OPERATIVE TREATMENT OF THORACIC AND THORACOLUMBAR FRACTURES
VIII – THE SPINE > Trauma > CHAPTER 142 – OPERATIVE TREATMENT OF
THORACIC AND THORACOLUMBAR FRACTURES
the forefront of fracture management in the spine. Techniques and
implants have evolved to provide better results with decreased
morbidity and mortality (1,9,11,13,17), and current operative management more rapidly returns the patient to work and satisfactory function (9,10,20,86). Changes in health care management and patient expectations have made prolonged bed rest or immobilization unacceptable (12).
Improved imaging, a better understanding of fracture and implant
biomechanics, and the introduction of a variety of new anterior and
posterior fixation devices allow surgeons to plan definitive
stabilizing procedures for any fracture pattern, allowing rapid
mobilization and return to function. Hence, patients who cannot be
mobilized in a cast or brace within a few days
of their injury are often more reasonably treated with surgery.
-
Protect neural elements, restore/maintain neurological function;
-
Prevent or correct segmental collapse and deformity;
-
Prevent spinal instability and pain;
-
Permit early ambulation and return to function; and
-
Restore normal spinal mechanics.
rest can be treated nonoperatively in a brace, molded orthosis, or
hyperextension cast. Single-column injuries (e.g., compression
fracture, laminar fracture, spinous process fracture) are treated in an
off-the-shelf brace that encourages normal spinal alignment and limits
extreme motion (Fig. 142.1). More significant
compression fractures may be treated in a molded orthosis. Two-column
injuries, including severe compression fractures, mild to moderate
burst fractures, and bony Chance fractures, are too unstable to be
braced but may well be reduced and maintained at bed rest or in a
hyperextension cast. Previous studies (84) have
shown that even severe burst fractures can be treated with a regimen of
bed rest, postural reduction, and casting. Bony remodeling reduces
residual canal compromise by more than 50% over the course of a year (71) (Fig. 142.1),
making surgical treatment unnecessary in many patients, including those
with retropulsed fragments in the spinal canal. Recumbent treatment,
although effective, is very expensive and rarely reimbursed or
permitted in managed care systems. Hyperextension casting, on the other
hand, allows immediate mobilization and early return to independent
function.
 |
|
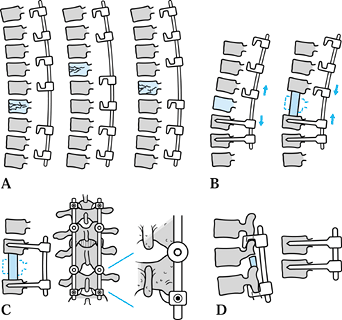
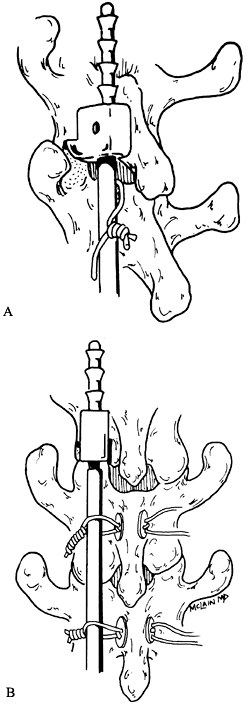
Figure 142.1. Fracture remodeling. A:
Thoracic level burst fracture. With nonoperative treatment, normal remodeling mechanisms tend to restore canal diameter compromised by retropulsed bony fragments. B: Resorption of the retropulsed vertebral body results in a “heart-shaped” canal with near-normal anteroposterior (AP) diameter 1 year later. (Courtesy Joseph Mumford, MD, Topeka, KS.) |
 |
|
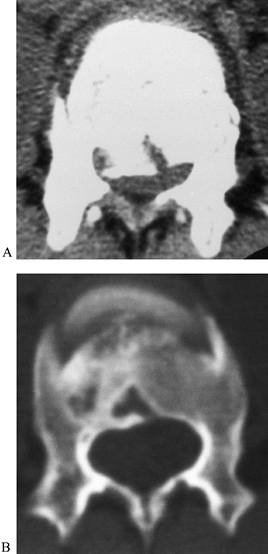
Figure 142.2. Closed reduction and hyperextension casting of thoracolumbar fractures.
|
-
Place the patient on a modified fracture table (Fig. 142.2A).
Suspend the patient on a narrow, midline, taut canvas support in
cervical halter traction, with arms out to the side, knees flexed, and
feet resting on the support to give the patient a sense of balance. -
Apply a vertically directed force that will achieve hyperextension at the fracture site (Fig. 142.2B).
Once maximum hyperextension is achieved through this means, relax the
horizontal canvas support and place additional traction on the iliac
crests. -
After satisfactorily positioning the patient on the table, wrap the torso with Webril (Fig. 142.2C). Pad the bony prominences additionally with foam and apply the cast.
-
Note the extreme hyperextension placed into the cast, as well as the large anterior abdominal hole that has been created (Fig. 142.2D, Fig. 142.2E).
Send the patient to the x-ray department for postreduction and casting
x-ray studies. If satisfactory alignment has been achieved, allow the
patient to ambulate immediately.
transferred posteriorly through the facet joints, allowing immediate
weight bearing and good restoration of sagittal alignment and vertebral
body height. In Chance fractures, hyperextension closes the posterior
defect and approximates the fracture margins. The cast cannot be placed
until the abdomen is cleared and any ileus or distention has subsided,
however, limiting its use in polytrauma patients. Patients with
abdominal trauma, prolonged ileus, chest trauma, or multiple extremity
fractures may not be suitable for casting for some time after
admission. Once the abdomen is cleared and a well-molded cast is
applied, the patient may begin transfers and ambulation. Braces and
removable orthoses cannot generate the hyperextension forces necessary
to maintain sagittal alignment and should not be considered substitutes
for a well-molded hyperextension cast. Also see Chapter 10.
First, immediate spinal stability is provided for patients who can
tolerate neither a cast or prolonged recumbency. Prolonged recumbency
in multiply injured patients predisposes them to severe and
life-threatening complications. Prompt surgical stabilization allows
the patient to sit upright, transfer, and start rehabilitation earlier,
with fewer complications (14,31,42).
Second, surgical treatment more reliably restores sagittal alignment,
translational deformities, and canal dimensions than does cast
treatment. And, finally, surgical decompression more reliably restores
neurologic function and decreases rehabilitation time (16,23,52,72).
injuries, are typically stable, and rarely cause neurologic injury. A
hyperextension orthosis or chair-backed brace is sufficient to allow
ambulation and return to limited activity. Fractures with more than 50%
collapse of the anterior vertebral body or with more than 20° of
sagittal angulation are considered potentially unstable. A computed
tomography (CT) scan may be necessary to distinguish these injuries
from a burst fracture. Severe compression fractures can be treated with
a hyperextension cast, although some may require posterior
instrumentation and fusion.
treated in a hyperextension cast if the patient has no abdominal or
thoracic injuries. Unstable injuries typically require operative
reduction and stabilization.
-
Burst fractures that are considered unstable include
-
Greater than 50% axial compression.
-
Greater than 20° angular deformity.
-
Multiple contiguous fractures.
-
Neurologic injury—complete, incomplete, or root.
-
Three-column injuries and dislocations.
-
Patients with extensive associated injuries.
-
Greater than 50% canal compromise at L-1 and 80% compromise at L-5.
decisions are based on issues of mechanical stability and sagittal
alignment primarily, and canal compromise secondarily. In the thoracic
region, sagittal deformities are corrected by longitudinal distraction,
which may also indirectly reduce some retropulsed vertebral fragments
from the spinal canal. In the lumbar region, forceful distraction tends
to reduce lumbar lordosis, introducing sagittal imbalance and a flat
back. Forceful distraction in a patient with a three-column injury may
inadvertently lengthen the spinal column and stretch the spinal cord,
causing neurologic injury. Segmental spinal systems now allow segmental
distraction within the construct while neutralizing construct length
and sagittal alignment (Fig. 142.3). The segmental
fixation system allows multiple points of fixation, to distribute
reduction forces more evenly. Posterior systems cannot resist sagittal
deforming forces if the anterior spinal column is deficient, however (70).
Thoracolumbar and lumbar fractures with severe collapse and vertebral
comminution tend to lose correction over time unless anterior
instability is corrected. Patients with sagittal collapse tend to have
more pain and may develop new neurologic symptoms if kyphosis
progresses (27,70).
 |
|
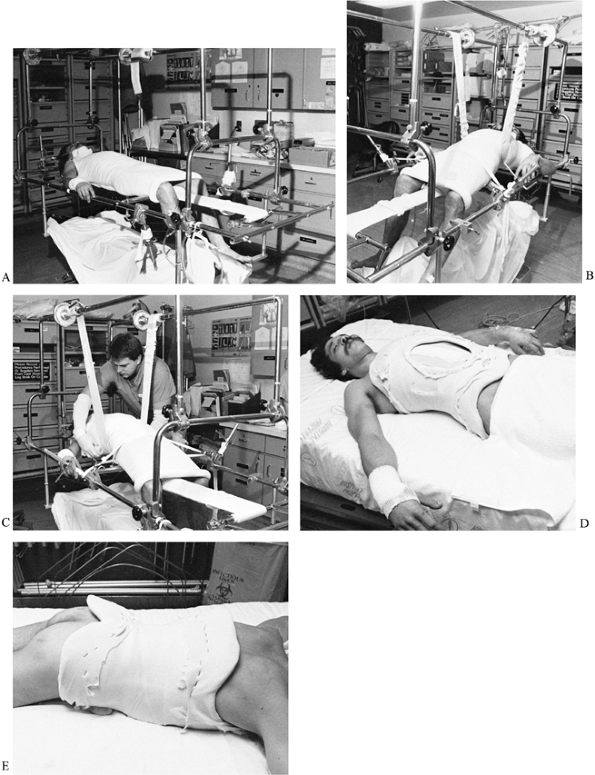
Figure 142.3.
Segmental fixation allows the surgeon to neutralize the overall length of the spinal segment, preventing overdistraction, and segmentally distract or compress segments within the construct to either decompress the fracture site or compress an anterior graft. |
fracture, but it becomes the primary concern only when a high degree of
compromise is recognized. Residual compromise greater than 50% is
worrisome at the T12–L1 level, where the conus medullaris and cauda
equina fill the spinal canal (Fig. 142.4).
Small increments of axial or sagittal collapse can compromise
neurologic elements, and anterior decompression and stabilization
should be considered for both mechanical and neurologic reasons. On the
other hand, 80% to 85% canal compromise may be well tolerated in the
lower lumbar spine, where only a few roots remain in the otherwise
capacious canal (40). Retropulsed bony fragments reabsorb and remodel over time, and do not need to be addressed in their own right (70).
Sagittal collapse and kyphosis of a moderate degree is usually well
tolerated in the thoracic region, and does not require aggressive
reconstruction. Lower lumbar burst fractures are also well tolerated,
and most have a satisfactory outcome without reconstruction. Canal
compromise, sagittal imbalance, and segmental kyphosis are all poorly
tolerated at the thoracolumbar junction, which is, unfortunately, the
most common site of fracture.
 |
|
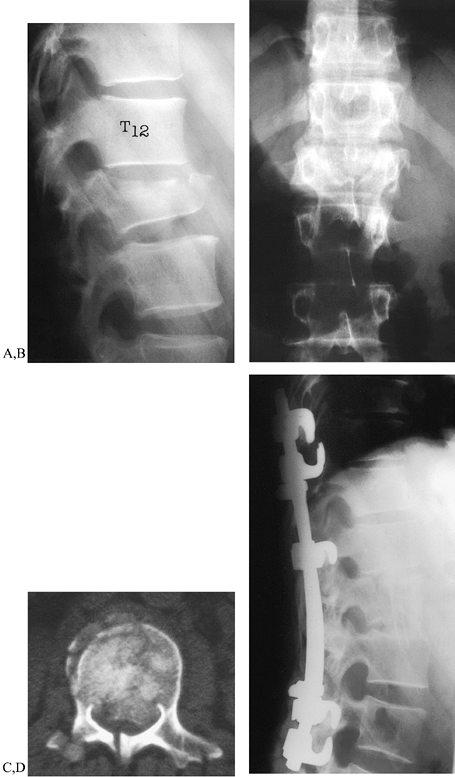
Figure 142.4.
Burst fracture: 32-year-old man fell 35 feet, sustaining severe L-1 burst fracture (Denis type B) and an open tibial shaft fracture. A, B: Lateral and AP radiographs demonstrate loss of vertebral height and widening of the pedicles, with little kyphosis. Cortical retropulsion is difficult to appreciate on plain radiograph. C: Computed tomography demonstrates severe comminution and canal compromise. A fracture of the lamina is also seen. Even though the patient was neurologically intact, the 75% compromise at the L-1 level seen here was considered too severe, and the spine, unstable. D: Anterior vertebrectomy was followed by strut graft reconstruction, restoring anterior column support and thoracolumbar alignment. Posterior segmental instrumentation stabilizes the spine; the intermediate, down-going hook compresses and entraps the anterior strut. The patient had a full recovery and returned to work and sports without restrictions. |
treatment is carried out to protect residual function, restore
neurologic deficits, and allow early mobilization and rehabilitation
without a cast. If the cord or cauda equina injury is incomplete,
neurologic decompression can significantly improve the eventual outcome
(16,33,61), assuming that there is significant residual compression at the time of surgery (Fig. 142.5).
If no residual compression exists, posterior stabilization is carried
out alone. If the neurologic injury is complete, anterior surgery will
not improve the chance of neurological improvement but may be indicated
to treat sagittal deformity or instability. Posterior instrumentation
is usually adequate to allow immediate transfers and early
rehabilitation.
 |
|
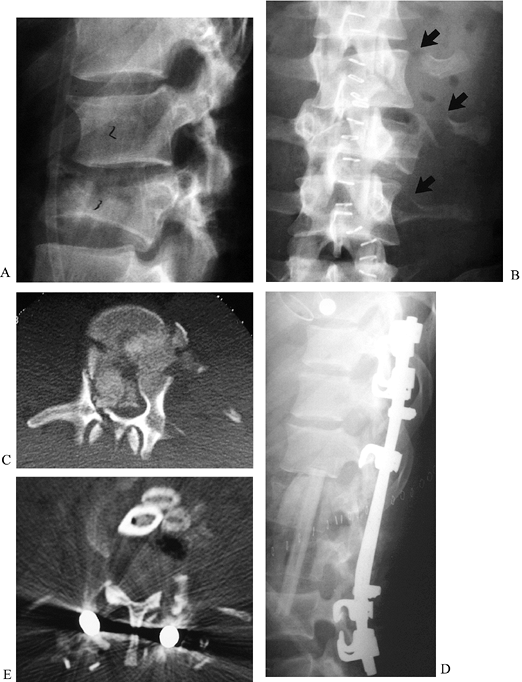
Figure 142.5.
Burst fracture-contiguous levels: 18-year-old man, status post motor vehicle accident, sustained L-2 and L-3 burst fractures with incomplete cauda equina injury. A, B: Lateral and AP radiographs. Multiple transverse process fractures suggest extent of soft-tissue trauma. C: CT of L-3 demonstrates greater than 80% canal compromise, laminar fractures, and extensive comminution. L-2 was less disrupted but unable to support an anterior strut. D: Lateral radiograph following L-2 partial and L-3 total vertebrectomy, followed by fibular autograft reconstruction. Construct was stopped at L-4 to spare the subjacent discs. At 4-year follow-up, the patient had normal neurologic function and minimal, intermittent back pain. E: Postoperative CT of patient following anterior decompression and reconstruction with autograft fibula and rib. The entire vertebral body has been removed from pedicle to pedicle, and all fragments have been removed from the canal. The patient had full neurologic recovery. |
segments (24,25 and 26,44,79).
Two-column injuries occurring through bone heal reliably and may well
be treated in a hyperextension cast. Ligamentous injuries do not heal
reliably and more often result in residual instability and pain. These
injuries are best treated with a short compression construct and
posterior fusion, as are patients with abdominal injuries in patients
who cannot tolerate a cast (Fig. 142.6).
 |
|
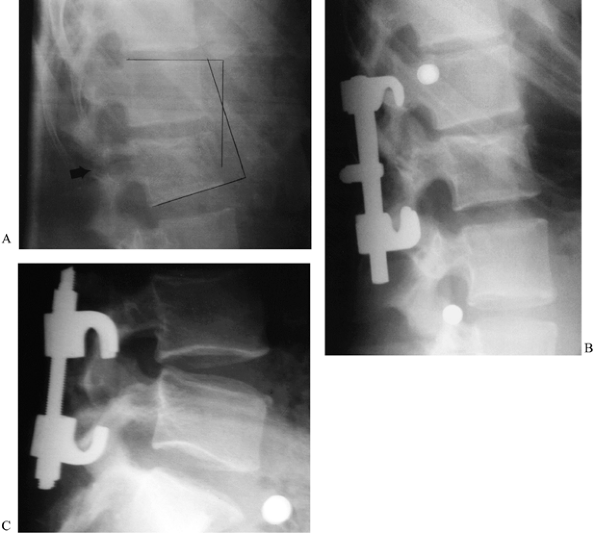
Figure 142.6.
Flexion-distraction injury—Chance fracture: 23-year-old with seat belt injury. The patient was neurologically intact but sustained severe internal injuries requiring colostomy. A: Lateral radiograph demonstrates focal kyphosis, expanded vertebral height, and transpedicular fracture line associated with Chance fracture. B: Because of abdominal injuries, casting was not possible. Operative reduction and fusion were carried out using a segmental fixation system. Reduction was obtained by positioning the patient in lordosis, manipulating the spinous processes to reduce displacement, and sequentially compressing the rod/hook construct until the fracture was closed and facets tightly compressed. C: A similar fracture treated with threaded Harrington compression rods. |
unstable. The incidence of spinal cord injury is high, as is the
incidence of intra-abdominal injury, necessitating a more aggressive
surgical approach. Pedicle instrumentation or extended segmental
constructs are often needed to stabilize these fractures.
trauma (motor vehicle accidents and falls from height) and are
typically associated with severe neurologic damage and multiple
associated injuries (67,74,75).
Complete spinal cord lesions do not improve with surgery, but mortality
and morbidity are both improved by early mobilization and
rehabilitation. Cauda equina lesions are less predictable than thoracic
lesions (some improvement may be seen), and restoration of spinal
alignment is indicated to stabilize the spine and to decompress
entrapped and compressed roots.
making a surgical decision. Delaying treatment affords no benefit to
the patient but may allow the surgeon to assemble a more skilled team
of personnel. If the patient is stable, neurologically intact, and not
suffering from multiple injuries, it is safe and reasonable to schedule
surgery for the next elective opportunity. On the other hand, morbidity
or mortality are not increased by taking the patient to the operating
room on an emergent basis, and in some instances, an emergent
stabilization may prove instrumental in the patient’s overall
management.
with severe chest trauma and pulmonary contusion may deteriorate
rapidly after hospitalization. Recumbency frequently leads to
hypoventilation, pneumonia, and sepsis, irrespective of antibiotic
prophylaxis, making delayed stabilization impossible. Pneumonia and
respiratory insufficiency will not clear until the patient can be set
upright, so a vicious circle is initiated that may take weeks to
resolve or may even take the patient’s life. Early stabilization
(12
to 24 hours) allows aggressive pulmonary toilet, upright positioning,
and limits time on the ventilator and in the intensive care unite
(ICU), reducing the likelihood of nosocomial infection. Indications for
urgent or emergent stabilization include
-
Severe chest trauma, pulmonary contusion.
-
Polytrauma, with multiple injured systems or long-bone fractures.
-
Progressive neurologic deficit.
-
Fracture dislocation in a patient already undergoing emergency surgery.
-
Fracture dislocation or deformity threatening skin breakdown.
patients, perioperative and postoperative morbidity were not increased
by emergent stabilization, but neurologic improvement was increased and
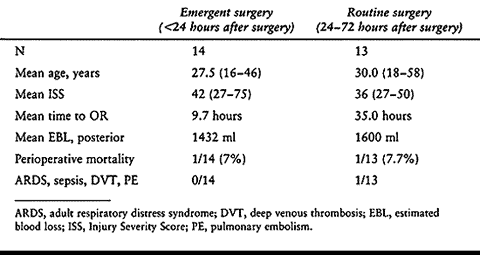
life-threatening complications were reduced (70a) (Table 142.1).
Note that overall mortality is this study was significantly less than
predicted by the high Injury Severity Score (ISS), where an ISS of
greater than 40 typically results in a 50% mortality rate in this age
group.
 |
|
Table 142.1. Polytraumatized Patients Undergoing Surgical Decompression or Stabilization on an Emergent or Routine Basis
|
the presence of spinal instability, instrumentation is almost always
incorporated into the surgical plan. The type of instrumentation used
depends on the injured level, the fracture pattern, the need for
anterior stabilization or decompression, and the surgeon’s level of
experience and training.
-
Nonsegmental rod/hook systems (Harrington rod).
-
Hybrid systems (Luque; Harrington rod with sublaminar wires).
-
Segmental systems.
-
rod/hook constructs
-
extended pedicle screw constructs
-
short-segment pedicle instrumentation (SSPI)
-
compression instrumentation
-
-
anterior screw/plate or screw/rod instrumentation
spinal systems but can still play a role in fracture stabilization,
primarily in the thoracic spine. Applied properly, Harrington
distraction rods can reduce angular deformity, restore vertebral body
height, and provide adequate stiffness to allow early mobilization (5,41,52,54).
Fixation is dependent on strong distraction forces between the superior
and inferior hooks, however, and constructs must span a number of
vertebrae to provide optimal corrective forces. Constructs that span
three levels above and two below the injury are biomechanically
superior to shorter constructs. Three-column spinal injuries cannot
resist the distraction forces of the Harrington rod, however, and rods
placed in these injuries will either overdistract the spinal column or
will not be firmly fixed.
body (60).
Because there are only two points of fixation on each rod, forces tend
to concentrate at those points, and lamina fracture or hook
dislodgement are frequent, leading to complete loss of fixation (32,36,82).
improves fixation of the Harrington rod and limits the risk of hook
displacement (55). Spinous process wires are
less likely to pull sublaminar hooks into the canal, but well-fitted
hooks are unlikely to displace with either technique (Fig. 142.7).
These constructs are best suited to fractures of the midthoracic spine,
where extended fusions are relatively well tolerated. Although the
addition of sublaminar segmental wires has improved the sagittal and
torsional stiffness of Harrington constructs (3,19,63,81,85),
it has not eliminated rod breakage. Luque instrumentation may prove
useful in some thoracic fractures but does not provide sufficient axial
stability to treat burst fractures.
 |
|
Figure 142.7. Harrington rod fixation for thoracic fractures. Harrington rods, supplemented with sublaminar wires (A) or interspinous wires (B), provide sufficient rigidity and stability to treat many thoracic level fractures and fracture dislocations.
|
results for a variety of spinal disorders. Originally intended for
scoliosis patients, segmental hook and rod systems have now been used
to successfully treat trauma, infections, tumors, and degenerative
disorders (51,59,76).
Clinical series have documented the efficacy and technical demands of
segmental systems in scoliosis, kyphosis, and congenital deformities,
and have provided the clinician with enough information to develop
rational and reliable treatment plans. Such principles have not been as
well established for fracture treatment, however.
frequency for thoracic and thoracolumbar spine fractures, but only a
handful of clinical studies have been published to support this
application (47,64,80). McBride reported good results in thoracic and thoracolumbar fractures treated with longer hook and rod constructs (64,65), and SSPI constructs have been endorsed for treatment of lumbar fractures (7,20).
Enthusiasm for SSPI has been tempered somewhat by recent studies
identifying a high rate of screw failure in unstable fractures (4,8,69,70), however.
three-point bending mechanics to reduce and maintain thoracic kyphosis
and prevent translation of disrupted vertebral segments. The success of
this strategy has been documented in nonsegmental systems (Harrington
rods), and a number of construct patterns have been presented for
segmental systems (64,65,80).
Although they use the same basic reduction strategy as the Harrington
rod, segmental rod/hook systems offer several unique advantages over
first-generation instrumentation systems (6,39,49):
-
Proximal and distal hook pairs (claws) provide more stable fixation than the Harrington hooks they replaced.
-
Segmental systems are not dependent on strong distraction forces for purchase.
-
Contact between the rod and the lamina still provides correcting forces in the sagittal plane.
-
Segmental systems allow placement of
intermediate hooks, thus distributing corrective forces over more
laminae and reducing the likelihood of hook pull-out or fixation
failure. -
Segmental constructs are stiffer than Harrington rods in both axial and torsional loading.
with absent or fractured laminae directly. They provide three-column
fixation in unstable injuries and limit the length of fusion in the
lumbar spine (50). Pedicle screws may be used
exclusively or in combination with hook constructs to address a wide
variety of fracture patterns. Combined (or “extended”) constructs are
particularly useful at the thoracolumbar junction. Here, the thoracic
spine is relatively immobile and tolerant of fusion. Extending the
construct into these segments incurs little mechanical cost and
provides more extensive fixation. This improved proximal fixation
allows the surgeon to apply enough corrective force to restore sagittal
alignment, an imperative at the thoracolumbar junction. Pedicle screws
are then applied in the upper lumbar segment to limit the length of the
construct, minimizing interference with lumbar motion segments.
Extending fusion into the lower lumbar spine does alter mechanics and
predisposes patients to junctional pain and subsequent degeneration.
intermediate hook applied just above the fracture and just below the
upper claw, and directed either cranially or caudally, depending on the
situation. In most constructs, a narrow-width hook is placed up-going
under the lamina of the vertebra two levels above the fracture. With
the upper and lower fixation points locked in place to neutralize the
construct length, this hook allows segmental distraction of the
fracture to improve vertebral height and decompress the spinal canal
indirectly without overdistracting the spine. In anterior and posterior
reconstructions, this additional hook may be directed downward to
compress and capture the anterior strut graft.
lumbar spine and provides sagittal, axial, and torsional stability
superior to rod/hook constructs or sublaminar wiring (49,50).
Fixation is not dependent on intact lamina, so there is no need to
extend the fusion in cases of laminar fracture or laminectomy. Because
distraction is not needed to correct the axial deformity, the risk of
either overdistracting the disrupted segment or producing a flat-back
syndrome is lessened. Both the surgical and mechanical disturbance to
the adjacent lumbar segments is minimized. Nevertheless, SSPI is
limited in its ability to maintain sagittal correction in severe burst
fractures (7,69,70).
If the anterior and middle spinal columns cannot share axial loads, the
bending moments generated at the pedicle screw hub result in a high
rate of bending failure or fracture. Once initial bending has occurred,
progressive collapse is more likely, with progressive loss of lordosis
in some patients.
developed over the past 10 years, all based on the principle of
anterolateral screw fixation coupled with longitudinal plates or rods (Fig. 142.8).
These devices can span multiple segments and can be applied from the
midthoracic region down to the L-5 vertebral body. They are intended to
augment anterior column reconstruction, providing torsional and
translational stability while sharing axial loads with a strut graft or
cage (see Chapter 137). When posterior soft
tissues and structures are intact, an anterior reconstruction and
instrumentation may be adequate to stabilize the spine. If the
posterior elements are disrupted, however, the anterior construct is
likely to fail unless posterior instrumentation is carried out as well.
 |
|
Figure 142.8. Anterior instrumentation for burst fracture treatment.
|
spinal alignment is corrected at the time of fixation. Failure to
correct sagittal alignment will result in a fixed kyphotic
deformity,
predisposing the patient to dysfunction, pain, and instrumentation
failure, and necessitating late revision and reconstruction. Failure to
correct translational deformity will result in a residual stenosis at
the level of offset, and may predispose the patient to nonunion and
treatment failure.
dislocation injuries is kyphosis. If this deformity is allowed to
persist, it will become fixed and irreducible, but immediately after
fracture, fragments are typically mobile and amenable to indirect
reduction.
-
If nonoperative treatment is planned, place the patient supine over a bolster until provisional healing has occurred (84)
or until the patient is ready for casting. For operative care,
accomplish reduction by properly positioning the patient on the
surgical frame. -
Return fractures of the thoracic spine to
normal kyphosis by placing the patient on a Wilson frame, adjusted to
fit the patient’s chest wall. Avoid hyperextension. -
Reduce fractures of the lower lumbar spine on either a Wilson or a fracture frame.
-
Carry out instrumentation of the shortest
possible segment with the hips extended and the torso positioned
comfortably on the frame of choice.
-
Position the patient gently and carefully
in the prone position, with support under the iliac crests distally and
the anterior chest wall proximally. Allow the abdomen and midtrunk to
hang free. -
Options for positioning include
transverse bolsters, the Relton-Hall type frame, and the Jackson
turning frame. The Jackson turning frame allows the surgeon to position
bolsters, arm boards, and headrest with the patient supine and awake,
then turn the frame and patient as a unit without further repositioning
(Fig. 142.9). A Wilson frame attachment is also available.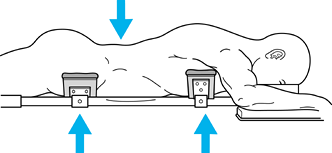 Figure 142.9.
Figure 142.9.
Postural reduction of burst and flexion distraction injuries. Normal
thoracolumbar lordosis can be restored by placing patient on a spinal
frame supporting the torso and pelvis and allowing the abdomen to hang
free. Further elevating the thighs will increase the lordosis in
segments adjacent to the fracture, which helps in restoring normal
alignment. -
As the abdomen and lower torso hang free, normal lumbar lordosis is accentuated, reducing the kyphotic deformity.
-
Because postural reduction does not
completely reduce the kyphosis of a severe burst fracture, it is
incumbent on the physician to recognize residual deformity
intraoperatively and manually restore thoracolumbar alignment at least
to neutral position.
necessary to manipulate the spine operatively. Two options are
available. First, in situ contouring of the implants can restore lordosis to segments that are not completely reduced passively.
-
Contour standard rod and screw or plate and screw constructs in situ
to restore sagittal balance, or contour the rod before placement and
then insert and rotate it into sagittal orientation to increase
lordosis. Take care not to overpower and damage the implants, however. -
Supplement pedicle screws by offset laminar hooks before attempting vigorous contouring.
-
Implants designed specifically for
fracture reduction are available; they are designed to neutralize
construct length at the same time that manipulation of the pins
corrects sagittal collapse (7,30,37,38).
thoracolumbar region. Transpedicular instrumentation systems limit the
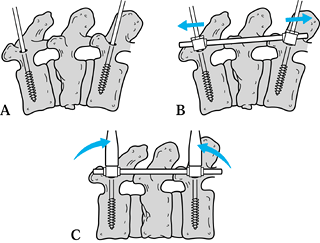
extent of the spinal fusion to a few levels, and allow direct reduction
of deformity. Figure 142.10 illustrates the use of SSPI:
 |
|
Figure 142.10. Short-segment pedicle instrumentation. See text.
|
-
After obtaining the best postural reduction, place screws according to anatomic landmarks and fluoroscopic control (step A).
-
Apply the fixation rod and carry out
gentle axial distraction to restore the normal height and alignment of
the posterior elements (step B). -
Restore lordosis by levering the dorsal extensions of
P.3737
the screws together to distract the anterior and middle columns back to
their normal height (step C). The sagittal rotation force applied at
the screw-rod connection will further lengthen the posterior column as
well, so avoid overdistraction during step B. -
Then tighten the locking nuts to fix both the axial and the sagittal correction.
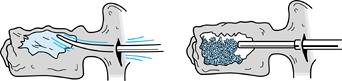
directly through a posterolateral approach. Using this method, the
surgeon elevates the depressed endplate through a transpedicular
approach and reinforces the fracture site with a transpedicular bone
graft (Fig. 142.11).
 |
|
Figure 142.11. Transpedicular bone graft. See text.
|
-
To restore the anterior weight-bearing
column without strut–graft reconstruction, carry out a transpedicular
reduction and grafting. -
Using a specially designed
instrumentation set (Synthes NA, Paoli, PA), directly elevate the
fractured endplate using a transpedicular approach. -
Impact fracture fragments into the fracture defect or remove them through a transpedicular decompression.
-
Impact additional graft, harvested from
the pelvis using an acetabular reamer, into the anterior half of the
vertebral body using a transpedicular funnel and stylet.
reduction to restore alignment. Fracture-dislocations are usually
reduced easily because the soft tissues are completely disrupted. If
part of the facet capsule or posterior longitudinal ligament is intact,
manual reduction is more difficult. In such a case, in a neurologically
intact patient, use a burr to take down the locked facet and allow a
gentle reduction without overdistracting the spine (Fig. 142.12).
 |
|
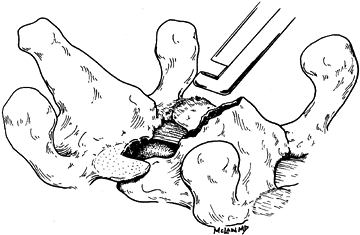
Figure 142.12.
Reduction of fracture-dislocation. When simple distraction cannot easily reduce a dislocated facet in a neurologically intact patient, resection of the overlapping articulation with a Kerrison rongeur or burr will allow gentle reduction. |
instrument only those segments intended for fusion, the routine
practice is to fuse all instrumented segments. Long rod/short fusion
constructs have been only marginally successful at protecting lumbar
segments in fracture patients (3), and newer
systems allow surgeons to avoid instrumenting the lower lumbar spine
altogether. This technique eliminates the need for a second surgery to
remove the hardware and avoids concerns over degenerative changes seen
in immobilized, unfused facet joints (21,56).
-
Observe meticulous fusion technique to avoid pseudarthrosis.
-
After stabilizing the fractured segment,
decorticate laminae, and transverse processes, take down the facet
joints, and liberally dress the lateral and dorsal surfaces with
autologous iliac crest graft. -
Concentrate corticocancellous strips of
autograft bone across the fractured segment and around the construct
ends, which are typical areas of fusion failure. -
Take care to preserve the adjacent facet joints and avoid extending the fusion beyond the instrumented segments.
-
Stable thoracic compression and burst
fractures may be treated in a Jewett brace or thoracolumbar sacral
orthosis (TLSO) with good results. -
Multilevel compression or burst fractures
will collapse into further kyphosis; instrument either with a
Harrington rod and Drummond wires or with a segmental rod/hook
construct. If the Harrington system is used, follow the old rule of
“three above, two below,” with spinous process wires placed at each
intact laminar level. -
Contour the rods to fit the thoracic
kyphosis better but leave them somewhat straighter than the desired
alignment to provide a third reduction force where the rod contacts the
spinal laminae.
-
For compression fractures, place a simple transversopedicular claw (Fig. 142.13) above and below the fracture level.
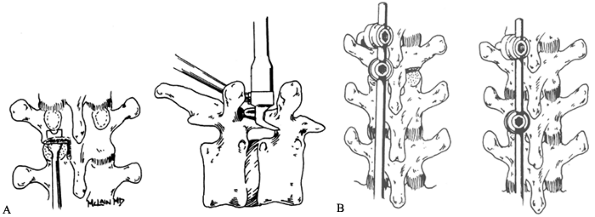 Figure 142.13. Proximal fixation patterns. A: Proximal transversopedicular claw constructs mirror those applied in adult deformities. B: In osteoporotic bone, or when the transverse process has been broken, a laminolaminar claw can be substituted.
Figure 142.13. Proximal fixation patterns. A: Proximal transversopedicular claw constructs mirror those applied in adult deformities. B: In osteoporotic bone, or when the transverse process has been broken, a laminolaminar claw can be substituted. -
In more severe fractures, use additional
claws and intermediate hooks to provide secure fixation and allow
intersegmental distraction. -
The rod/hook construct should take
advantage of three-point bending mechanics to reduce and maintain
thoracic kyphosis and prevent translation of disrupted vertebral
segments.
fixation than the Harrington hooks they replace and are not dependent
on strong distraction forces for fixation.
distribute corrective forces over more laminae, reducing the likelihood
of hook pull-out and fixation failure.
-
Arrange hooks to accommodate the regional
anatomy and the fracture pattern, as long as at least two hooks are
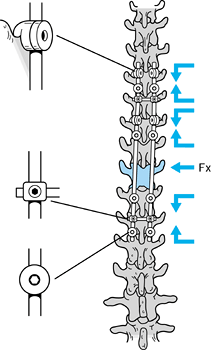
applied on either side of the fracture (Fig. 142.14A, Fig. 142.14B, Fig. 142.14C and Fig. 142.14D).![]() Figure 142.14.
Figure 142.14.
Construct patterns for posterior instrumentation: Four basic construct
patterns have been applied in thoracic, thoracolumbar, and lumbar
fractures, with or without anterior reconstruction. A:
Upper and lower hook patterns used primarily in the thoracic segments
but sometimes in the thoracolumbar segments. These consist of claw
configurations above and below the fractured level, with supplemental
hooks applied as an additional claw above the fracture in lower
thoracic fractures (1), below the fracture in upper thoracic fractures (2), and across the fracture in the midthoracic region (3). B:
Extended pedicle screw patterns used at the thoracolumbar junction.
Pedicle screws placed below the fractured level are supported by offset
laminar hooks or additional screw fixation at the level below. Proximal
fixation is provided by a claw construct carried to the lower thoracic
segment. A supplemental hook is placed above the fracture, providing
distraction against the lumbar screws when an indirect reduction is
desired (1), and compressing the anterior graft when a direct decompression has been performed (2). C:
Short-segment pedicle instrumentation (SSPI) patterns used in
thoracolumbar and lumbar fractures to limit fusion. Specifically
designed constructs are available, or SSPI constructs can be designed
from standard instrumentation sets. If the anterior column is unstable,
protect posterior screws with an anterior strut (1), or with offset hooks applied above and below the screws (2). D:
Compression construct patterns. Flexion distraction injuries are
generally treatable with a simple posterior compression construct (1).
If a fracture dislocation has occurred, pedicle screw instrumentation
may be required to combat translational and rotational displacements (2). -
In upper thoracic fractures, place
supplemental hooks caudal to the injury to avoid a bulky construct
under the thinner soft tissues of the upper back. -
In lower thoracic injuries, place the supplemental hooks cranial to the fracture site.
-
Never place supplemental hooks at the
laminae just above the fractured vertebra, because this places the hook
directly opposite any bone fragment retropulsed into the spinal canal. -
In osteoporotic bone or in face of transverse process fractures, substitute laminolaminar claws for transversopedicular claws.
-
SSPI allows direct reduction of sagittal
deformity and translation while instrumenting the shortest possible
segment of the lumbar spine. -
Treat thoracolumbar and lumbar fractures with pedicle screws placed immediately above and below the fractured segment.
-
In cases of severe axial instability,
place offset laminar hooks at the level above the cranial hooks and at
the level of the caudal hooks.
pedicle screw hub, resulting in a high rate of bending failure. Acute
bending failure occurs before a solid arthrodesis has occurred and
before anterior column structures have regained enough strength to
share compressive loads. Failure during this period results in
progressive collapse of the spinal segment, progressive kyphosis, and
clinical symptoms. Ebelke et al. (34) found that transpedicular bone grafting eliminated pedicle screw failure in their series (see the section entitled Transpedicular Bone Graft), and similarly, patients with an intact or restored anterior column do not experience screw-bending failure (70).
with anterior column instability, SSPI is still an ideal approach for
selected patients (Fig. 142.15A, Fig. 142.15B). Do not attempt in situ
contouring of the rod unless offset laminar hooks are applied to
supplement screw fixation. These hooks provide improved clinical
results (4,39) and have
been shown to improve construct stiffness and to reduce screw bending
moments significantly both in sagittal loading and in situ contouring (22,83).
 |
|
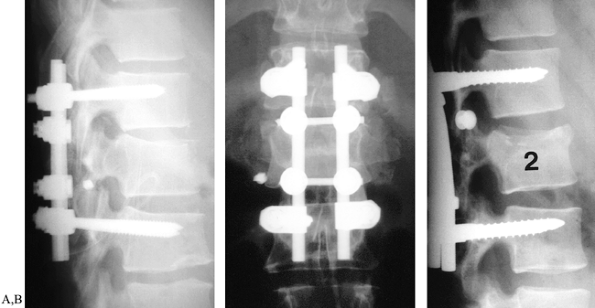
Figure 142.15. Short-segment pedicle instrumentation. A, B:
Lateral and AP views of 38-year-old patient with an L-1 burst fracture and marked sagittal collapse. Synthes Universal System fracture module was applied to correct kyphosis and anterior vertebral collapse. C: Similar fracture pattern treated with Cotrel-Dubousset segmental instrumentation. Because anterior column disruption was not severe, offset hooks were not applied. |
address thoracolumbar fractures with as little alteration of lumbar
spinal mechanics as possible (Fig. 142.16).
 |
|
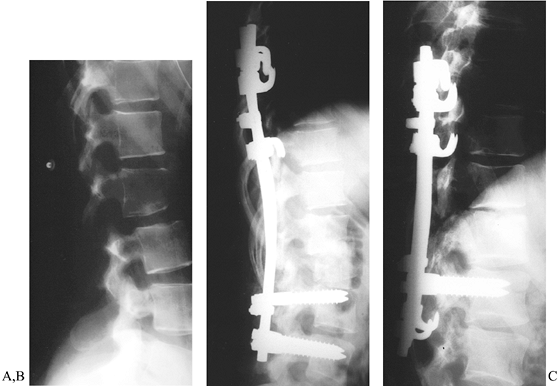
Figure 142.16. Extended pedicle screw constructs. A: Lateral view of 18-year-old patient with L1–L2 fracture-dislocation and incomplete cauda equina syndrome. B:
Extended construct using pedicle screws at L-2 and L-3 to stabilize the spinal column, with a down-going supplemental hook to compress the anterior strut graft. C: Extended pattern using supplemental offset hooks to protect pedicle screws. Intermediate hooks are directed cranially to decompress the fracture site indirectly. |
-
Extend the fixation construct into the
lower thoracic region to apply sufficient corrective force to reverse
sagittal deformity and restore neutral or lordotic alignment. -
Use pedicle screws just below the level of fracture to limit the extent of lumbar dissection and fusion (47,70). Pedicle screws may be supplemented with offset hooks.
short-segment construct, is the pedicle screw itself. Unless they are
supplemented with an offset laminar hook, additional levels of
fixation, or an anterior reconstruction, the pedicle screws are exposed
to large cantilever bending loads (73,78).
These forces are concentrated at the screw hub, a natural stress riser,
and the contact point between the screw and the lamina (22,45,68,70). Screw breakage that occurs after healing is complete is often asymptomatic (62).
Bending failure that occurs before the fracture has consolidated
results in progressive material failure and sagittal collapse, and can
occur even in braced patients (20,29,58). Patients treated with supplemental offset hooks or with an anterior reconstruction do not develop segmental collapse.
indication for anterior decompression. It should be recognized,
however, that canal compromise can be improved through indirect
reduction (77,86), and that bony remodeling improves canal diameter over time irrespective of treatment (71). Still, persistent neural compression can inhibit neurologic recovery (46), and anterior decompression can provide dramatic neurologic improvement in many patients (57,61).
Because functional outcome is more clearly related to the residual
neurologic deficit than to any other parameter, we continue to
emphasize the need to maximize early neurologic recovery. This entails
early recognition, rapid resuscitation, corticosteroid therapy, and
surgical
decompression when the patient is hemodynamically stable (12,15,23).
-
Carry out anterior decompression at the
thoracolumbar level through a combined thoracoabdominal approach,
providing access to the entire thoracolumbar segment. -
A T-11 retroperitoneal approach may
expose all of L-1 and most of T-12 but access to the fractured vertebra
and, particularly, to the canal will be hampered by the intact
diaphragm (see Chapter 138). -
After completing the surgical approach,
identify the fractured vertebral body by inspection and confirm the
level radiographically. -
After double-ligating the segmental
vessels at the level of the fracture and both vertebral bodies to be
instrumented, peel the psoas back from the vertebral body with a Cobb
elevator.After elevating the psoas muscle back to the level of
the neural foramen, completely debride the disc spaces above and below
the fracture of disc material, removing the outer annulus
circumferentially to the far side.
-
Debride the posterior annulus back to the
rim of the vertebral body and release it with a small curved curet. The
discectomies should be relatively bloodless. Release as much of the
fractured vertebra as is possible. -
Once the discs are gone, remove the fractured body piecemeal, taking the near and anterior cortices with double action rongeurs.
-
Remove bone back to the posterior cortex
with rongeurs and a high-speed burr, until the bell of the near pedicle
is exposed and the posterior vertebral cortex has been identified. -
Usually, there will be one large fragment
of bone locked between the pedicles, attached to the posterosuperior
annulus. Insinuate a fine, curved curet between the bell of the pedicle
and the back rim of this fragment to draw it out of the canal. -
Once this edge is freed from the overhanging pedicle, deliver the whole fragment anteriorly with the curet and pituitaries.
-
Significant bleeding may be encountered
as the posterior cortex is pulled away from the posterior longitudinal
ligament (PLL) and the nutrient vessels (Fig. 142.17). Use bipolar cautery and thrombin-soaked gel foam to control this hemorrhage.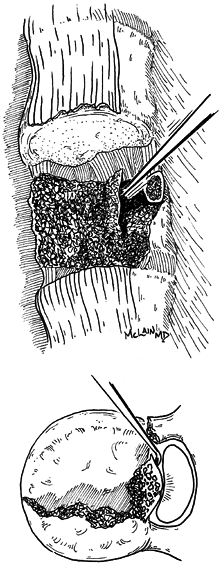 Figure 142.17. Reduction of retropulsed fragments.
Figure 142.17. Reduction of retropulsed fragments. -
On completion of the vertebrectomy, the dura should be visible from endplate to endplate and from pedicle to pedicle.
-
Then prepare the endplates for reconstruction.
after decompression, SSPI performs well in fractures of the lumbar
spine below L-2. Of the few burst fractures of the lower lumbar spine
that require surgical treatment, half will undergo anterior
decompression for cauda equina compression, followed by strut graft
reconstruction (70). Patients with no
neurologic injury typically require posterior SSPI alone. If there is
severe vertebral comminution, however, anterior reconstruction may be
needed to prevent progressive sagittal collapse (66).
multilevel injuries may benefit from internal fixation by one of two
techniques: compression hook constructs or pedicle screw fixation.
-
Reduce transverse disruptions by positioning the patient prone on transverse bolsters or the Jackson frame.
-
Use a limited exposure of the fracture
site, extending to the cranial rim of the first intact lamina above the
injury and to the caudal rim of the intact lamina below the injury. -
Debride the disruption of bone fragments,
hematoma, and disrupted ligamentum flavum, joint capsule, and muscle.
This will prevent the soft tissues from infolding into the canal when
the injury is reduced. -
After determining that the facet joints
are reduced and the laminar edges aligned, apply a compression
construct, with a hook above and one below the intact laminae. -
For more unstable injuries or frank
dislocations, pedicle screw instrumentation provides three-column
fixation to control axial, translational, and rotational displacements.
decompressive procedure or may be carried out primarily to address
axial instability. Anterior plate fixation may be adequate to
immobilize the spine in some cases in which the posterior elements have
not been injured. In cases in which laminar fractures or soft-tissue
disruption have rendered the posterior column incompetent, reinforce
anterior reconstruction with concomitant posterior instrumentation.
Likewise, anterior reconstruction at the lumbosacral junction will
require a posterior instrumentation, because no suitable fixation of
the sacrum yet exists.
the spinal canal is large compared with the volume of its contents, and
sagittal imbalance is more easily compensated for than at the
thoracolumbar junction.
occasionally associated with sacral fractures or sacral facet
fractures. Progressive deformity or onset of neurologic symptoms
requires surgical stabilization, typically with lumbosacral pedicle
screw instrumentation. Noninstrumented fusion is an option, but
progression of the slip may occur even when fusion is successful.
pelvic and sacral injuries. These injuries are the result of
high-energy trauma, and the patients are severely traumatized. Urgent
spinal stabilization is indicated to allow safe treatment of multiple
injuries, with early mobilization and aggressive pulmonary therapy. If
decompression is needed anteriorly, blood loss may be severe.
-
Repair dural tears primarily or with a fascial graft, and reconstruct the vertebrectomy with a tricortical strut or cage.
-
Standard anterior instrumentation is not
possible because screw fixation to the sacrum is both difficult and
tenuous. Immediate posterior instrumentation to prevent graft
displacement is indicated, when possible. -
Coordinate reconstruction of pelvic fractures or sacral disruptions with spinal care.
pelvic ring fractures, either in association with sacroiliac (SI) joint
injuries or as discreet sacral fractures. The treatment of sacral
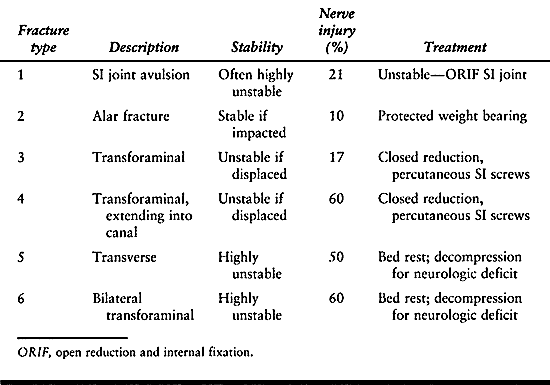
fractures in the context of pelvic trauma is discussed in Chapter 17. There are six basic fracture patterns, as shown in Table 142.2.
 |
|
Table 142.2. Sacral Fracture Patterns
|
root and cauda equina injury. Residual compression may result in
persistent neurologic deficit requiring surgical treatment. Patients
with persistent radiculopathy following fracture should undergo a
fine-cut CT scan of the sacrum. Neural foraminae with greater than 50%
canal compromise may be indicated for surgical decompression (24,28,35).
-
Position the patient prone with the abdomen free and a bolster under the pelvis.
-
Expose the sacral lamina through a midline incision and perform an L5–S1 laminotomy.
-
Then unroof the dural sac by laminectomy down to the S-3 level.
-
Identify the involved root (typically S-1) and follow it laterally into the foramen.
-
Take the interval between S-1 and S-2 down to the dorsal aspect of the ventral cortex.
-
Carry out debridement to the anterior
aperture of the neuroforamen, or until the compression is relieved and
the nerve root is free and mobile. -
Fixation of the fracture is usually not
possible. Limit the patient’s weight bearing until the fracture has
united; patient should avoid sitting for up to 2 months.
laminectomy alone may not be enough to decompress the nerve roots,
which are often tented over the kyphotic deformity. This bony
prominence must be removed.
-
To avoid injuring these roots, carry out
a lateral approach to the anterior from between the exposed nerve roots
at the level of fracture, usually between S-1 and S-2. -
Use narrow osteotomes and down-biting curets to fragment the retropulsed bone, and decompress the cauda equina.
-
Once the kyphotic ridge has been removed, the nerve roots should be freely mobile.
followed, serious complications can occur following spinal
stabilization. Reduction of fractures and fracture dislocations through
distraction is a routine manuever, but overdistraction can widely
displace bony elements and stretch the spinal cord, causing serious
neurological injury. Also, posterior reconstruction of severe burst
fractures without restoring the anterior weight-bearing column exposes
instrumentation systems to excessive cantilever-bending forces,
resulting in acute pedicle screw-bending failure, or late collapse and
fatigue failure. If the normal thoracolumbar lordosis is not restored
at the time of surgery, the forces of weight bearing will fall anterior
to the lumbar spine and pelvis, imparting an exaggerated flexion moment
on the fracture and fixation construct, again predisposing to
instrumentation failure. Finally, failure to expose the thecal sack
completely—from pedicle to pedicle and endplate to endplate—during an
anterior decompression may result in persistent neurologic impairment.
ability to address the individual “personality” of each spine fracture
has improved. Segmental constructs and pedicle fixation have improved
fixation strength and construct stiffness, allowing us to get patients
out of bed, into rehabilitation, and home more rapidly and with better
long-term results. Newer implant systems must still be applied
with
full attention to fracture type and biomechanical principles, or
implant failure is sure to occur. Technique and implant design cannot
alter the damage done to the spinal cord at injury either, and
functional outcomes are most profoundly dependent on neurologic
integrity. Further research in spinal cord recovery and regeneration
holds the greatest promise for future victims of major spinal trauma.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
M, Etter C, Kehl T, Thalgott J. The Internal Skeletal Fixation System:
A New Treatment of Thoracolumbar Fractures and Other Spinal Disorders. Clin Orthop 1988;227:30.
BA, Crandall DG, Burkus K, Matthews T. Use of Long Rods and a Short
Arthrodesis for Burst Fractures of the Thoracolumbar Spine. A long-term
follow-up study. J Bone Joint Surg [Am] 1994;76:1629.
BA, Fogarty JP, Tayob AA. Contoured Harrington Instrumentation in the
Treatment of Unstable Spinal Fractures. The Effect of Supplementary
Sublaminar Wires. Clin Orthop 1984;189:186.
C, Lovet J, de Peretti F, et al. The Treatment of Spinal Fractures with
Cotrel-Dubousset Instrumentation. Results of the First 85 Cases.
Scoliosis Research Society/European Spine Meeting. Orthop Trans 1990;14:776.
IT, Tandogan NR, Kis M, et al. Cotrel-Dubousset Instrumentation in the
Treatment of Unstable Thoracic and Lumbar Spine Fractures. Arch Orthop Trauma Surg 1994;113:86.
DR, Burkus JK, Montesano PX, et al. Unstable Thoracolumbar and Lumbar
Burst Fractures Treated with the AO Fixateur Interne. J Spinal Disord 1992;5:335.
EC. Short-segment Compression Instrumentation for Selected Thoracic and
Lumbar Spine Fractures: The Short-rod/Two-claw Technique. J Neurosurg 1993;79:335.
TN, Whitecloud TS III, Rodriguez RP, Hadad RJ Jr. Segmental Spinal
Instrumentation in the Management of Fractures of the Thoracic and
Lumbar Spine. South Med J 1983;76:1232.
OM, Myllynen PJ, Riska EB. Unstable Fractures of the Thoracic and
Lumbar Spine: The Audit of an 8-year Series with Early Reduction using
Harrington Instrumentation. Injury 1987;18:190.
MB, Shepard MJ, Collins WF, et al. A Randomized, Controlled Trial of
Methylprednisolone or Naloxone in the Treatment of Acute Spinal Cord
Injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med 1990;322:1405.
CE, Sullivan JA. Management of Thoracic and Lumbar Spine Fractures with
Harrington Distraction Rods Supplemented with Segmental Wiring. Spine 1983;8:532.
M, McLain RF, Yerby SA, et al. Short-segment Pedicle Instrumentation.
Biomechanical Analysis of Supplemental Hook Fixation. Spine 1996;21:288.
JC, Akbarnia BA, Bucholz RD, et al. Neurologic Recovery Associated with
Anterior Decompression of Spine Fractures at the Thoracolumbar Junction
(T12–L1). Spine 1992;17(Suppl):S325.
F, Armstrong GWD, Searls K, Matta L. Acute Thoracolumbar Burst
Fractures in the Absense of Neurological Deficit: A Comparison Between
Operative and Non-operative Treatment. Clin Orthop 1984;189:142.
Instrumentation in Traumatic Spine Injuries. The 6th Proceeding of the
International Congress on Cotrel-Dubousset Instrumentation. Montpellier, France: Sauramps Medical, 1989:41.
CA, Yahiro MA, Lu HT, Melkerson MN. Surgical Treatment Alternatives for
Fixation of Unstable Fractures of the Thoracic and Lumbar Spine. A
Meta-analysis. Spine 1994;19(Suppl):2266.
JH, Harrington PR, Erwin WD. Results of Reduction and Stabilization of
the Severely Fractured Thoracic and Lumbar Spine. J Bone Joint Surg [Am] 1978;60:799.
DK, Asher MA, Neff JR, Kraker DP. Survivorship Analysis of VSP Spine
Instrumentation in the Treatment of Thoracolumbar and Lumbar Burst
Fractures. Spine 1991;16(Suppl):428.
J-P, Weidenbaum M, Michelsen CB, et al. A Comparative Biomechanical
Study of Spinal Fixation Using Cotrel-Dubousset Instrumentation. Spine 1987;12:877.
JR, Leider LL, Erickson DL, et al. Harrington Instrumentation and Spine
Fusion for Unstable Fractures and Fracture-dislocations of the Thoracic
and Lumbar Spine. J Bone Joint Surg [Am] 1977;59:143.
DJ, Taddonio RF, Byrne DW, et al. Incidence of Acute Care Complications
in Vertebral Column Fracture Patients with and without Spinal Cord
Injury. Spine 1995;20:1136.
SD, Court-Brown CM. Rationale for the Management of Flexion-distraction
Injuries of the Thoracolumbar Spine Based on a New Classification. J Spinal Disord 1989;2:176.
Segment Internal Fixation Using CD Instrumentation with Pedicular
Screws: Biomechanical Testing. The 6th Proceeding of the International
Congress on Cotrel-Dubousset Instrumentation. Montpellier, France: Sauramps Medical, 1989:19.
C, Firooznia H, Rafii M, et al. Computed Tomography of Thoracic and
Lumbar Spine Fractures that Have Been Treated with Harrington
Instrumentation. Radiology 1984;151:731.
KR, McAfee PC, Shih C. Biomechanical Analysis of Posterior
Instrumentation Systems after Decompressive Laminectomy. An Unstable
Calf-spine Model. J Bone Joint Surg 1988;70A:680.
KR, McAfee PC, Shih C. Biomechanical Analysis of Anterior and Posterior
Instrumentation Systems after Corpectomy. A Calf-spine Model. J Bone Joint Surg 1988;70A:1182.
RR, Asher MA, Snider RK. Thoracolumbar Spinal Injuries: A Comparative
Study of Recumbent and Operative Treatment in 100 Patients. Spine 1980;5:463.
RR, Nordwall A, Nachemson, A. Reduction, Stability, and Strength
Provided by Internal Fixation Systems for Thoracolumbar Spinal
Injuries. Clin Orthop 1982;171:300.
CE, Ashman RB, Sherman MC, et al. Mechanical Consequences of Rod
Contouring and Residual Scoliosis in Sublaminar Segmental
Instrumentation. J Orthop Res 1987;5:206.
DL, Rodgers WB, Mansfield FL. Transpedicular Instrumentation and
Short-segment Fusion of Thoracolumbar Fractures: A Prospective Study
Using a Single Instrumentation System. J Orthop Trauma 1995;9:499.
DC, Graziano GP. A Comparison Study of Treatment of Thoracolumbar
Fractures Using the ACE Posterior Segmental Fixator and
Cotrel-Dubousset Instrumentation. Orthopaedics 1995;18:679.
PC, Bohlman HH, Yuan HA. Anterior Decompression of Traumatic
Thoracolumbar Tractures with Incomplete Neurological Deficits Using a
Retroperitoneal Approach. J Bone Joint Surg 1985;67A:89.
PC, Werner FW, Glisson RR. A Biomechanical Analysis of Spinal
Instrumentation Systems in Thoracolumbar Fractures. Comparison of
Traditional Harrington Distraction Instrumentation with Segmental
Spinal Instrumentation. Spine 1985;10:204.
TO, McLain RF, Yerby SA, et al. The Effect of Pedicle Morphometry on
Pedicle Screw Loading in Unstable Burst Fractures: A Synthetic Model. Spine 1997;22:246.
of Correction: Late Kyphosis in Short Segment Pedicle Fixation in Cases
of Posterior Transpeduncular Decompression. The 6th Proceeding of the
International Congress on Cotrel-Dubousset Instrumentation. Montpellier, France: Sauramps Medical, 1989:37.
J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar Burst Fractures. The
Clinical Efficacy and Outcome of Nonoperative Management. Spine 1993;18:955.
MM, Oxland TR, Kifune M, et al. Validity of the Three-column Theory of
Thoracolumbar Fractures. A Biomechanic Investigation. Spine 1995;20:1122.
HM, Donaldson DH, Brown CW, Stringer EA. Stabilization of Thoracic
Spine Fractures Resulting in Complete Paraplegia. A Long-term
Retrospective Analysis. Spine 1994;19:1726.
RC, Cotler HB. Posterior Instrumentation and Fusion for Unstable
Fractures and Fracture-dislocations of the Thoracic and Lumbar Spine. A
Comparative Study of Three Fixation Devices in 70 Patients. Spine 1993;18:450.
WP, Rogers JV, Sickler ME, et al. Thoracolumbar Burst Fractures: CT
Dimensions of the Spinal Canal Relative to Postsurgical Improvement. AJR Am J Roentgenol 1985;145:337.
PJ Jr, Patwardhan AG, Lorenz M, et al. Instability of the Lumbar Burst
Fracture and Limitations of Transpedicular Instrumentation. Spine 1995;20:1452.
J, Lindahl S, Nordwall A. Unstable Thoracolumbar Fractures. A
Comparative Clinical Study of Conservative Treatment and Harrington
Instrumentation. Spine 1985;10:111.