Spinal Injuries in Sports
Most acute injuries are related to participation in contact sports,
such as football, wrestling, rugby, and hockey. Most injuries occur
about the shoulder and neck and less commonly in the low back. Other
conditions, such as thoracic outlet syndrome, effort-induced
thrombosis, axillary artery occlusion, and peripheral nerve injuries,
are infrequent but can present similarly to spinal disorders and should
be considered in the differential diagnosis.
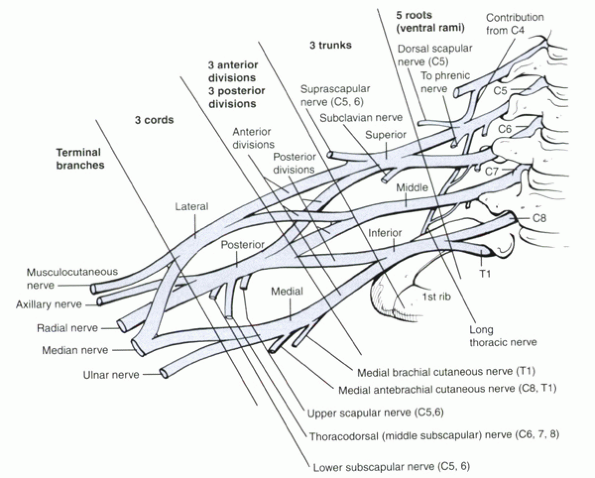
nerve roots and is divided into roots, trunks, divisions, cords, and
branches (Fig. 7-1). Usual mechanisms of injury
are compression and traction. Traction usually is from forceful
separation (i.e., lateral flexion of the neck) of the head from the
shoulder. Arm position at the time of impact usually dictates the
region of the plexus that is injured. If the arm is adducted, the upper
roots are subjected to greater stress. If the arm is abducted, the
lower roots are more susceptible to injury.
trauma or sustained external pressure to regions overlying the plexus,
such as the supraclavicular fossa. A concomitant clavicular fracture
frequently occurs. The nerve roots are compressed at the neural
foramina with neck hyperextension or axial compression or both; neck
hyperextension and axial compression are common in contact sports such
as football.
clinically. Motor and sensory exams and reflexes should be documented
for the upper and the lower extremities. A comprehensive vascular
examination also should be performed. A thorough shoulder exam should
rule out intrinsic shoulder pathology as the cause of symptoms.
confirm the diagnosis. Other diagnoses that may present similarly
should be considered in the differential diagnosis, such as:
-
“Dead arm” syndrome (from anterior instability of the shoulder)
-
Occult fracture or developmental abnormality of the cervical spine
-
Disc herniation
-
Transient quadriplegia
-
Acute brachial neuropathy (Parsonage-Turner syndrome)
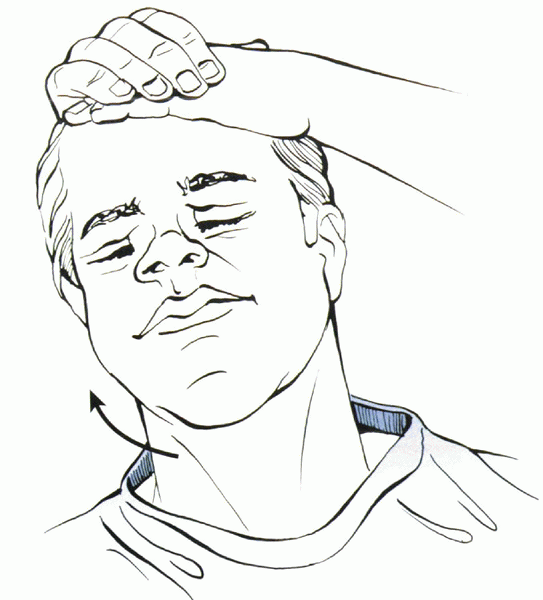
neck suggests a spine fracture. Spurling maneuver can reproduce
radicular pain associated with disc herniation or foraminal stenosis (Fig. 7-2).
Examination of the scapula should include forward elevation and wall
push-off to detect medial scapular winging from serratus anterior
palsy. Trapezius, levator scapulae, and rhomboid dysfunction can cause
lateral winging.
can reproduce symptoms from a traction injury to the upper or lower
trunk. Tinel’s sign with percussion along the supraclavicular fossa may
produce electric shock—like symptoms or pain into the extremity.
contact sports. The “burner” or “stinger” was named after the pain,
tingling, and burning experienced in the upper extremity of the athlete
after contact. These injuries usually occur after the athlete strikes
his or her head against another player, a wall, or a mat. After this
event, the athlete experiences sudden pain, burning, and sometimes
tingling that begins in the neck, radiates into the shoulder, and
continues down the arm and into the hand. Symptoms do not follow a
dermatomal pattern. Weakness of the supraspinatus, infraspinatus,
deltoid, and biceps muscle often is noted, which usually presents hours
to days after the injury.
 |
|
Figure 7-1
A clear understanding of the brachial plexus is important in determining the level of the injury, which can influence prognosis. |
usually result from traction to the brachial plexus or compression of
the cervical root at the intervertebral foramen. Direct impact to the
plexus within the supraclavicular region also has been reported.
Traction injuries can occur with tackling. This causes sudden lateral
deviation of the head away from the affected side and simultaneous
depression of the ipsilateral shoulder. These injuries are more
frequent in high school athletes, possibly because of less developed
supportive neck musculature.
intervertebral foramen. The foramen is dynamically narrowed during
activities that cause cervical spinal extension, compression, and
rotation toward the symptomatic side. These injuries are seen more
commonly in collegiate or professional athletes. Patients present with
more neck pain and diminished range of motion than do patients with
traction injuries. Direct trauma to the supraclavicular region at Erb’s
point can produce a burners syndrome with upper trunk deficits
predominating. Spurling maneuver is used to evaluate compression-type
injuries, whereas the brachial plexus stretch test can be used to
evaluate traction-type injuries.
reported as risk factors for recurrent burners. Logically, this
association has been described for compression-type and extension-type
injuries but not traction mechanisms. Athletes with a history of
recurrent burners and associated degenerative disc disease or
congenital stenosis should abstain from participation in contact sports.
cervical cord or root pathology. This important distinction often is
made on the playing field. By definition, burners present with
unilateral arm symptoms. Athletes who present with bilateral upper or
any lower extremity symptoms are more likely to have had a more serious
spinal cord injury. Focal neck tenderness or severe pain with motion
should raise suspicion for a fracture or ligamentous injury to the
cervical spine. In these cases, the spine should be immobilized using a
collar and backboard, and the patient should be transported to a
hospital for immediate imaging.
cause permanent sequelae. Even with this favorable natural history,
certain restrictions should be placed on athletes after sustaining
these injuries to prevent more severe problems in the future.
At that time, physical therapy can begin and be advanced as tolerated.
Athletes also should be started on year-round trapezial strengthening
programs. Theoretically, strengthening the neck musculature may
increase the shock-absorbing capacity of the cervical spine. Athletes
must fulfill particular criteria before they can return to play (Table 7-1).
 |
|
Figure 7-2
Spurling maneuver—the patient turns head toward the symptomatic arm, while pressure is applied to the cranium. This applies load to the cervical spine and is positive if pain radiates to the affected upper extremity. Caution must be used because this test is nonspecific and must be taken in context with the entire history and physical exam. |
equipment to help prevent injuries. Commonly used devices are thicker
shoulder pads, neck rolls, springs, and the “cowboy collar” (Fig. 7-3).
The devices must fit correctly and be used with properly fitting
shoulder pads to be effective. Educating participants about proper
athletic technique also is important. Proper tackling and blocking
techniques, with avoidance of spearing, should be taught to young
football players as they first are learning the sport.
|
TABLE 7-1 RETURN-TO-PLAY CRITERIA AFTER BURNERS SYNDROME*
|
||
|---|---|---|
|
spinal injuries in sports. Injuries range from cervical sprains to
catastrophic complete spinal cord injuries (SCIs). An estimated 10% to
15% of football players experience an injury to the cervical spine. The
overall incidence of SCI in the high school and college populations is
around 1 in 100,000. Most are incomplete, with preservation of varying
degrees of neurologic function.
of the data compiled by the National Football Head and Neck Injury
Registry showed that axial loading of a slightly flexed head and neck
is the most frequent contributing mechanism of injury. The slightly
flexed posture reverses normal lordosis, potentiating axial load
transmission down the straightened cervical spine. Preexisting spinal
stenosis predisposes to SCI from these mechanisms. Athletes can sustain
cord injury despite the absence of bone or ligamentous disruption. This
phenomenon has been described by Penning. When the cervical spine is in
hyperextension, the cord can be compressed between the posteroinferior
margin of the superior vertebrae and the anterosuperior lamina of the
subjacent vertebra. Infolding of the posterior longitudinal ligament
and the ligamentum flavum contributes to central canal narrowing.
This
transient compression can occur with energies not great enough to cause
discoligamentous or bone disruption. SCI can occur without an
“unstable” spinal injury. Some athletes experience multiple symptomatic
episodes.
 |
|
Figure 7-3 The “cowboy collar” can be used for athletes who are prone to burners syndrome.
|
place patients at high risk for injury. Most cervical spine injuries in
football players result from hyperflexion, but other mechanisms,
including hyperextension, rotation, and lateral bending, have been
reported. Gymnasts may sustain injuries after “missed” maneuvers that
result in an uncontrolled fall. Wrestlers commonly exhibit neck
hyperflexion, but also may endure rotational and horizontal shearing
forces that place great stresses on the intervertebral discs, facet
joints, and spinal ligaments. SCI also has been documented in
noncontact sports, such as diving and surfing. These events usually
result from the individual striking his or her head on the bottom of
the pool or body of water, causing neck hyperflexion.
predispose athletes to SCI. Two forms of cervical stenosis have been
described in athletes: developmental and acquired.
-
Developmental: Otherwise known as congenital stenosis,
is present at birth, and is characterized by shortened pedicles causing
an abnormally narrow canal, sometimes described as funnel-shaped. -
Acquired: The
result of reactive bone thickening and ligamentous hypertrophy that can
result from repeated collisions in sports over time. Other
pathoanatomic features include disc bulges, spondylolysis, and
osteophytes.
have been suggested. Sagittal canal diameter is measured on a standard
lateral cervical spine radiograph. The measurement is recorded as the
anteroposterior distance between the posterior aspect of the vertebral
body and the nearest point along on the spinolaminar junction. Wolf et
al established normal parameters for this dimension. The average
diameters at C1, C2, and C3-7 were 22 mm, 20 mm, and 17mm. Sagittal
canal diameters of more than 15 mm were established as normal, and
diameters of less than 13 mm were defined as stenotic. Evaluation of
the sagittal canal diameter on a lateral cervical spine radiograph is
limited by errors related to magnification, radiographic technique, and
measurement variability.
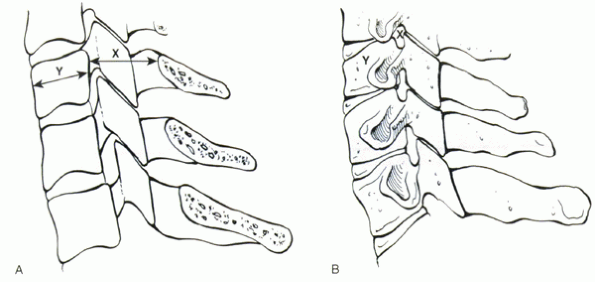
derived a ratio of the anteroposterior canal diameter and the
anteroposterior vertebral body diameter. A value less than 0.8 was
defined as spinal stenosis (Fig. 7-4). Herzog
et al questioned the reliability of the Torg ratio, finding it to have
a high sensitivity but a poor positive predictive value for detecting
clinically significant cervical narrowing. Studies that have evaluated
the cervical spines of clinically asymptomatic professional football
players showed abnormal Torg ratios in 33% to 49%. The high incidence
of these abnormally low ratios is due to the large vertebral body size
in this population, with absolute dimensions of the spinal canal being
adequately capacious for the spinal cord. Magnetic resonance imaging
(MRI) evaluation of these players revealed adequate space available for
the cord in the athletes and no true stenosis.
with either MRI or computeed tomography (CT) myelogram, is becoming the
new standard. Functional spinal stenosis is defined as obliteration of
the cerebrospinal fluid cushion surrounding the cervical spinal cord.
This method of evaluation is being used by many team physicians for
decision making regarding athletes’ return to play and treatment and
activity modifications.
most common complaints among athletes, especially football players.
Patients can sustain an injury to the musculotendinous unit (sprain) or
paraspinal muscle itself (strain): One sprains a tendon but strains a
muscle. Typically an athlete presents with localized neck pain without
radiation to the arms or back. Athletes may have decreased cervical
range of motion secondary to pain. Sometimes the pain may be localized
to one specific cervical level. There are no neurologic deficits.
known contact event are placed in a cervical collar pending further
work-up. Initially the radiographic evaluation includes
anteroposterior, lateral, and odontoid views of the cervical spine. If
these initial radiographs are normal, flexion and extension lateral
radiographs are obtained after the pain and paraspinal muscle spasm
have subsided. Instability based on Panjabi and White’s criteria of
displacement change of 3.5 mm or a change in angulation between two
adjacent vertebral bodies of 11 degrees is assessed on plain lateral
radiographs and preferably on flexion/extension views. Continuing
symptoms and radicular pain may prompt further evaluation with MRI or
bone scan.
the use of a cervical collar and analgesic medications is continued
until pain and spasm subside. After the collar is removed, range of
motion exercises can begin. Return to athletic participation is delayed
until painless full range of motion is achieved. Instability may
necessitate surgical stabilization to prevent future neurologic injury.
collisions or other events leading to axial loading can result in
increased intradiscal pressure. If large enough, cord compression can
manifest as either transient or permanent quadriplegia or
quadriparesis. Patients may present with acute paralysis of all four
extremities and loss of pain and temperature sensation. Patients also
may present with an anterior cord syndrome. Acute radicular symptoms
can occur alone, however. MRI is the study of choice to detect a
herniated disc. Patients with persistent clinical and radiologic
evidence of spinal cord compression should be offered surgery, which
may include anterior cervical discectomy and interbody fusion.
players can reveal asymptomatic cervical spondylosis. In one study, 7%
of freshman college football players had abnormally narrowed disc
spaces. Early degenerative changes have been attributed to years of
repetitive loading from tackling. Severe degenerative changes,
including foraminal stenosis, central canal stenosis resulting from
posterior osteophytes, and loss of normal cervical lordosis, can result
in the classic “spear tackler’s spine.”
 |
|
Figure 7-4 (A, B) The Torg ratio is calculated by dividing the sagittal diameter of the vertebral canal (x) by the diameter of the vertebral body (y).
|
-
Bilateral burning pain
-
Tingling
-
Loss of sensation in the upper or lower extremities
cervical spine is thought to be the mechanism. A pincer mechanism that
theoretically causes a brief compression of the cord is thought to play
a role in the transient nature of the symptoms. Motor deficits can vary
from mild weakness to total paralysis depending on the extent of insult
to the spinal cord. By definition, symptoms are transient, and complete
recovery usually occurs within 10 to 15 minutes, but it may take 48
hours.
usually is negative for fractures or dislocations. Incidental findings,
such as congenital stenosis, spondylosis, Klippel-Feil syndrome, or
evidence of intervetebral disc disease, may be present, however.
originally described by Maroon. This is a variant of a central cord
syndrome. It is characterized by burning dysesthesias and paresthesias
that occur in a glovelike distribution. Symptoms usually last less than
24 hours. This syndrome has been documented after cervical spinal
fractures and in athletes with no radiographic abnormality. Preexisting
cervical stenosis may be a predisposing factor. Reversible MRI spinal
cord signal abnormalities have been documented.
more common in association with fractures and dislocations, although
permanent deficits may occur without such injuries.
in athletes who employ improper tackling technique, using the top of
their football helmet to hit an opposing player head on. This injury is
associated with an increased risk for permanent neurologic damage.
Affected athletes show the following:
-
Narrowing of the cervical spinal canal
-
Persistent straightening or reversal of the normal lordotic curve
-
Concomitant preexisting posttraumatic radiographic abnormalities of the cervical spine
predispose an athlete to spinal injuries by changing the mechanics and
load-dissipating properties of the cervical spine. Congenital anomalies
can occur by failure of formation or segmentation.
segmentation that may involve one or more motion segments. Torg and
Glasgow classified Klippel-Feil syndrome into two types. Type I
involves a long congenital fusion (more than two segments), whereas
type II has one or two fused segments. As the number of fused segments
increases, the ability of the cervical spine to dissipate loads
decreases. More force is concentrated on the unfused motion segments,
increasing the chance for injury in these regions with contact sports.
hypoplasia, or os odontoideum. These conditions can result in
atlantoaxial instability, which places athletes participating in
contact sports at great risk for SCI. In some instances, an athlete can
have failure of formation of the atlantooccipital junction. These
individuals are prone to experience compression of the posterior
columns of the spinal cord at the posterior margin of the foramen
magnum and should be restricted from contact sports.
is usually an incidental finding and asymptomatic. It usually does not
hinder participation in athletics.
catastrophic SCIs were secondary to fracture-dislocations or anterior
compression (burst) fractures in 33% and 22% of cases. In most cases,
the cervical spine is straight on impact, which lessens its ability to
dissipate the load. With increasing loads the spine fails in flexion,
resulting in vertebral body comminution, subluxation, or facet joint
dislocation. Experimentally, Maiman et al found the average axial load
to failure to be less with a straightened versus a normal lordotic
posture. The greatest force applied to the spine was found when the
load was applied to the vertex of the skull. This force decreased as
the load was moved forward on the skull.
fracture-dislocations of the cervical spine, other mechanisms also can
cause injuries. Rotation, extension, and shear forces alone or in
combination have been implicated in various fracture patterns observed
in the cervical spine. Although the multiple fractures experienced by
athletes participating in contact sports such as football are beyond
the scope of this chapter, they have led to the National Collegiate
Athletic Association Football Rule Committee to outlaw the use of one’s
helmet to tackle an opponent.
-
Remove the athlete from play.
-
Institute immediate immobilization of the cervical spine.
-
Perform a neurologic evaluation.
-
Ensure proper airway control in unconscious patients.
-
Remove the facemask (to allow airway
access) without moving the cervical spine. Newer facemasks allow
removal by cutting plastic attachment loops or unscrewing. Older
facemasks may require removal with bolt cutters. As a rule, the
chinstrap and helmet is left in place until arrival at a hospital,
where a coordinated team can perform specialized removal maneuvers.
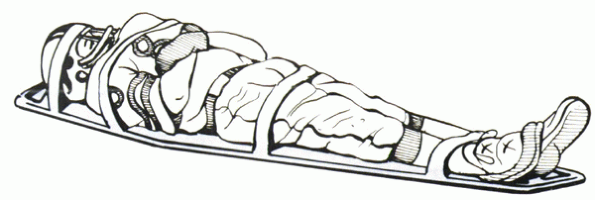
should be transported to a hospital for further evaluation. These
patients should be immobilized on a spine board. Circumferential taping
across the helmet, chest, torso, pelvis, and lower limbs is the most
effective method of securing the athlete to the board (Fig. 7-5). All movements and transfers should use strict logroll precautions.
an event dealing with the cervical spine is a difficult one to make.
Many times the pressures placed on the physician or medical personnel
by the athlete, coaches, and parents can cloud the decision. No
definitive decisions should be made until a complete history and
physical exam have been performed.
after all neurologic symptoms have resolved and full strength and
painless cervical range of motion are present. If this status cannot be
achieved, the athlete is kept out of competition, and cervical
immobilization should be maintained. Radiographic evaluation of
patients with persisting symptoms is recommended.
Patients with acute cervical strains are kept out of competition until
painless full range of motion and full cervical strength are attained.
If cervical spine plain films and flexion/extension films are normal,
the athlete may return to play. It is essential that symptoms have
resolved because reinjury rate in these patients is high.
neurologic sequelae and can lead to decision-making dilemmas. Athletes
with radiculopathy may return to play after symptoms have resolved. If
the disc herniation is causing clinically symptomatic spinal cord
compression, an anterior discectomy and fusion may be considered.
Return to play may be considered if symptoms have resolved, definite
radiographic fusion has been achieved, and full painless range of
motion is restored. Although one-level or two-level fusions are not an
absolute contraindication, many surgeons dissuade athletes from
continuing contact sports.
cervical spine may be at higher risk for SCI. In these patients, the
presence of instability, disc disease, degenerative changes, evidence
of cord abnormalities on MRI, neurologic symptoms lasting more than 36
hours, and more than one recurrence of neurologic symptoms are
contraindications to continued participation in contact sports.
Athletes with radiographic evidence of spear tackler’s spine should not
be cleared for continued play. Torg et al
deemed this condition to be an absolute contraindication to
participation in football or other contact sports. In other cases, one
episode of transient spinal cord neurapraxia is not a contraindication
to returning to play after full resolution of symptoms. The presence of
congenital spinal stenosis alone in an athlete is not an absolute
contraindication to participation in contact sports. These patients and
their families should be counseled adequately, however, as to the
increased risks for SCI.
absolute contraindication to participation in contact sports. All
anomalies, even if found incidentally, should prompt removal from play.
The only exceptions to this rule are Klippel-Feil type II deformities
below C3. In these cases, there is a relative contraindication to
participation in contact
sports. As always, decisions must be made on a case-by-case basis.
 |
|
Figure 7-5
Transfer of the athlete with a suspected cervical spine injury must be performed carefully. Optimally the helmet and body are secured to a rigid backboard using circumferential bands of tape. |
-
Type 1 denotes patients with a neurologic injury. These patients should not be allowed to return to sports.
-
Type 2
injuries consist of transient neurologic deficits without radiologic
evidence of abnormalities. These athletes are allowed to return to
activity unless they have sustained repetitive injuries or had
particular risk factors, such as congenital stenosis. -
Type 3
injuries that have radiographic abnormalities. This group represents a
wide spectrum of disorders with varying recommendations. Athletes who
sustain fractures in the presence of congenital cervical stenosis
should not be cleared for return to contact sports.
 |
|
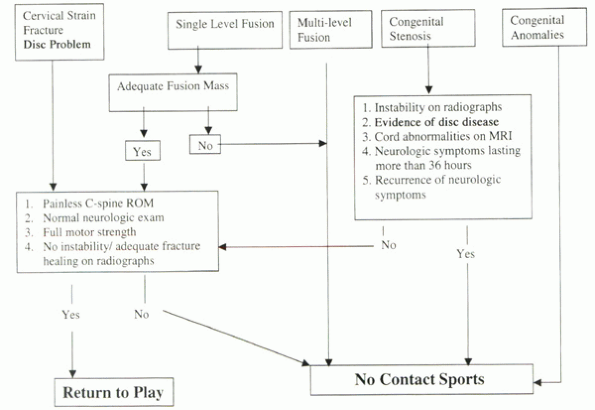
Algorithm 7-1 Return-to-play criteria after cervical spine injury.
|
other radiographic abnormalities, such as congenital fusion, disc
herniations, and degenerative cervical spinal disease, were evaluated
on a case-by-case basis.
This pain can be from an overuse syndrome or acute trauma. Complaints
may range from mild to severe pain after a game or practice. Some
injuries are characteristic of certain sports: lumbar herniated discs
in weightlifters, sacral stress fractures in runners, and spondylolysis
in football players and gymnasts. Position, hours, and number of years
played can indicate overuse. Predominantly axial low back pain suggests
internal disc disruption from degenerative disc disease. Predominantly
leg symptoms suggest radiculopathy from a herniated disc. Infections,
tumors, and inflammatory arthritis more typically are suggested by
nonmechanical back pain. Other red flags are night pain, pain at rest,
fever, or weight loss.
 |
|
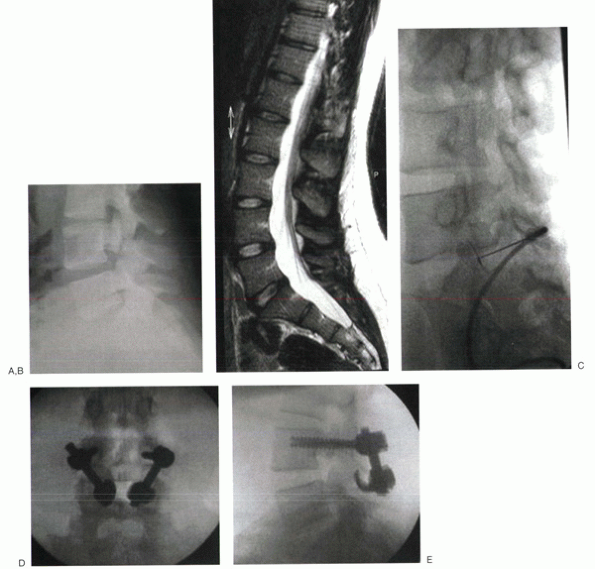
Figure 7-6 In athletes with painful spondylolysis that is recalcitrant to nonoperative care, a pars repair may be performed. (A)
Preoperative lateral radiographs of a 20-year-old college baseball player show a spondylolytic defect of the L4 pars. There is no evidence of spondylolisthesis. (B) For best results, there should be no or minimal disc degeneration. (C) A preoperative pars defect injection temporarily alleviated most or all of the patient’s pain. Although various techniques for pars repair exist, common to all is autograft interposition in and around the defect to encourage healing. Translaminar screws, tension wiring, or pedicle screw-hook constructs provided rigid fixation. In this patient, screws were inserted into the L4 pedicle, and up-going hooks were placed beneath the L4 lamina. (D, E) A short rod was used to connect the two, enabling compression across the grafted defect. (Courtesy of Christopher M. Bono, MD, Boston University Medical Center, Boston, MA.) |
 |
|
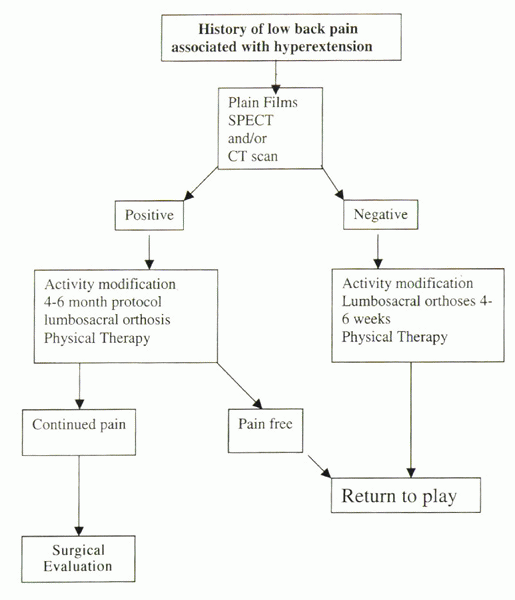
Algorithm 7-2 An algorithmic approach to the diagnosis, return-to-play decision making, and treatment of spondylolysis can be useful.
|
that occurs after acute trauma during a sporting event. Chronic pain
should be assessed according to protocols used for nonathletes for the
specific suspected diagnosis, such as disc herniation, spinal stenosis,
or axial back pain. An adolescent athlete with substantial back pain
lasting longer than 3 weeks should be evaluated with plain lumbar
radiographs and a bone scan or single photon emission computed
tomography (SPECT). A retrospective study comparing 100 adolescent
athletes and 100 adults with acute low back pain showed that 47% of the
adolescent athletes had spondylolysis compared with only 5% of the
adult subjects. The presence and grade of
spondylolysis/spondylolisthesis can influence the decision to allow
return to play.
athletes includes rest and pain control. Rest should be limited to no
more than 48 hours to avoid deconditioning. Medications include
nonsteroidal antiinflammatory drugs and a brief course of mild
narcotics or muscle relaxants. Physical therapy may decrease
recurrences, although no particular regimen is superior. Spinal
orthoses may be used for short-term relief of mechanical symptoms from
spondylolysis or low-grade spondylolisthesis.
8 weeks if they are pain-free, show a full range of motion, and are
neurologically intact. Surgical treatment is specific for the
diagnosis. Among other postoperative considerations, such as solid
fusion, athletes may return to play after lumbar surgery after normal
strength, endurance, and power have been regained. Because
spondylolysis is so commonly encountered, an algorithm for its
treatment is presented (Algorithm 7-2).
Although a single-level fusion is the current standard in recalcitrant
cases, a pars defect repair may be considered in some cases (Fig. 7-6).
JE, Hadley MN, Quigley MR, et al. Management of athletic injuries of
the cervical spine and spinal cord. Neurosurgery 1991;29:491-497.
P, Zurakowski D, Kriemler S, Micheli LJ. Spondylolysis: returning the
athlete to sports participation with brace treatment. Orthopedics
2002;25:653-657.
SA, Callaghan JJ, Albright JP, et al. Cervical spinal stenosis and
stingers in collegiate football players. Am J Sports Med
1994;22:158-166.
PJ, Torg JS. Athletic injury to the cervical nerve root and brachial
plexus. Operative Techniques in Sports Medicine 1993;1:231-235.
JS, Das M. Trampoline-related quadriplegia: review of the literature
and reflections on the American Academy of Pediatrics’ Position
Statement. Pediatrics 1984;74: 804-812.
