several parallel struts may have to be used. Use Pinto distractors to
correct the kyphosis while the struts are inserted. These distractors
are nonimplantable and come in three sizes. Each distractor is a
turnbuckle with pronged feet at each end that anchor in the vertebral
bodies. When maximum correction of the apical kyphosis is achieved,
insert the struts and remove the Pinto distractors (Fig. 161.10).![]() Figure 161.10. A: Pinto distractors (nonimplantable). B: Acute angular kyphosis with two Pinto distractors holding the deformity in a corrected position. C: The Pinto distractors are removed and the three strut grafts are anchored in the vertebrae.
Figure 161.10. A: Pinto distractors (nonimplantable). B: Acute angular kyphosis with two Pinto distractors holding the deformity in a corrected position. C: The Pinto distractors are removed and the three strut grafts are anchored in the vertebrae. -
In large kyphotic deformities it is
important to fill the dead space between the vertebral bodies and the
strut graft with bone graft (Fig. 161.11) (19).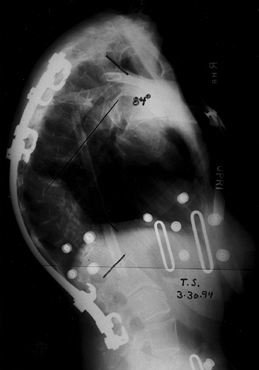 Figure 161.11. Radiograph shows an anterior fibular graft with bone graft positioned back to the vertebral bodies.
Figure 161.11. Radiograph shows an anterior fibular graft with bone graft positioned back to the vertebral bodies.
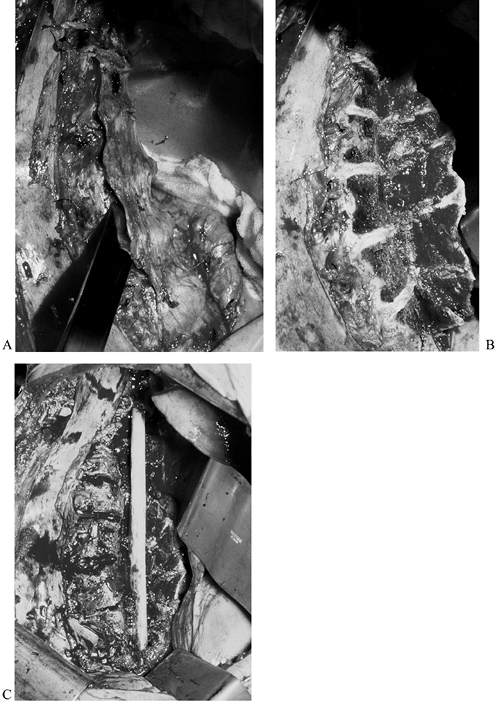
strut graft technique, originally pioneered by P. Stagnara, consists of
creating an osteoperiosteal flap from the vertebral bodies that are in
the kyphotic area (23).
-
Use a wide osteotome to reflect the
anterior portion of the vertebrae for the length of the kyphotic curve.
This technique creates a good vascular bed. -
Countersink the fibular or rib strut
graft, with the bony flap adjacent to the graft, usually on the
concavity of the scoliotic curve. -
Pack the intervertebral disc spaces with bone graft (Fig. 161.12).
![]() Figure 161.12. A: A Lambotte osteotome is used to create a vertebral flap. B: The vertebral flap is mobilized. C:
Figure 161.12. A: A Lambotte osteotome is used to create a vertebral flap. B: The vertebral flap is mobilized. C:
The fibular strut graft is placed with the intervertebral disc spaces
filled with bone graft. Bone graft is then placed from the flap to the
vertebral bodies.
described. Break the bony endplates with an angled Lambotte osteotome
or curet, and pack the entire disc space with rib graft (see Chapter 146, Chapter 155).
-
Clean all the intervening disc spaces and prepare each end vertebra of the curve as described in the strut graft technique.
-
Cut a trough in the interposed vertebral
bodies with large Luxsell and Adson rongeurs and curved curets. The
trough should be deep enough to bury the rib or fibular graft. -
The trough may also be filled with morcelized bone graft if anterior flexibility is needed during the posterior instrumentation.
-
Correct the kyphosis by pushing on the
apex of the curve, countersink the premeasured graft in the trough, and
lock it in the end vertebrae.
circumstances when early stabilization, earlier arthodesis, and shorter
immobilization are needed.
-
Determine the length of the vascular
pedicle needed. Measure the length of the strut graft that is needed on
the anterior portion of the rib and cut it free with a rib cutter,
leaving all soft tissue attached. -
Sharply dissect the neurovascular pedicle
back to the rib base to allow mobilization of the strut. Expose each
end of the strut subperiosteally for approximately 2 cm and impact and
countersink these graft ends in the prepared end vertebra of the
kyphosis, being careful not to kink the vascular pedicle (Fig. 161.13) (3).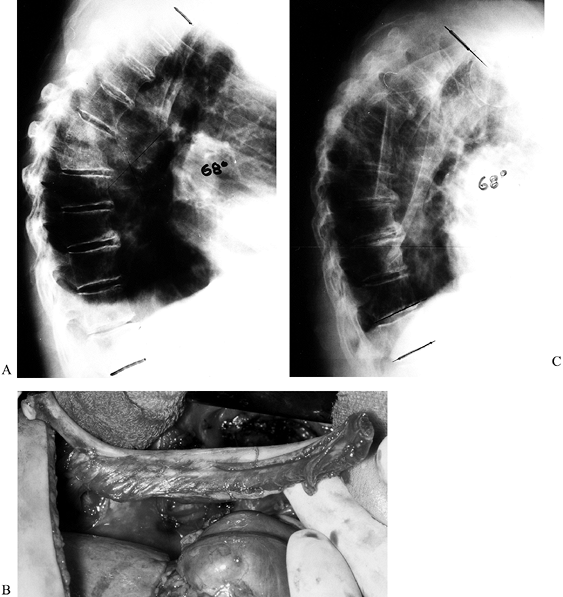 Figure 161.13. A: A 72-year-old man with vertebral osteomyelitis T-6–T-7. B: The vascularized rib graft with the neurovascular pedicle is at the left. C:
Figure 161.13. A: A 72-year-old man with vertebral osteomyelitis T-6–T-7. B: The vascularized rib graft with the neurovascular pedicle is at the left. C:
This postoperative radiograph shows the anchored vascularized rib
graft. Note the supplemental inlay and interbody grafts in the area of
the osteomyelitis.
vertebra in a type II congenital kyphosis, the remnant of the posterior
disc can be visualized. If the disc remnant cannot be visualized,
perform the osteotomy at the level of the vertebral foramina to allow
sagittal correction after the osteotomy.
-
Perform multiple vertebral osteotomies at
the levels of the posterior disc remnants or foramina using gouges,
osteotomes, and curets. A power burr can be helpful for a portion of
the osteotomy. -
Clean the disc spaces of all soft tissue back to the posterior annulus using curets and rongeurs.
-
Use angled curets to complete the osteotomy on the opposite side, back to the posterior annulus.
-
Check mobility of each intervertebral space with a Blount spreader, and pack each space with rib graft cut into small pieces (Fig. 161.14) (19).
![]() Figure 161.14. A: Type II congenital kyphosis. Note the posterior disc remnants in the area of the anterior bar. B: After osteotomy is completed with angled curets, gouges, and rongeurs. Mobility is then checked with a Blount spreader. See Figure 161.11 for the postoperative radiograph.
Figure 161.14. A: Type II congenital kyphosis. Note the posterior disc remnants in the area of the anterior bar. B: After osteotomy is completed with angled curets, gouges, and rongeurs. Mobility is then checked with a Blount spreader. See Figure 161.11 for the postoperative radiograph. -
Use intervertebral structural cages to
correct sagittal alignment and prevent vertebral collapse at the site
of the osteotomies. The longer kyphotic curves will also need strut
graft support.
-
Expose the anterior spine extraperiosteally on the convex side.
-
Using rongeurs and curets, clean the disc
space of its annulus fibrosus and nucleus pulposus, along with the
cartilage endplates at each vertebral level to be instrumented (the
same technique as an interbody fusion). -
Measure the vertebral body size with a caliper to determine the appropriate length of screw to be used.
-
Prepare a hole with a trocar in each vertebral body to be instrumented at the midlateral aspect of the rotated vertebra.
-
Insert a vertebral screw and washer, aiming each screw toward the opposite pedicle or anterior to the pedicle.
-
Take great care to identify the anterior
longitudinal ligament at each level so that the degree of vertebral
rotation is appreciated before the screw is inserted. -
Prepare the disc spaces for grafting by
breaking the bony endplates with an osteotome and curets to ensure good
cancellous bony exposure. -
Distract the disc spaces with a Blount spreader, and hold them open with whole-rib grafts.
-
After assembling the rod-and-screw construct, correct the sagittal deformity.
-
With the Zielke system, attach the
derotation bar and derotate the spine as the nuts are sequentially
tightened. As the spine is derotated, the scoliosis and rotational
kyphosis are corrected. -
With segmental rod-and-screw systems,
sequentially distract the intervertebral segments as the rod is
introduced into one screw at a time.
collapse and the development of sagittal kyphosis after derotation has
occurred. A supplementary posterior fusion and segmental
instrumentation is usually done as a second-stage procedure (Fig. 161.15).
 |
|
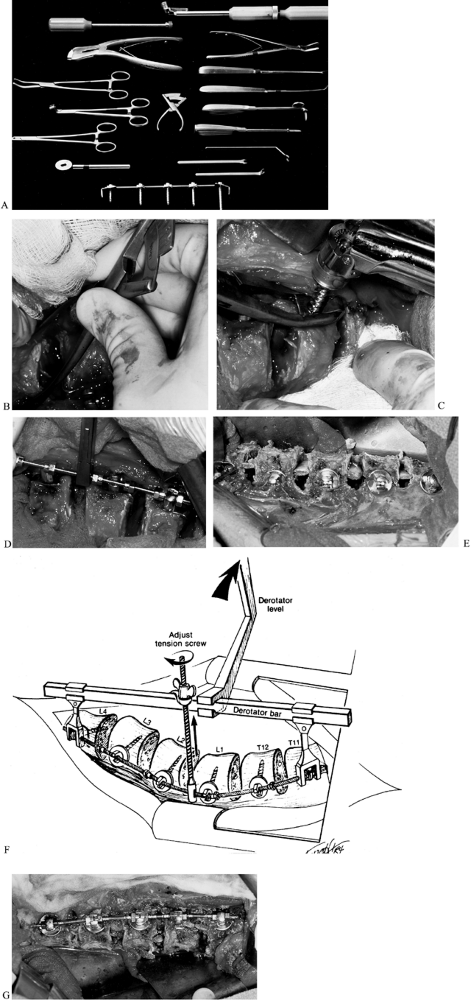
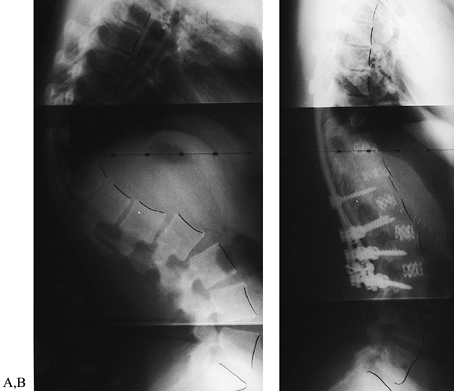
Figure 161.15. A: Zielke instrumentation. B: Measuring the vertebral size with a caliper. C: Inserting a vertebral screw with a plate (a washer may be used instead). D:
Rod insertion. Double nuts are used at the end of the construct and single nuts are used at other levels compressing toward the apex of the curve. E: Whole-rib grafts may be used to prevent collapse and sagittal kyphosis. Intervertebral cages may be useful in this situation. F: The derotator bar is used to pull the vertebral bodies back toward the sagittal plane, derotating the spine and correcting rotational kyphotic collapse. G: After derotation, the system is locked and the nuts are tightened. |
allograft dowels or rings as structural grafts has been useful in
correcting and maintaining correction of kyphosis. They unload the
posterior segmental instrumentation by participating in load sharing.
This combination creates a more rigid construct for arthrodesis. They
are especially useful in maintaining lumbar lordosis.
-
Expose the spine extraperiosteally and
create a flap of the annulus. Tag the flap with suture, then clean the
disc spaces of all soft tissue as previously described. -
The most useful cages are those that
allow abundant bony ingrowth through a mesh design and add sufficient
structural support. The allografts are hollow in the center for
autografts, for early bony ingrowth. -
Insert a wedge into the disc space and
impact it. Measure the height of the disc space and select the size of
the cage. Fill the cage or allograft with bone graft and insert and
impact it into place. -
Remove the wedge and insert the second cage or allograft.
-
Decorticate the remaining vertebral endplates and fill the remaining space with autogenous graft (20).
-
Reapproximate the annular flap and suture the margins together to act as a barrier for the bone graft.
used, depending on the circumstances; usually a single allograft is
sufficient. Follow the anterior procedure by a posterior arthrodesis
and segmental instrumentation (Fig. 161.16).
 |
|
Figure 161.16. A: Postlaminectomy sagittal thoracolumbar kyphosis from resection of an arteriovenous malformation. B:
Postoperative radiograph with intervertebral Harm’s cages used as structural intervertebral grafts and posterior segmental instrumentation [three-stage (posterior–anterior–posterior), same-day surgery]. (Images courtesy of Dr. Harry Schufflebarger, Miami, FL.) |
kyphosis are (a) segmental spinal instrumentation and Moe facet fusion
and posterior arthrodesis, (b) posterior spinal osteotomy, and (c) the
eggshell procedure.
now available, and most are strong enough to be acceptable. Which
system to use is based on the experience of the surgeon. It is
important to note, however, that some systems have a lower design
profile than others. It is important to minimize the prominence of the
instrumentation beneath the skin (see Chapter 156).
flatback syndrome, posterior osteotomies will be necessary for
correction. When the spine is also fused anteriorly, combined anterior
and posterior osteotomies will be necessary. The osteotomy site is
selected by locating the vertebral foramina across which the osteotomy
will be performed. The cranial–caudal width of the osteotomy is
determined by the degree of closure that is necessary. Multiple
osteotomies will spread the degree of correction across multiple levels
and reduce the risk of neurologic compromise as compared with a
single-level osteotomy. Single-level osteotomies can be useful,
however, in ankylosing spondylitis and in patients with paralysis.
-
Perform the osteotomy with osteotomes, gouges, curets, and Kerrison rongeurs (see Chapter 163). Remove the bone in sizable pieces and save them for later use as an autograft.
-
A power burr can be used, although bone
that can be used as an autograft is often lost. By attaching a Luken’s
trap to the suction system, much of the fine bone removed by the burr
can be recaptured. -
Carry the osteotomy down to the inner cortical table, which is then osteotomized with Kerrison rougeurs.
-
It is important to adequately decompress
the spinal canal and undercut the osteotomy at the edges of the canal
to prevent nerve root entrapment or central canal stenosis upon closure
of the osteotomy (10,17). -
Provide adequate fixation to maintain correction and prevent displacement of the osteotomy.
osteotomy should include removal of lamina, spinous processes, facets,
and bilateral pars interarticularis. The amount of bone removal is
determined by the degree of correction that is desired and that is
judged to be safe (7,16,17,21,22,24).
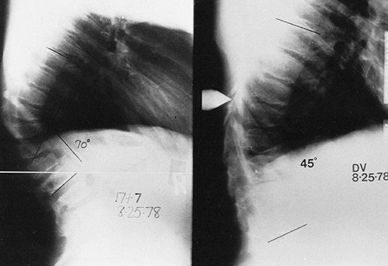
operative technique that allows the spine surgeon to operate on the
anterior thoracic or lumbar vertebral column through a posterior
approach. It is most useful caudal to T-6 because of the more rigid
conduit to the anterior spine (transpedicular vertebrectomy) (18).
This approach can be used for a vertebral biopsy or decompression of a
vertebral body abscess, but most eggshell procedures are done for
chronic or acute deformity. In deformity surgery, the eggshell
procedure is performed in addition to other procedures done for
correction, arthrodesis, and stabilization.
-
Position the patient prone on a spinal frame.
-
Prepare the spine for segmental posterior
instrumentation by inserting all hooks and screws in preparation for
stabilization at the time of deformity correction. -
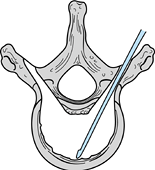
Locate the pedicle by plain radiographs
or image intensification. The location of the pedicle is identified by
the bifurcation of a line transecting the transverse process and a line
along the lateral margin of the pars interarticularis (Fig. 161.17).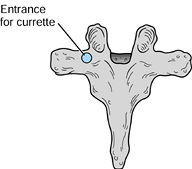 Figure 161.17. Entrance to the pedicle posteriorly.
Figure 161.17. Entrance to the pedicle posteriorly. -
Enter the pedicle with either a power
burr or osteotomes and curets. Introduce a small curet into the pedicle
and into the vertebral body. -
Enlarge the pedicle hole by progressively increasing the size of the curets.
-
Leave the posterior elements intact and
do not disturb the medial wall of the pedicles at this time. An
extension moment promotes kyphosis correction and posterior bone
removal may not be necessary. -
Use a sweeping motion to remove progressively more of the cancellous bone of the vertebral body.
-
The surgeon can operate at an angle of
approximately 45° from lateral to medial and decancellate an area
directly anterior to the spinal canal. -
Perform the same procedure through the opposite pedicle (Fig. 161.18) and continue until the desired amount of material (e.g., bone, tumor) is removed.
![]() Figure 161.18.
Figure 161.18.
The curet is in the vertebral body to perform decancellation. The
vertebral body is entered from both pedicles. An eggshell is created. -
To remove additional bone from just
anterior to the spinal canal, remove the lateral wall of the pedicle to
allow a more oblique angle for the curet to approach this area. Once
this is accomplished, an eggshell is created (Fig. 161.18). -
If correction of localized kyphosis is
planned, fracture the lateral wall of the pedicles and extend the
fracture into the shell of the vertebral body. An extension moment
applied to the spine may assist in this technique. If additional
correction is necessary, perform a sequential posterior decompression
by removing the spinous process, lamina, pars interarticularis, and
pedicles (Posterior Subtraction Osteotomy) (Fig. 161.19).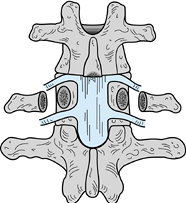 Figure 161.19. Complete posterior decompression is done.
Figure 161.19. Complete posterior decompression is done. -
Pack morcelized bone graft anteriorly before closing the osteotomy for anterior arthrodesis.
-
Complete this wedge osteotomy and use
segmental posterior instrumentation to correct the kyphosis and
stabilize the spine. When the posterior elements are removed, a slow
correction of the deformity is recommended to be sure that there is no
encroachment of bone on the spinal canal or malalignment of the
vertebra causing dural compression. Be careful of nerve root
impingement. -
The inferior and superior laminae need to be undercut to avoid impingement on the dura during closure of the osteotomy.
-
The axis of the closure of the osteotomy is anterior to the spinal canal, thus shortening the neural tube.
-
Stable posterior fixation is required to maintain osteotomy stability, kyphotic correction, and arthrodesis (Fig. 161.20).
![]() Figure 161.20. Extension of the eggshell osteotomy and posterior segmental fixation.
Figure 161.20. Extension of the eggshell osteotomy and posterior segmental fixation. -
The ultimate stability of the spinal construct depends on whether or not facet-to-facet or bone-to-bone apposition is obtained.
patients on egg-crate or air mattresses, and log-roll them frequently
to prevent decubiti and atelectasis. Prescribe daily bedside physical
therapy for muscle strengthening, and joint range-of-motion exercises.
Remove any chest tube and posterior drains on the second postoperative
day or when the drainage is minimal.
patient in a bivalved polypropylene body jacket. If the patient is a
teenager or young adult with good fixation and good-quality bone,
bracing may not be needed. If there is any question about the stability
of the instrumentation, bone weakness, or situations in which
instrumentation cannot be used in the cervicothoracic spine (e.g.,
achondroplasia, diastrophic dwarfism), use a halo brace. In cervical
kyphosis, apply a halo brace intraoperatively. Then allow patients to
ambulate in the brace.
anterior and posterior procedures at the same surgical setting to
minimize anesthesia and recovery times. Sometimes a staged procedure
may be indicated in patients who have had previously failed attempts at
correction with resultant pseudarthroses and progressive curves,
depending on the individual circumstances (19).
-
Failing to fuse the entire kyphotic curve
(fusion too short) may allow progression of the kyphosis. This is
especially true in children due to the adding-on phenomenon, in which
vertebrae cranially and caudally tilt into the curve and are added to
the curve. -
Placing the strut graft too far anteriorly with no bony contact with the apex of the kyphosis will lead to graft fracture.
-
Placing the anterior strut graft too far posterior to the weight-bearing axis may lead to failure and progressive deformity.
-
Failure to supplement an anterior
procedure with a posterior fusion and instrumentation may lead to
inadequate correction or late failure. -
Inadequately countersinking the strut graft may result in graft dislodgement after surgery.
-
Failure to make osteotomies wide enough
and the vertebral canal edges round enough may lead to nerve root
entrapment at osteotomy closure. -
Dural, spinal cord, and nerve root injuries from too aggressive disc removal can occur.
-
Inadequate disc removal will lead to failed fusion or to late progression of the deformity.
-
Focusing on spinal instrumentation and inattention to fusion technique may lead to pseudoarthrosis and failure.
-
Inadequate placement of posterior
instrumentation may result in incomplete correction or an unbalanced
torso, and failure to maintain lumbar lordosis below the kyphosis will
lead to unbalanced sagittal alignment. -
Too-vigorous correction of the kyphotic
deformity with posterior instrumentation in osteopenic bone can lead to
bony failure, with loss of fixation and correction. -
Too-vigorous derotation with the Zielke instrumentation can cause spinal root injuries.
-
With any anterior instrumentation, take care to prevent flatback syndrome.
-
When there is severe vertebral rotation, anterior screw placement is critical so that spinal canal penetration does not occur.
-
Finally, a well-applied brace is
extremely important in some patients and should not be delegated to the
inexperienced surgeon, or a less-than-ideal result may occur in an
otherwise masterfully performed surgical procedure.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
DS. Spondylolysis and Spondylolisthesis in Children and Adolescents:
Current Concepts in Management. In: Bradford DS, Hensinger RM, eds.The Pediatric Spine. New York: Thieme, 1985;416.