Gastrocnemius and Soleus Rotational Muscle Flaps: Soft-Tissue Coverage
IV – Miscellaneous Topics > 46 – Gastrocnemius and Soleus Rotational
Muscle Flaps: Soft-Tissue Coverage
bones, joints, tendons, or hardware are exposed and require coverage.
In the lower leg and particularly the tibia, a muscle flap must be well
vascularized and durable. Of all the local rotational flaps, the
gastrocnemius is one of the most reliable. The gastrocnemius is a broad
muscle with a single proximal vascular pedicle, which is well protected
in the popliteal fossa. The gastrocnemius muscle or myocutaneous
rotational flap is used for the procedure of choice for soft-tissue
coverage of complex open wounds about the knee and proximal third of
the tibia and fibula. The use of this flap is indicated in the
following circumstances: (a) coverage of acute, grade IIIB, open,
tibial fractures with or without hardware involving exposure of the
knee joint, capsule, fracture site, or exposed cortex (Fig. 46.1);
(b) obliteration of dead space and wound closure after radical
debridement of osteomyelitic wounds in this region as well as infected
nonunions (Fig. 46.2); (c) coverage of exposed total-knee arthroplasties or pre-arthroplasty tissue augmentation in densely scarred wound beds (Fig. 46.3); and (d) limb salvage and coverage of endoprostheses or allograft material after resection of musculoskeletal neoplasms (Fig. 46.4).
a much more limited area of rotation and is used primarily for small,
medially based, open wounds in the middle third of the leg. Indications
include coverage of acute open fractures and chronic osteomyelitic
wounds (Fig. 46.5).
include vascular compromise of the muscle itself by disruption of the
sural artery pedicle, compromise of the popliteal artery from which it
emanates, or occlusion of the proximal arterial tree. Significant local
trauma to the muscle itself, although rare, prevents its successful
rotation.
 |
|
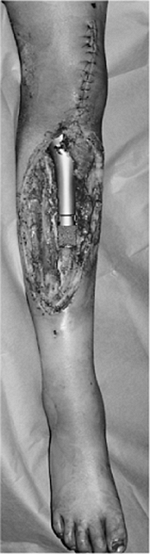
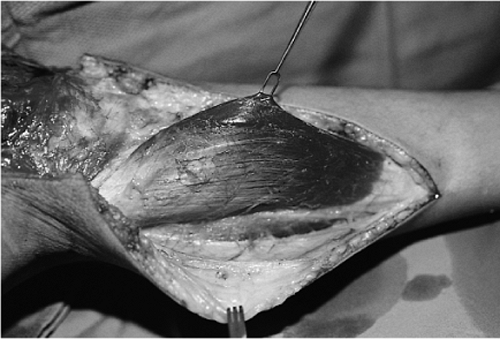
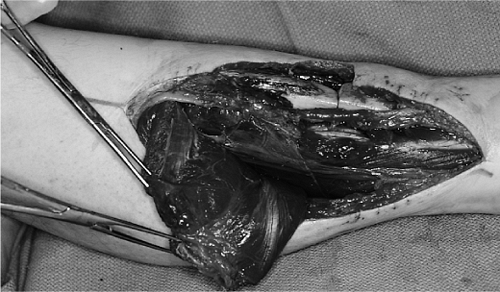
Figure 46.1.
Grade IIIB open tibial-plateau fracture with exposed knee joint after internal fixation and unsuccessful attempt at primary wound closure. |
 |
|
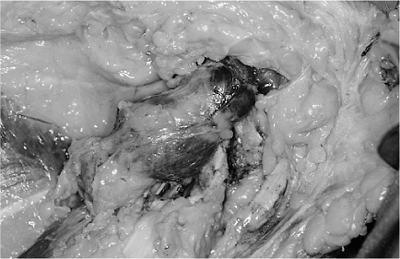
Figure 46.2. Dead space involving skin, subcutaneous tissue, muscle, and bone in a proximal-third infected nonunion.
|
 |
|
Figure 46.3. Scarred, atrophic, prepatella skin in an elderly patient after removal of an infected total-knee arthroplasty.
|
 |
|
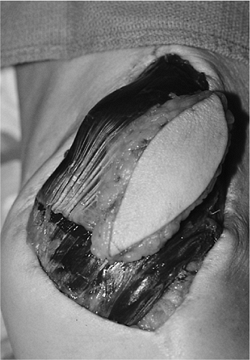
Figure 46.4.
A 10-year-old girl immediately after tumor extirpation of a proximal tibial osteosarcoma and placement of endoprosthesis after loss of anterior skin. |
 |
|
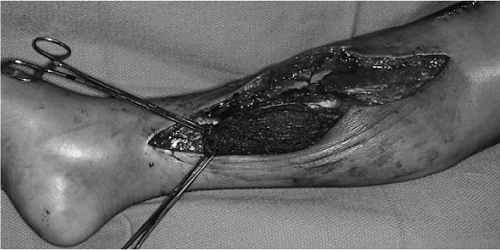
Figure 46.5. Middle-third grade IIIB open-tibial fracture with a bony sequestrum and loss of overlying soft tissue.
|
proximal third region in which its size and dimension are too large for
coverage by the gastrocnemius muscle. Similarly, injury to the
substance of the soleus muscle will hinder its ability to be
transposed. Vascular compromise to the soleus muscle is extremely rare
because of its segmental inflow. Because of minor perforators that exit
from the posterior tibial artery distally, the surgeon must take great
care to assure adequate vascularity to the most distal aspect of the
soleus muscle when a large transposition is undertaken. As with the
gastrocnemius, a large anterior or laterally located wound in the
middle third of the leg may not be completely covered by the soleus
muscle (Fig. 46.6), and free tissue transfer may be a better option.
 |
|
Figure 46.6.
Large, grade IIIB, open, middle-third tibial fracture cannot be closed by a local soleus flap and requires free tissue transfer. |
tumor recurrence is best avoided by thorough debridement or excision
before wound closure. No muscle flap will successfully combat retained
sequestrum or loose infected hardware, which act as nidi for continued
infection.
planning either a gastrocnemius or soleus muscle flap for coverage of a
complex open wound. Radiographs should be viewed with particular
attention paid to fracture location and the presence or absence of
internal fixation devices. For acute fractures, if an external fixator
is indicated, the surgeon should anticipate the need for subsequent
soft-tissue closure and construct the frame to allow unrestricted
transposition of the muscles from the posterior to a medial or anterior
plane. The zone of injury around the fracture site should be recognized
because aggressive or radical debridement may significantly alter the
dimensions of the wound (Fig. 46.7). Clinical
examination of the leg should be made, with particular attention paid
to would length, width, and depth. Other factors such as induration,
discoloration, ecchymosis, and cellulitis must be considered.
dorsalis pedis and posterior tibial pulses for arterial inflow, as well
as Doppler examination for venous outflow, should be documented.
Arteriography may be indicated if pulses are absent or diminished (Fig. 46.8).
The function of the posterior compartment muscles should be assessed
whenever possible. Sensory examination of the foot must be documented,
with particular attention given to the posterior tibial, sural, and
saphenous nerves. The surgical incisions can be planned in conjunction
with the need for additional debridement and internal or external
fixation of the fracture.
 |
|
Figure 46.7. Large amount of retained titanium from a previously removed, infected, total-knee arthroplasty.
|
 |
|
Figure 46.8.
Angiogram demonstrating patency of the popliteal artery and continuity of the sural arteries despite the fracture comminution and retained gunshot pellets. |
 |
|
Figure 46.9. Completed debridement of infected fracture of the knee with removal of all nonviable soft tissue and bony sequestrum.
|
 |
|
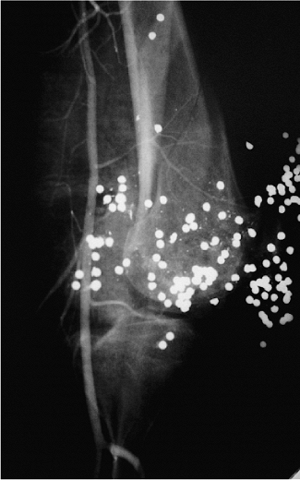
Figure 46.10. The gastrocnemius muscle is visible when the deep investing fascia is incised longitudinally.
|
complete and definitive debridement of a traumatic or infected wound
has been completed or a tumor has been extirpated (Fig. 46.9).
A tourniquet is placed on the thigh, and the entire leg is prepped and
draped. The approach to the gastrocnemius muscle can be made through
perpendicular, oblique, or parallel incisions.
must be tunneled beneath the resulting bipedicled fasciocutaneous flap.
The gastrocnemius muscle is identified by incising the deep investing
fascia of the leg longitudinally along the anterior border of the
muscle (Fig. 46.10).
the muscle and distally to its insertion on the Achilles tendon if
necessary. The fatty plane between the gastrocnemius and soleus is
developed by either sharp or digital dissection. This areolar plane is
confirmed by visualization of the plantaris longus tendon, which lies
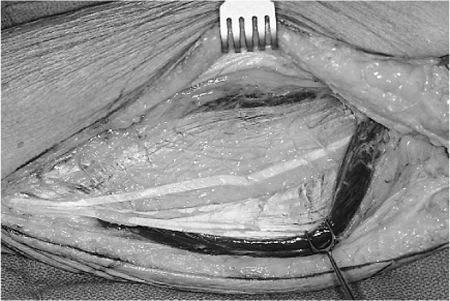
adjacent to the soleus at or near its medial border (Fig. 46.11). The white investing fascia on the posterior border of the
soleus and the deep border of the gastrocnemius make recognition of
this plane unmistakable. Occasionally perforators between the soleus
and gastrocnemius exist and must be divided. As the surgeon works
posteriorly (superficial), the muscle is easily separated from the deep
investing fascia. One or two myocutaneous perforators must be saved if
a myocutaneous flap is planned; otherwise, they are divided. The
gastrocnemius is separated along its median raphe into a medial and a
lateral head. The raphe is easier to identify and more prominent in the
distal portion of the muscle (Fig. 46.12).
The sural nerve and lesser saphenous vein run along the raphe and
should be preserved. These are constant landmarks and facilitate
separation of the medial from the lateral head. When the median raphe
has been identified, dissection proceeds from distal to proximal, with
the surgeon working along the posterior midline while protecting the
neurovascular structures at all times. When both the posterior and
anterior surfaces are freed, the gastrocnemius can be released from its
attachment to the Achilles tendon. The dissection continues proximally
to the origin of the gastrocnemius muscle from the femoral condyle (Fig. 46.13).
 |
|
Figure 46.11. The plantaris longus tendon confirms the plane between the gastrocnemius and soleus muscles.
|
 |
|
Figure 46.12.
The median raphe separates the medial and lateral heads of the gastrocnemius and carries the neurovascular structures, which must be protected. |
resecting its tendinous attachments, resulting in a 2- to 3-cm increase
in the length for arc of rotation. The muscle can also be expanded
significantly in both the transverse and longitudinal planes by
crisscross incisions made both anteriorly and posteriorly through its
heavily fused bilaminar myofascia (Fig. 46.15).
Furthermore, the gastrocnemius muscle can be split longitudinally in
the distal portion so that part of the muscle can be used to obliterate
deep dead space, while the remainder of the muscle can be used for
superficial coverage.
 |
|
Figure 46.13. Exposure of the muscle origin on the femoral condyle requires adequate muscle retraction and sufficient proximal exposure.
|
 |
|
Figure 46.14. When needed, the sural artery pedicle can be visualized on the deep surface of the gastrocnemius in the popliteal fossa.
|
 |
|
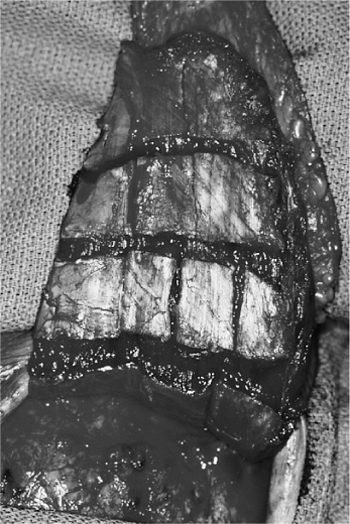
Figure 46.15.
Transverse and longitudinal myofascial release on both deep and superficial surfaces allows significant expansion of muscle area to be used for coverage. |
 |
|
Figure 46.16. Ideal wounds for soleus coverage are small medial wounds located in the middle third of the leg.
|
fashion from a lateral cutaneous approach by using one of the three
incisions described. Of paramount importance is the identification and
protection of the peroneal nerve just below the head of the fibula as
it penetrates from superficial to deep into the lateral compartment.
After the safety of this nerve is assured, raising the lateral
gastrocnemius muscle is done in a fashion similar to that described for
the medial head. It should be noted, however, that the lateral
gastrocnemius muscle is smaller than the medial head and will not
provide the same quantity of muscle for laterally based lesions.
approach and is used to cover small medial and anterior-based
middle-third wounds (Fig. 46.16). A curvilinear
incision is made over the medial aspect of the calf. The plane between
the gastrocnemius and soleus muscles is easily identified and serves as
an excellent starting point. When raising the soleus, the
gastrocnemius–Achilles musculotendinous unit must be preserved at all
times. Alice clamps are placed on the edge of the Achilles tendon to
better demonstrate the area where the two merge. The fascia that fuses
the posterior soleus to the Achilles is divided (Fig. 46.17). Proceeding from proximal to distal, the surgeon dissects the muscle off the Achilles
tendon with either a knife or Metzenbaum scissors from medial to
lateral. A pseudoraphe is encountered approximately three fourths of
the way through the dissection. It is important to separate this and
continue the dissection both posteriorly and then laterally to include
the entire soleus muscle. The muscle is released distally to include as
much length as possible (Fig. 46.18).
The plane between the deep side of the soleus and the deep flexor
compartment is identified and can be digitally dissected. Care must be
taken to identify the distal perforators arising from the posterior
tibial artery and vein. These can be very short, and if inadvertently
injured or cut, they may retract beneath the deep fascia, making them
difficult to ligate. When these distal perforators have been
identified, ligated, and divided, the soleus attachments on the lateral
side are dissected free under direct visualization. The muscle must be
freed quite proximally, especially on its lateral side, to achieve any
significant rotation of the muscle into the wound (Fig. 46.19).
Crisscross release of the soleus myofascia can be done on the deep or
anterior surface of the muscle to expand the size and the dimensions of
the flap (Fig. 46.20).
 |
|
Figure 46.17.
The anterior border of the Achilles is identified and retracted with Alice clamps to aid dissection of the posterior surface of the soleus from the tendon. |
 |
|
Figure 46.18. When freed from its anterior and posterior attachments, the soleus muscle is transected distally.
|
with absorbable sutures. It is worth emphasizing that the muscle,
particularly the gastrocnemius, can be split longitudinally, with one
slip obliterating dead space and the remainder addressing the
requirements of the open wound. Finally, a skin graft over the flap is
necessary and can be harvested from the ipsilateral calf, thigh, or
buttock after application of aerosolized thrombin. The thickness of the
graft is usually 0.015 to 0.018 inches (Fig. 46.21).
Alternatively, a myocutaneous flap can be designed, based on
perforators from the gastrocnemius, to include skin and subjacent
subcutaneous tissue (Fig. 46.22).
The skin overlying the muscle is used and can extend 5 cm proximal to
the medial malleolus. The ability to close the donor site must be
considered before executing this myocutaneous flap. This possibility
does not exist with the soleus. Before wound closure, a Jackson–Pratt
drain is placed in the wound. A well-padded short-leg posterior splint
is applied with the foot and ankle in neutral dorsiflexion (Fig. 46.23).
 |
|
Figure 46.19.
Because of the broad attachments on both the tibial and fibular sides, dissection must continue proximally for any significant transposition to be achieved. |
 |
|
Figure 46.20. Scoring of the myofascia on the anterior surface of the soleus allows great dimensions for coverage.
|
than 30 mL per day. The dressings are changed between 3 and 5 days, and
the skin grafts are inspected. At 1 week, the patient is allowed to
place the leg in a dependent position for a short period and the area
is trained to increase the tolerance over the course of the subsequent
3 to 5 weeks. Prolonged dependency is avoided for 6 to 8 weeks to avoid
venous congestion. The timing of weight-bearing ambulation depends
primarily on the orthopedic injury, rather than on the muscle
flap.
The patient is seen weekly in the office until the wound is completely
closed and dry. Patients must be counseled preoperatively about the
deformity caused by muscle rotation, including loss of natural
convexity in the proximal and middle third of the leg caused by
rotation of the gastrocnemius muscle. It is well documented that both
the gastrocnemius and soleus muscles will atrophy over time after
transposition. After a gastrocnemius or soleus muscle flap is
completed, range of motion of the knee and ankle are usually started
during the first week.
 |
|
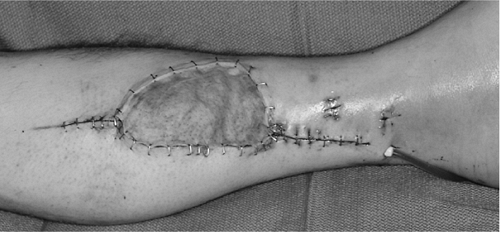
Figure 46.21.
A split-thickness skin graft measuring between .015 and .018 inches can be placed immediately after successful flap transposition. To improve recipient-site aesthetics, we use sheet grafts as opposed and with equal success to meshed grafts. |
 |
|
Figure 46.22.
A cutaneous paddle can be reliably transferred with the gastrocnemius muscle if it contains at least one myocutaneous perforator. |
the gastrocnemius and soleus muscles, flap death is rare. More common,
however, is the development of a postoperative
hematoma,
which requires surgical evacuation, irrigation, and control of the
bleeding site. Loss of power with plantar flexion is rarely a problem
if the gastrocnemius or the soleus muscle is used alone. A combined
gastrocnemius and soleus flap can lead to a greater incidence of muscle
weakness and gait abnormalities. Pain and dysesthesias at the donor
site resulting from flap transposition should be expected during the
first 6 to 8 weeks and should not be considered a complication.
 |
|
Figure 46.23.
At the completion of the procedure, Jackson–Pratt drains are placed on suction, and the extremity is secured in a well-padded posterior splint with the foot plantigrade. |
loss of its middle and distal perforators, the distal end of the soleus
may become devascularized, and if this complication is recognized, it
should be resected. If unrecognized, it can lead to partial flap
necrosis and subsequent wound infection with bone or hardware exposure
or both. Reversed or distally based soleus flaps, although described,
should not be considered reliable alternatives for muscle transposition.
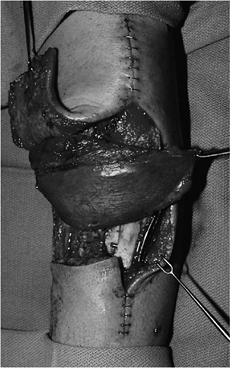
After open reduction and internal fixation (ORIF), the wound broke
down. The gastrocnemius muscle was harvested from the medial side
through a transverse skin incision (Fig. 46.25). The muscle was rotated into place (Fig. 46.26)
with release of its investing fascia, allowing the hardware to be
entirely covered. A split-thickness skin graft was placed. The wound
healed without incident (Fig. 46.27).
 |
|
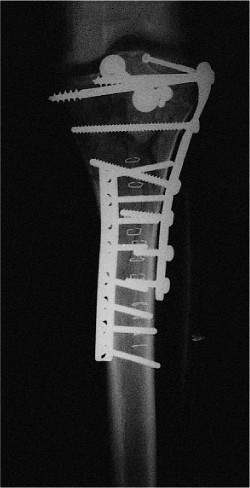
Figure 46.24. Grade IIIB, open, tibial-plateau, and proximal-third fracture after ORIF.
|
 |
|
Figure 46.25. Exposure of the gastrocnemius is made through a transverse posterior incision from the wound.
|
 |
|
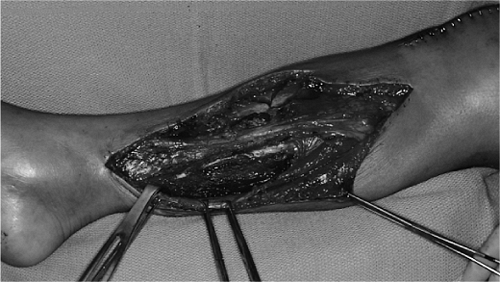
Figure 46.26. When the muscle is freed, it is transposed into place for complete wound coverage.
|
 |
|
Figure 46.27. A well-healed skin graft over the muscle completes the healing process allowing the fracture to unite.
|
MM, Price WM. Gastrocnemius transposition flap in conjunction with limb
sparing surgery for primary bone sarcomas around the knee. Plast Reconst Surg 1984;73:741.
