Vertical Talus
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Vertical Talus
Vertical Talus
Paul D. Sponseller MD
Description
-
Congenital vertical talus is an uncommon disorder, a rigid flatfoot that requires early identification and treatment.
-
Its essence is a dislocation of the talonavicular joint with associated adaptive changes.
-
It may be unilateral or bilateral.
-
>1/2 of affected patients have other neurologic, genetic, or connective tissue disorders.
-
The deformity occurs in utero, but it may be 1st identified any time from infancy to adulthood.
-
Classification:
-
Isolated
-
Syndrome-related
-
-
Synonyms: Congenital convex pes planus; Congenital rigid rocker-bottom foot
Epidemiology
Incidence
-
Rare, but a high association with other disorders and anomalies:
-
10% of children with myelodysplasia have congenital vertical talus (1).
-
It also can be associated with trisomy 13, 15, and 18 and with arthrogryposis or Larsen syndrome.
-
-
In 20–40% of cases, congenital vertical talus occurs as an isolated anomaly (1,2).
-
It affects males and females equally.
Risk Factors
-
Myelodysplasia
-
Ligamentous laxity
-
Arthrogryposis multiplex
Genetics
-
Unknown, but probably variable
-
In some cases, vertical transmission as an autosomal dominant trait with incomplete penetrance has been described.
Etiology
-
Muscle imbalance between the dorsiflexor
muscles of the forefoot and plantarflexor muscles of the hindfoot cause
disruption in the middle of the foot (talonavicular joint). -
Ligamentous laxity and in utero malposition may be causative factors in some cases.
Associated Conditions
-
Arthrogryposis
-
Larsen syndrome
-
Myelomeningocele
-
Trisomy 13, 15, 18
Signs and Symptoms
-
Signs: Moderate reversal of the arch and a crease on the dorsum of the foot near the sinus torsi
-
Symptoms: Lack of push-off strength, painful callus under the head of the talus possible if untreated by walking age
Physical Exam
-
Check the other extremities, as well as the spine, for anomalies.
-
Measure strength in both lower extremities.
-
Observe the foot in stance and gait if the child is walking.
-
It is easily distinguishable from the more common calcaneovalgus and flexible flatfoot.
-
The sole of the foot is convex, has a rocker bottom, and is rigid.
-
The heel is in a fixed equinus with a tight Achilles tendon.
-
The head of the talus is prominent and palpable medially in the sole of the foot.
-
The hindfoot is in valgus.
-
The forefoot is abducted and in dorsiflexion at the midtarsal joint (Fig. 1).
-
As the patient becomes older, the appearance of the foot becomes more distinctive.
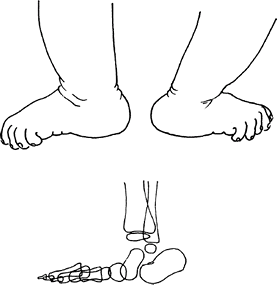 Fig. 1. Vertical talus produces a dorsal crease and a plantar prominence.
Fig. 1. Vertical talus produces a dorsal crease and a plantar prominence.
Tests
Imaging
-
Obtain radiographs.
-
The talus is plantarflexed (on lateral films) and angled medially (on AP films).
-
The navicular is dislocated dorsally and is perched on the neck of the talus.
-
The forefoot is displaced dorsally and abducted.
-
The calcaneus is in a fixed equinus.
-
Only the most posterior aspect of the
talus articulates with the tibia and, in extreme cases, the talus is
parallel to the tibia. -
The diagnosis is confirmed in extreme
plantarflexed views, when the navicular will not reduce, and the line
through the talar axis passes plantar to the metatarsal axis.-
Normal is dorsal to the cuboid and in line with the metatarsal axis.
-
However, the navicular does not ossify until ~3 years of age, in the normal foot or the foot with congenital vertical talus.
-
The position of the navicular may be inferred from the orientation of the first metatarsal.
-
Pathological Findings
-
The calcaneus is in equinus and laterally displaced.
-
The talus is hypoplastic, angled medially, and plantarflexed.
-
Fixed dorsal dislocation of the navicular is noted.
-
Contracture of the Achilles tendon (posteriorly) is evident.
-
Contracture of the toe extensor and the tibialis anterior (anteriorly) is seen.
-
Specially positioned plantar flexion lateral radiograph is helpful (see later).
Differential Diagnosis
-
Calcaneovalgus foot
-
Flexible flatfoot
P.481
General Measures
-
Stretching
-
Surgery
-
If the condition is recognized, surgical intervention is preferred before the patient is 2 years old.
-
Casting and manipulation alone usually are not effective, although they should be used preoperatively to stretch soft tissue.
Activity
Unrestricted
Surgery
-
The essential features are reduction (open or closed) and pinning of the talonavicular joint.
-
Although open surgery previously was the norm (1,3), reduction and percutaneous pin fixation with an Achilles tenotomy recently has become an accepted technique (4).
-
The associated contracted tendons (Achilles and, if needed, anterior tibialis) also should be lengthened.
-
The medial joint capsules may be stabilized, or, in children ≥3 years old, the talonavicular joint may be fused.
-
Children >5 years old may require triple arthrodesis.
-
-
Postoperative percutaneous PINS of the talonavicular joint usually are removed at 6 weeks.
-
Postoperative bracing often is used for a number of months.
-
Late treatment requires subtalar fusion.
-
Recurrent deformity is treated with soft-tissue reconstruction and subtalar fusion.
-
-
In adolescents and adults, salvage is
performed by triple arthrodesis and often requires removal of a large
portion of the talus.
Patients should be followed throughout childhood to monitor the growth of the foot.
Prognosis
If untreated, the condition produces progressive disability.
Complications
-
Complications of nontreatment: Callus, skin breakdown, poor push-off
-
Complications of treatment: Stiffness, residual varus or valgus, need for additional surgery
Patient Monitoring
Even after surgery, the patient should be followed periodically to verify normal growth.
References
1. Morrissy
RT, Giavedoni BJ, Coulter-O’Berry C. The child with a limb deficiency.
In: Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric
Orthopaedics, 6th ed. Philadelphia: Lippincott Williams & Wilkins,
2006:1329–1381.
RT, Giavedoni BJ, Coulter-O’Berry C. The child with a limb deficiency.
In: Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric
Orthopaedics, 6th ed. Philadelphia: Lippincott Williams & Wilkins,
2006:1329–1381.
2. Ogata K, Schoenecker PL, Sheridan J. Congenital vertical talus and its familial occurrence: An analysis of 36 patients. Clin Orthop Relat Res 1979;139:128–132.
3. Seimon LP. Surgical correction of congenital vertical talus under the age of 2 years. J Pediatr Orthop 1987;7:405–411.
4. Dobbs MB, Purcell DB, Nunley R, et al. Early results of a new method of treatment for idiopathic congenital vertical talus. J Bone Joint Surg 2006;88A:1192–1200.
Codes
ICD9-CM
754.69 Congenital vertical talus
Patient Teaching
-
Patients should be informed of the chances of inheritance in future children.
-
The natural history of this condition, if
left untreated, which is severe callus formation, skin breakdown, and
poor push-off, also should be discussed. -
The risk of hip dysplasia should be mentioned and excluded.
-
The possible need for additional surgery should be mentioned.
FAQ
Q: How is vertical talus commonly recognized?
A: By the deep crease in the sinus tarsi and the plantar convexity.
Q: Does it resolve spontaneously?
A: No, it does not.
