Fractures of the Pelvis
Approximately two thirds of pelvic fractures are complicated by other
fractures and injuries to soft tissues. The fatality rate from pelvic
hemorrhage with current management techniques ranges from 5% to 20% (4,5).
Pelvic fractures generally are the result of direct trauma or of
transmission of forces through the lower extremity. The importance of
these fractures lies more in the associated soft-tissue injury and
hemorrhage than in the fracture per se (1,5,6).
-
Types
-
Type A: stable
-
Type B: rotationally unstable, but vertically and posteriorly stable
-
Type C: rotationally and vertically unstable
-
-
Subtypes, which have important influences on treatment, are presented in Table 21-1 and illustrated in Figs. 21-1, 21-2, and 21-3.
-
Fractures of the acetabulum are discussed in Chap. 22.
-
Note for historical purposes that a Malgaigne fracture is a vertical fracture or dislocation of the posterior sacroiliac joint complex involving one side of the pelvis.
-
Pelvic fractures are suspected because of pain, crepitus, or tenderness over the symphysis pubis, anterior iliac spines, iliac crest, or sacrum,
but a good roentgenographic examination is essential for diagnosis.
Patients with these injuries are often unconscious or intubated, so the
examination for stability is helpful. The iliac wings are grasped and
force-directed to the midline; instability can be detected with this
maneuver. Gentle handling of the patient minimizes further bleeding and
shock. -
Specific studies.
Patients with all but minimal trauma should have an indwelling urinary
catheter for the dual purposes of measuring urine output while the
associated shock is being treated and investigating possible bladder
trauma. If there is blood at the penile meatus, then a retrograde
urethrogram should be performed before passage of the catheter (1,2,6).
This prevents completion of a partial urethral tear. Intravenous
pyelography (IVP) and cystography document renal function, bladder
anatomy, and help delineate the size of any pelvic or retroperitoneal
hematoma. When the initial urinalysis reveals less than 20 red blood
cells per high powered field rbc/hpf, an IVP is generally not necessary
(8). Despite the difficulties involved, a
pelvic (in women) and rectal examination should be done to check for
fresh blood and open wounds, perineal sensation in a conscious patient,
a displaced unstable prostate, and sphincter tone. These fractures
frequently are associated with neurologic damage, so a careful
neurologic evaluation should be done in all patients.
-
Symptoms and signs.
At presentation, approximately 20% of patients are in shock. Severe
backache can help differentiate the pain of retroperitoneal bleeding
from the pain of intraabdominal bleeding. -
Treatment.
Pneumatic antishock garments (MAST trousers) help reduce the pelvic
volume by compression of the iliac wings. MAST trousers are not useful
as
P.300
a routine transfer aid for patients with blunt trauma (9).
These garments are useful in transport of patients where there is a
high degree of suspicion of a pelvic fracture, but should be removed as
soon as resuscitation is underway because they are associated with
compartment syndrome in the legs (10). Most
causes of hemorrhage are adequately handled by rapid replacement and
maintenance of blood volume, followed by reduction (when appropriate)
and stabilization of the fractures as described in VI.
Adequate blood replacement is the first priority, and its effectiveness
is monitored by the patient’s pulse, blood pressure, central venous
pressure, urine output, and so on, as described in Chap. 1.
Blood loss of 2500 mL is common, and blood replacement is usually
necessary even without evidence of an open hemorrhage. Diagnostic
peritoneal lavage is a useful test to rule out intraabdominal injury at
the site of hemorrhage (6). Abdominal computed tomography (CT) scan and abdominal ultrasound are effective (first) screening tests for this condition (2,5).
The surgeon must follow the patient’s platelet count and coagulation
studies after 4 units of blood have been given because disseminated
intravascular coagulation can result from dilution of these components.
The use of angiography and embolization of distal arterial bleeding
points with blood clot, Gelfoam, or coils has been proven to be useful (1,2).
Because only 10% of patients have identifiable arterial bleeding, the
authors prefer to stabilize the pelvis first with internal or external
fixation (1,2,5,11,1213). Anterior external fixation with one or two pins in each iliac wing is an effective means of stabilizing the pelvis
P.301P.302
when the traumatic pattern allows its use (11,14,15).
Alternatively, wrapping the patient in a hospital sheet at the level of
the iliac rings or in a commercially available pelvic binder have been
proven to be effective simple methods of decreasing the pelvic volume (4).
If the pelvic injury involves the posterior wing with a sacral fracture
or unstable sacroiliac joint injury, the antishock clamp can be
lifesaving. It requires skill, familiarity with the device, and
fluoroscopic control (16). Spica casting can also be used if the necessary expertise or equipment is not available (17).
Distal femoral pins must be incorporated into the cast. If this does
not control the bleeding, then arteriography and embolization are
indicated (2).TABLE 21-1 Substances of Pelvic FracturesType A: Stable
A1 Fractures not involving ring; avulsion injuries
A1.1 Anterior superior spine
A1.2 Anterior inferior spine
A1.3 Ischial tuberosity
A2 Stable, minimal displacement
A2.1 Iliac wing fractures
A2.2 Isolated anterior ring injuries (four-pillar)
A2.3 Stable, undisplaced, or minimally displaced fractures of the pelvic ring
A3 Transverse fractures of sacrum and coccyx
A3.1 Undisplaced transverse sacral fractures
A3.2 Displaced transverse sacral fractures
A3.3 Coccygeal fractureType B: Rotationally unstable; vertically and posteriorly stable
B1 External rotation instability; open-book injury
B1.1 Unilateral injury
B1.2 Less than 2.5-cm displacement
B2 Internal rotation instability; lateral compression injury
B2.1 Ipsilateral anterior and posterior injury
B2.2 Contralateral anterior and posterior injury; bucket-handle fracture
B3 Bilateral rotationally unstable injuryType C: Rotationally, posteriorly, and vertically unstable
C1 Unilateral injury
C1.1 Fracture through ilium
C1.2 Sacroiliac dislocation or fracture-dislocation
C1.3 Sacral fracture
C2 Bilateral injury, with one side rotationally unstable and one side vertically unstable
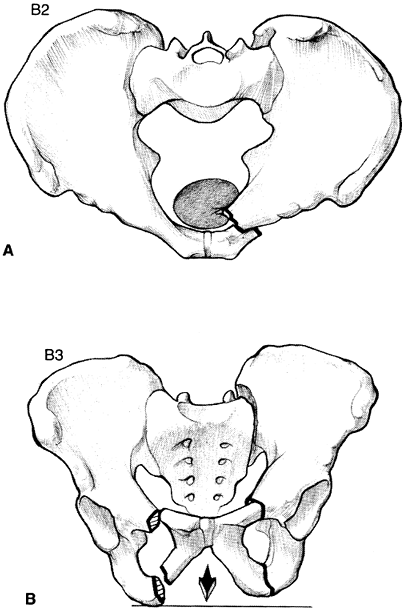
C3 Bilateral injury, with both sides completely unstableFrom Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg 1988;70B:I. 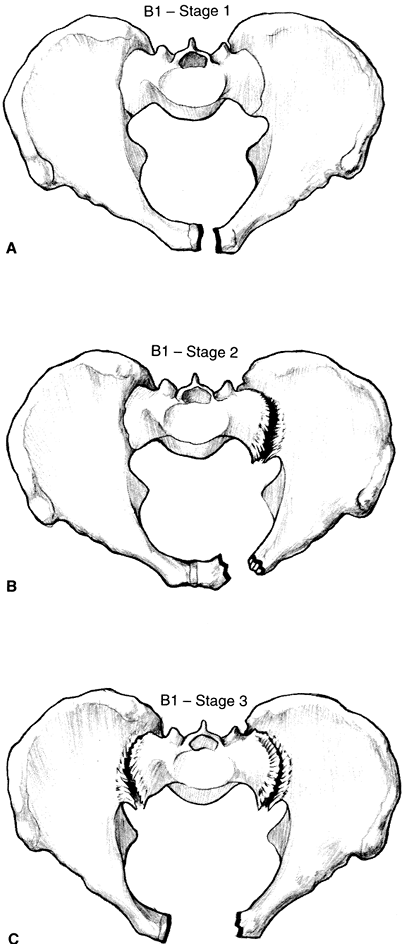 Figure 21-1. A: Type B1, stage 1 symphysis pubis disruption. B: Type B1, stage 2 symphysis pubis disruption. C: Type B1, stage 3 symphysis pubis disruption. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:228.)
Figure 21-1. A: Type B1, stage 1 symphysis pubis disruption. B: Type B1, stage 2 symphysis pubis disruption. C: Type B1, stage 3 symphysis pubis disruption. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:228.)![]() Figure 21-2. A: Type B2 lateral compression injury (ipsilateral). B: Type B3 lateral compression injury (contralateral). (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:228.)
Figure 21-2. A: Type B2 lateral compression injury (ipsilateral). B: Type B3 lateral compression injury (contralateral). (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:228.)
-
An anteroposterior view of the pelvis
is made routinely in all patients who have suffered severe trauma or
who complain of pain in and around the pelvic region. After the
patient’s general condition has stabilized following a pelvic fracture,
special films are indicated, including a 60-degree caudad-directed
inlet view and a 40-degree cephalad-oriented tangential (or outlet)
view (7,12). The former helps visualize the posterior pelvic ring, and the latter is for the anterior ring. -
CT scans can be most useful in defining posterior ring fractures (1,2,13). Fifty percent of sacral fractures are missed on plain roentgenograms, but they are well visualized on CT scans.
-
Stable A type fractures
are treated symptomatically. Turn the patient by logrolling or begin
treatment on a Foster frame until the severe pain subsides. As soon as
the patient can move comfortably in bed, he or she can ambulate in a
walker and progress to walking with crutches. The fractures are through
cancellous bone that has good blood supply, and stability of the
P.303P.304
fracture
usually is present in 3 to 6 weeks, with excellent healing expected
within 2 months. Because of the dense plexus of nerves about the sacrum
and coccyx, injuries to this area may produce chronic pain, especially
if the patient is not encouraged to accept some discomfort and start an
early active exercise program.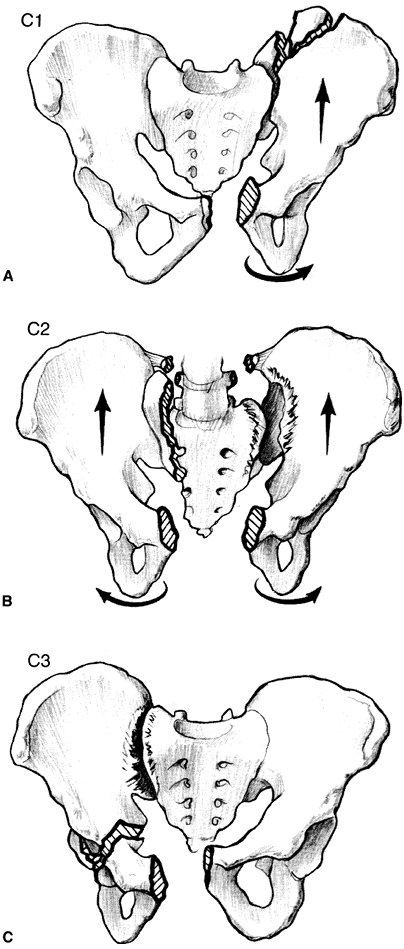 Figure 21-3. A: Type C1 pelvic injury. B: Type C2 pelvic injury. C: Type C3 pelvic injury. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:229.)
Figure 21-3. A: Type C1 pelvic injury. B: Type C2 pelvic injury. C: Type C3 pelvic injury. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:229.) -
Type B fractures
(rotationally unstable, but vertically and posteriorly stable) must be
treated on an individual basis. Fracture displacements, associated
injuries, age of the patient, and functional demands should be taken
into account (1,5,13).
In open-book fractures, disruption of the anterior sacroiliac joints
and sacrospinous ligaments occurs if the displacement is more than 2.5
cm. These may be reduced and stabilized by external fixation or plate
fixation across the symphysis (11,12).
The authors generally prefer plate fixation because of the problems
with patient comfort, pin tract infection, and loosening and loss of
reduction with external fixation (5,14,18).
Minimally displaced B1, B2, and B3 injuries may be treated
conservatively with bed to wheelchair mobilization for 6 to 8 weeks,
followed by crutch ambulation with weight bearing to tolerance on the
side of the pelvis where the posterior ring is uninjured or more
stable. Internal fixation is used for more widely displaced and
unstable injuries (2,12,13). Traction is not recommended because of patient morbidity and the inability to improve fracture displacements. -
Type C minimally displaced isolated injuries, especially those involving the ilium, may be treated conservatively as in B.
However, patients need to be followed up closely roentgenographically
and, if fracture displacement is increasing, reduction and fixation is
indicated. Some centers utilize simulated weight-bearing radiographs as
a method for detecting fracture instability. Improved results with
internal fixation over traction treatment have been documented (12).
If seen early on, then fractures of the sacrum and sacroiliac joints
can be managed with closed reduction and percutaneous lag screw
fixation (2,13).
Because of the complexity of reduction and fixation techniques as well
as the potential for high morbidity resulting from adjacent
neurovascular structures, patients with type C injuries should be
referred to an experienced pelvic and acetabular surgeon.
-
Complications from associated injuries (e.g., of the bladder, cranium, chest)
-
Persistent symptoms from sacroiliac joint instability, including pain and leg length inequality
-
Chronic pain patterns from injuries around the coccyx and sacrum and sacroiliac joint (19,15), including dyspareunia
-
Persistent neurologic deficit from nerve root injury with L5, S1, and distal sacral root injuries most common; erectile dysfunction is common in males
-
Pulmonary and fat emboli
-
Infection from bacterial seeding of the large hematomas or from open pelvic fractures (20). Injuries to the large bowel are not uncommon.
hemorrhage, limited weight bearing (6–8 weeks) for lateral compression
fractures that do not have significant deformity, non–weight bearing
for other nondisplaced patterns for 8 to 12 weeks, follow-up
radiographs to check for late instability
Ongoing hemorrhage (external fixation or posterior pelvic clamp),
displaced posterior pelvic injury, symphysis widening more than 2.5 cm,
unacceptable pelvic deformity
Symphysis plating, posterior iliosacral screws. Open reduction and
iliosacral screw placement is safest; consider percutaneous iliosacral
screws in thin patient with minimal deformity. Occasionally, anterior
sacroiliac joint fixation is performed if posterior skin is not safe or
if the injury is associated with an ipsilateral acetabular fracture.
GS, Leit ME, Gruen RJ, et al. The acute management of neurodynamically
unstable multiple trauma patients with pelvic ring fractures. J Trauma 1994;36:706–713.
TA, Fleisher GR, Mahboubi S, et al. Hematuria and clinical findings as
indications for intravenous pyelography in pediatric blunt renal
trauma. Pediatrics 1988;82:216–222.
ML Jr, Kreger PI, Simonian PT, et al. Early results of percutaneous
iliosacral screws placed with the patient in the supine position. J Orthop Trauma 1995;9:207–214.
JV, Trenhaile SW, Miranda M, et al. Vertical shear injuries: is there a
relationship between residual displacement and functional outcome? J Trauma 1999;46:1024–1030.
J, Hirvensalo E, Bostman O, et al. Failure of reduction with an
external fixator in the management of injuries of the pelvic ring
long-term evaluation of 110 patients. J Bone Joint Surg (Br) 1999;81:955–962.
CE, Bosse MJ, McCarthy ML, et al. Effect of trauma and pelvis fracture
on female genitourinary, sexual and reproductive function. J Orthop Trauma 1997;11:73–81.
DJ, Olson SA, Matta JM. Diagnosis and management of closed internal
degloving injuries associated with pelvic and acetabular fractures: the
morel-lavallee lesion. J Trauma 1997;42:1048–1051.