RHEUMATOID ARTHRITIS OF THE FOOT
Women are affected more frequently than men, with a peak onset noted in
the third to fifth decade. Rheumatoid arthritis affects both small and
large joints in the upper and lower extremities. Although its onset is
typically insidious, an acute presentation is not uncommon. Chronic
inflammatory changes of rheumatoid arthritis can cause significant
disability of the foot. Initial involvement of the feet is noted in 16%
of patients with acute manifestations of rheumatoid arthritis; however,
the incidence of chronic foot deformities in patients with longstanding
rheumatoid arthritis may approach 90% (65,89).
In chronic rheumatoid arthritis, symmetric involvement is frequently
reported, although early involvement may be asymmetric. Because of
chronic inflammatory synovitis, the metatarsophalangeal joints become
distended. This eventually leads to the loss of integrity of both the
collateral ligaments of the metatarsophalangeal (MTP) joints and the
supporting capsular structures, which sets the stage for progressive
deformity due to loss of stability.
characterized by erosion of the metatarsal heads with cystic
degeneration. As a patient continues to ambulate in the presence of
incompetent ligamentous and capsular structures, subluxation and
eventual dislocation can occur at the MTP joints (17).
In the presence of an active synovitis, the intrinsic muscles are
overpowered by the extrinsic flexor and extensor muscles, and clawing
of the interphalangeal (IP) joints and dislocation of the MTP joints
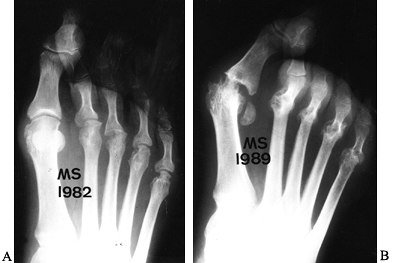
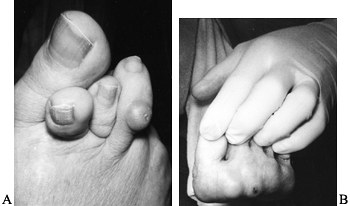
can occur (Fig. 117.1). This clawing leads to a
distal displacement of the plantar fat pad and the formation of
intractable plantar keratoses beneath prominent metatarsal heads (Fig. 117.2).
Marked rigidity of the foot due to ankylosis of the ankle, hindfoot, or
midfoot makes the foot less supple, which compounds forefoot symptoms.
 |
|
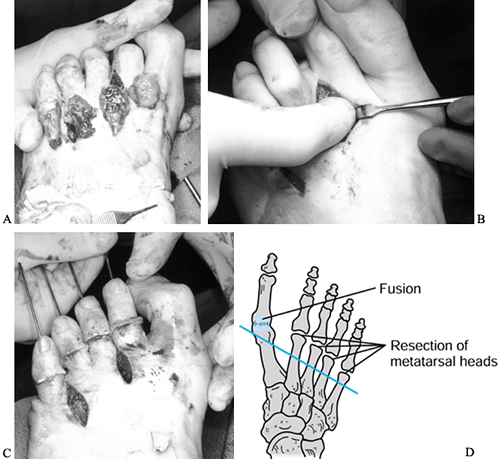
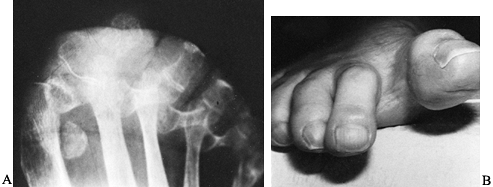
Figure 117.1. A: Rheumatoid arthritis with dislocated third metatarsophalangeal joint and chondrolysis of remaining lesser MTP joints. B: Seven years later, severe hallux valgus with dislocation of the second, third, fourth, and fifth MTP joints has occurred.
|
 |
|
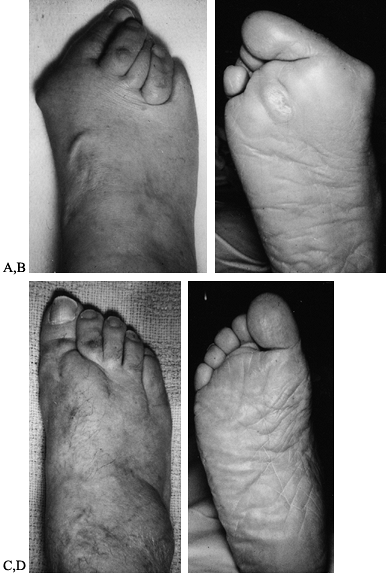
Figure 117.2. A: Normal anatomy of the lesser toe. B:
Pathophysiology of lesser toe deformity in rheumatoid arthritis. (From Coughlin M. The Rheumatoid Foot. Pathophysiology and Treatment of Arthritic Manifestations. Postgrad Med 1984;75:207, with permission.) |
that the forefoot had the greatest propensity for involvement with
longstanding rheumatoid arthritis. Michelson et al. (65)
observed that within the first 3 years following the onset of
rheumatoid arthritis, two thirds of patients developed MTP synovitis.
McGarvey and Johnson (63) and Spiegel and Spiegel (84) reported that approximately two thirds of patients with
chronic rheumatoid arthritis develop subluxation and dislocation of the
lesser MTP joints. Hammer-toe or claw-toe deformities of the lesser
toes vary in frequency from 40% to 80% (63,65,89,93).
As progressive clawing of the lesser toes develops, little stability is
afforded to the great toe, and gradual lateral migration occurs either
beneath or above the second and third toes. This is associated with
progressive articular destruction and resorption of subchondral bone,
which destabilizes the great toe MTP joint. With progressive deformity,
active weight bearing on the first ray lessens and a greater proportion
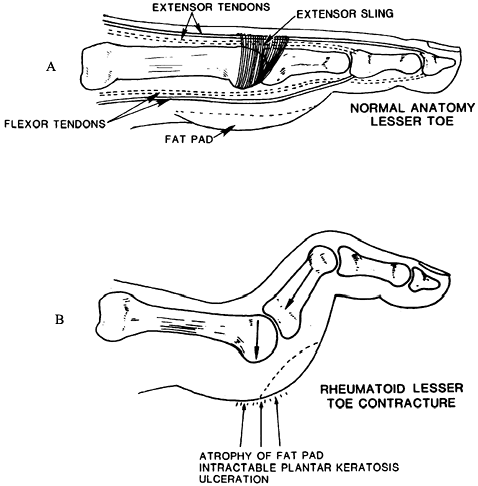
of weight is borne beneath the lesser metatarsal heads (Fig. 117.3).
 |
|
Figure 117.3. A: A typical rheumatoid foot showing severe hallux valgus and overlapping and clawed lesser toes. B:
The plantar surface of a foot, demonstrating prominent metatarsal heads, distal migration of the metatarsal fat pad, and an intractable plantar keratosis beneath the second metatarsal head. C: Postoperative appearance after the first metatarsophalangeal joint fusion and a resection arthroplasty of the lesser MTP joints with hammer-toe repairs. D: Postoperative photograph of the plantar aspect of the foot, demonstrating improved position of the foot and toes with resolution of the intractable plantar keratoses. |
forefoot was involved 10 times more frequently than the hindfoot in
patients with chronic rheumatoid arthritis. Vidigal et al. (93)
noted that two thirds of patients with chronic rheumatoid arthritis
developed mid tarsal involvement, associated with flattening of the
longitudinal arch in approximately 50% of patients. Often a valgus
deformity of the hindfoot occurs in association with this, leading to a
shuffling, flat-footed gait, and with the passage of time, the foot
changes to a passive weight-bearing platform for ambulation.
Chondrolysis associated with chronic synovitis eventually may lead to
tarsometatarsal joint involvement. Likewise, the
first
metatarsocuneiform joint may develop hypermobility with resultant
impaired gait. Transfer metatarsalgia may occur in association with
this first-ray hypermobility. Vainio (89)
noted that 59% of men and 72% of women with chronic rheumatoid
arthritis developed either midtarsal or hindfoot arthritis. Typically,
hindfoot degeneration occurs much later with chronic rheumatoid
arthritis. Spiegel and Spiegel (84) reported
that in patients with rheumatoid arthritis of a duration less than 5
years, only 8% developed arthritis of the hindfoot; however, of those
with a duration greater than 5 years, 25% developed symptomatic
hindfoot arthritis. Gold and Bassett (32) reported that
the talonavicular joint is typically the first hindfoot joint to become involved, and Michelson et al. (65)
reported that degenerative subtalar changes varied in incidence from
32% to 42%. As with the forefoot, the underlying pathophysiology is the
destruction of the capsule and ligaments supporting the joints combined
with concomitant progressive arthritis. Because the function of the
subtalar joint is directly associated with transverse tarsal joint
function, overall instability and deformity of these joints may lead to
altered gait and function with a progressive pes planovalgus deformity.
Likewise, posterior tibial tendon dysfunction can lead to a progressive
unilateral flat-foot deformity (25,45).
With the development of a severe hindfoot deformity, an Achilles tendon
contracture may develop. Thus, at the time of corrective surgery,
lengthening of the Achilles tendon may be necessary.
noted that 63% of patients with rheumatoid arthritis of less than 10
years’ duration developed ankle synovitis. Benson and Johnson (7) and others (73,89,93)
have reported the ankle joint to be involved with a frequency of 4% to
16%. Clearly, hindfoot involvement occurs much more frequently than
involvement of the ankle joint (Fig. 117.4). Wagner (94)
reported on 8,000 clinic visits to Rancho Los Amigos Hospital by
patients with arthritis; in this group, 90 ankle arthrodeses were
performed. Only three ankle arthrodeses were performed for patients
with rheumatoid arthritis. Thus, a very small percentage of patients
had rheumatoid arthritis of the ankle and progressed to surgery.
 |
|
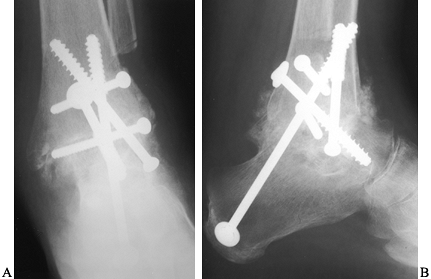
Figure 117.4. Anteroposterior (AP) (A) and lateral (B) radiographs demonstrating ankle arthritis and spontaneous subtalar fusion in a patient with longstanding rheumatoid arthritis.
|
inflammatory arthritis are ill-defined metatarsalgia and forefoot pain.
These complaints are often associated with synovitis and concomitant
intra-articular effusions that impair ambulation. Although ill-defined
metatarsalgia may be misdiagnosed as an interdigital neuroma (90),
in time chronic synovitis may make a diagnosis of rheumatoid arthritis
more obvious. In the presence of forefoot problems, as time passes
synovitis usually develops. Findings include nonspecific forefoot
edema, swelling, tenderness to palpation, and impaired ambulation. In
time, a hallux valgus deformity, subluxation or dislocation of the
lesser MTP joints, and fixed hammer-toe or claw-toe deformities may
develop (Fig. 117.5). Note any hindfoot
deformities and especially posterior tibial tendon dysfunction, pes
planovalgus, and Achilles tendon contracture.
 |
|
Figure 117.5. A:
Dorsal view of a foot with longstanding rheumatoid arthritis, with hallux valgus and subluxation of the lesser toes and hammer-toe deformities. B: Severe intractable plantar keratoses associated with dislocation of the lesser metatarsophalangeal joints. |
typical of synovial inflammatory diseases associated with hyperemia,
periarticular osteoporosis, and soft-tissue swelling. In time, marginal
cortical erosions may develop
that
then progress to central erosions, joint-space narrowing, and eventual
joint subluxation and dislocation as destruction of the articular
cartilage develops. Rheumatoid arthritis tends to involve the first,
fourth, and fifth metatarsal joints early on (32),
specifically the medial aspect of the first, second, third, and fourth
metatarsals and the lateral aspect of the fifth metatarsal. The IP
joints of the toes are typically not involved except for the hallux.
Hindfoot and midfoot deformities include midfoot collapse, pes planus,
and subtalar sclerosis. Look for involvement of the knee and hip
joints, because in general, involvement of these joints requires total
joint arthroplasty before reconstructive foot surgery (20).
|
maintaining a good gait pattern and independent ambulation, or
restoring adequate gait by minimizing inflammation, reducing pain, and
supporting inflamed joints. In the presence of fixed deformity,
surgical correction may be necessary, with arthrodeses and occasional
excisional arthroplasty being the preferred treatments.
swollen and inflamed joints of an acute rheumatoid flare-up.
Application of a cast may be necessary. Roomy footwear, padding, and
prefabricated or custom longitudinal arch supports may be efficacious.
An important aspect of nonsurgical care involves proper shoes and the
modification of shoes. A metatarsal pad placed proximal to an area of
plantar keratoses may diminish tenderness and relieve discomfort
associated with increased pressure. Many patients with early rheumatoid
foot deformities can be adequately treated with a soft-soled and
broad-toed shoe (85). An in-depth shoe with a
custom-molded, a viscoelastic, or a soft insole may help to accommodate
progressive deformities. Working with a pedorthist with skill in the
use of specialized orthopaedic appliances helps to maintain function
and prevent deformities. Orthotic devices help redistribute plantar
weight-bearing forces, which may decrease discomfort associated with
pressure areas, and support unstable joints. Shoes with low heels,
increased depth, and soft leather uppers may be used to accommodate
hammer-toe and claw-toe deformities. A soft-soled rocker-bottom shoe is
helpful in the treatment of not only metatarsalgia but hindfoot
deformities.
how to look for potential breakdown areas in their skin. Patients with
hindfoot and midfoot discomfort with minimal or no deformity can be
adequately treated with a custom arch support or a polypropylene ankle
or foot orthosis. As deformities increase, custom bracing may alleviate
discomfort and provide support. A molded leather ankle lacer with steel
stays can be used inside a shoe and provides significant hindfoot and
ankle support. With progressive deformity or deformity associated with
unrelenting
pain
refractory to conservative treatment, surgical intervention for
forefoot, midfoot, or hindfoot dysfunction may be indicated.
to maintain or attain a plantigrade foot. The clinical course of a
patient’s rheumatoid arthritis determines the treatment program. Direct
treatment toward correction of deformity, restoration of function, and
pain relief. Pharmacologic treatment is an essential part of
controlling the disease process, and involvement of a rheumatologist
for medical management is most important. Rheumatologists often
prescribe salicylates, nonsteroidal anti-inflammatory medications, gold
salts, antimalarials, and immunosuppressive agents for the treatment of
inflammatory arthritis, with the goals being reduction of inflammation
and relief of pain. An occasional intra-articular corticosteroid
injection may be helpful, but oral steroid therapy is employed less
commonly because of the deleterious side effects associated with
chronic use (24). I recommend that methotrexate
be discontinued 1 week before and 1 week after surgery to avoid the
diminished wound-healing capacity often associated with it. See Chapter 99
for more details on medical management. Cover patients who had previous
total joint arthroplasty with perioperative antibiotics at the time of
foot and ankle surgery.
forefoot and hindfoot deformities associated with rheumatoid arthritis.
Stretching exercises for contracted Achilles tendon, manipulation of
ankle and hindfoot joints to maintain or restore range of motion,
muscle-strengthening exercises to assist in maintaining ambulatory
capacity, and the use of ambulatory aids such as crutches, walkers, and
canes may help in maintaining ambulation. With upper extremity
involvement, platform crutches or canes may be necessary. Reduced
ambulation during acute flare-ups, and stretching and exercises for
involved joints are important elements of a physical therapy regimen to
help maintain function in the patient with progressive rheumatoid
arthritis.
throughout the progression of the rheumatoid disease process, surgical
intervention depends on the progression of the disease process and its
severity. Individualize the timing of specific surgical procedures for
each patient. Although sometimes conservative management provides
relief of pain, making surgical intervention unnecessary, a synovectomy
may be indicated to slow the progression of the inflammatory process.
With increasing deformity, the ultimate goal is to prevent the loss of
capacity to ambulate that may occur with progression of the arthritis.
Surgical intervention may be interspersed with long periods of
conservative care. In general, proximal joint surgery (total hip and
knee arthroplasty) should precede foot and ankle surgery. Hindfoot
surgery typically precedes forefoot surgery (22).
The rationale for hindfoot surgery preceding forefoot surgery is that
with a progressive pes planus deformity, a recurrent forefoot deformity
may occur. I prefer to operate on one foot at a time, because the
magnitude of surgery may diminish ambulatory capacity in the
postoperative period.
the treatment of painful joints early in the disease process, before
significant deformity has occurred (2,11,23,24,74,90).
This procedure is contraindicated in the presence of MTP joint
subluxation or dislocation, or with the formation of intractable
plantar keratoses; in these cases, it achieves limited gains. Excision
of hypertrophic synovial tissue may slow or arrest the degenerative
process, decrease distention of MTP joints, and reduce the soft-tissue
deformation that would lead in time to subluxation and dislocation.
Success of surgery depends on the length of remission, but a patient
should be informed that a synovectomy may provide only temporary
relief. Nonetheless, it helps to maintain function of the lesser MTP
joints and toes.
-
Center a dorsal longitudinal incision
over the involved MTP joint. With multiple joint synovectomies, use a
second and/or fourth interspace incision to expose adjacent joints. -
Using the extensor tendon as a guide,
carry the dissection down through the extensor hood and incise the
capsule, exposing the MTP joint. -
Resect proliferative synovial tissue on
the medial and dorsolateral aspects, taking care to remove any synovium
beneath the collateral ligaments. Carry the resection as far in the
plantar direction as possible. -
Close the joint capsule with absorbable sutures, and approximate the skin with interrupted sutures.
-
Carry out a synovectomy of the first MTP
joint through a dorsal longitudinal incision centered over it, using a
technique similar to that described for the lesser MTP joints.
and change it weekly for 6 weeks. Initiate active and passive MTP
range-of-motion exercises 3 weeks after surgery.
have reported good pain relief following synovectomy. Major
complications include injury to the dorsal cutaneous nerve of the
lesser toes. Take care to avoid injury to adjacent sensory nerves. In
time, recurrence of synovial hypertrophy may lead to symptoms and
require further surgery.
hammer-toe and claw-toe deformities that occur in association with MTP
subluxation and dislocation. Whereas a mild deformity may be treated
with passive manipulation and intramedullary Kirschner wire (K-wire)
fixation (closed osteoclasis) (14,23,49,60,70), more severe deformities need a proximal phalangeal condylectomy to achieve realignment with bony decompression (22,23,43,49,95).
-
Center an elliptical incision over the dorsal proximal interphalangeal (PIP) joint of the lesser toe (Fig. 117.6). Excise the dorsal callus, extensor tendon, and joint capsule, exposing the PIP joint.
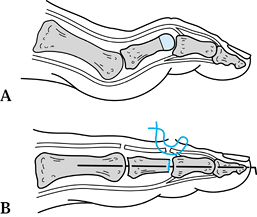 Figure 117.6. Hammer-toe repair. A: Resection of the distal condyle of the proximal phalanx. B: Use of an intramedullary K-wire to stabilize the arthroplasty site.
Figure 117.6. Hammer-toe repair. A: Resection of the distal condyle of the proximal phalanx. B: Use of an intramedullary K-wire to stabilize the arthroplasty site. -
Sever the collateral ligaments on the
medial and lateral aspects, allowing the condyles to be delivered into
the wound. Take care to avoid injury to the adjacent neurovascular
bundles. -
Resect the condyles of the proximal
phalanx in the supracondylar region, and smooth them with a rongeur. As
the toe is brought into correct alignment, if there appears to be any
remaining tension at the PIP joint, resect more bone. You may resect
the articular surface of the base of the middle phalanx with a rongeur
to achieve arthrodesis, but this is optional. -
To stabilize the arthroplasty, introduce
a 0.045 K-wire at the PIP joint, and drive it distally to exit the tip
of the toe. With the toe aligned, drive the pin in a retrograde
fashion, stabilizing the repair. -
If MTP joint arthroplasty is also done,
advance the pin into the metatarsal shaft, stabilizing the arthroplasty
site. Although the use of an intramedullary K-wire to stabilize the PIP
arthroplasty site is a matter of preference, internal fixation appears
to improve the cosmetic result by achieving and maintaining alignment
postoperatively (33,52,59,95).
days. Remove sutures and K-wires 3 weeks after surgery, and support the
toes with a gauze-and-tape dressing for 3 more weeks. Discontinue
dressings 6 weeks after surgery. Avoid constrictive shoe wear for at
least 3 months following surgery.
patients with rheumatoid arthritis have been reported, the goal of
treatment is to achieve and maintain adequate alignment of the lesser
toes. The major complication following surgery is recurrence of
deformity, which in time may lead to hyperextension of the MTP joint.
Recurrent deformity may be due to a lack of initial correction or to
true recurrence. Other complications include prolonged swelling, which
usually subsides in time; molding of the toe to the shape of the
adjacent toes; and, on occasion, a painful arthroplasty site, for which
injection with corticosteroids often gives lasting relief.
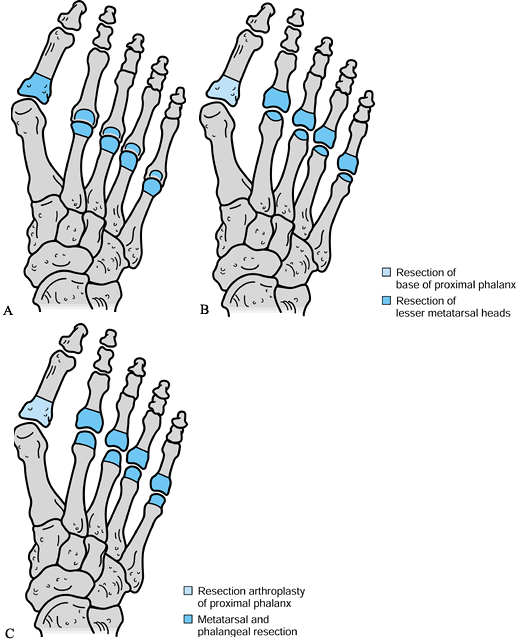
rheumatoid arthritis associated with hallux valgus, metatarsalgia, and
subluxation/dislocation of the lesser MTP joints. The choices of
techniques include a Hoffman procedure (metatarsal head excision) (Fig. 117.7A) (38), a Fowler procedure (resection of the base of the proximal phalanx with beveling of the plantar metatarsal surface) (Fig. 117.7B) (30), and a Clayton procedure (partial proximal phalangectomy combined with metatarsal head resection) (Fig. 117.7C) (13,14 and 15).
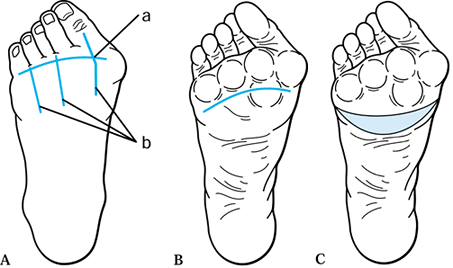
The choice of operative incisions depends on your preference. A
transverse plantar incision, an elliptical plantar incision with
resection of redundant skin and soft tissue, a transverse dorsal
incision, and multiple longitudinal dorsal incisions are all
alternatives (Fig. 117.8). I prefer three
longitudinal dorsal incisions, with the medial incision centered over
the first MTP joint and the two lateral incisions located over the
second and fourth intermetatarsal spaces.
 |
|
Figure 117.7. Alternatives for forefoot arthroplasty. A: Hoffman procedure. B: Fowler procedure. C: Clayton procedure.
|
 |
|
Figure 117.8. Operative incisions. A: (a) Transverse dorsal incision. (b) Longitudinal dorsal incisions. B: Transverse plantar incision. C: Elliptical plantar incision.
|
and a decision must be made as to whether an entire forefoot
arthroplasty should be performed. If one or two joints are involved, an
arthroplasty may be performed on only these joints. However, alert the
patient that the disease process will likely progress in time,
eventually involving the other MTP joints. Rarely is the first MTP
joint spared when the other lesser metatarsal joints are involved. When
the entire forefoot is involved except for the fifth MTP joint, perform
an arthroplasty of the fifth MTP joint as well. Whereas Thomas (85)
recommended surgical resection for a single involved MTP joint, he
recommended that an entire forefoot arthroplasty be performed if three
joints were involved. Marmor (62) and others (9,52,66,72)
recommended that an entire forefoot arthroplasty be performed when two
MTP joints required resection. I support this procedure because it
frequently eliminates the need for later additional surgery with
further involvement of the remaining MTP joints.
-
With the skin flaps slightly undermined, dissect obliquely to each side to expose the adjacent MTP joints.
-
Identify the extensor tendons, but leave them intact except in the presence of significant contracture.
-
Identify the bases of the proximal
phalanges by tracing the insertion of the long extensor tendon. Take
care to protect the neurovascular bundles. -
With sharp dissection, incise the capsule
and expose the metatarsal neck and head circumferentially. Plantar
flexion of the phalanx often delivers the metatarsal head dorsally. -
Resect redundant synovium.
-
With a bone-cutting rongeur, transect the
metatarsal in the metaphyseal region. The amount of bone resection
depends on the shortening that has occurred with the dislocation. -
Grasp and remove the metatarsal head.
Removal of the entire metatarsal head in one piece avoids leaving
remnants of bone, which may later lead to recurrent callosities. -
Bevel the plantar aspect of the metatarsal shaft to reduce any prominence. Resect any synovial cysts or bursa as well.
-
I prefer to preserve the concave surface
of the proximal phalanx (avoiding a partial proximal phalangectomy),
because I believe the base of the proximal phalanx affords significant
stability to the pseudoarticulation at the MTP joint. With
decompression of the MTP joint, I have found that in time the fat pad
routinely realigns, thereby eliminating the need for resection of the
plantar skin (Fig. 117.9A). It is important
that the excisional arthroplasty of the lesser MTP joints achieve
decompression of the MTP joint; usually a space of 1 cm between the
resected metatarsal surface and the base of the proximal phalanx is
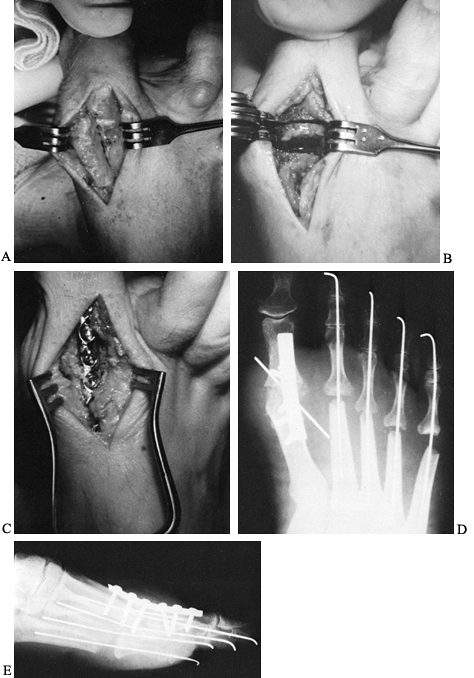
sufficient.![]() Figure 117.9. Metatarsal head resection. A: Excision of the four lesser metatarsal heads through two longitudinal intermetatarsal incisions. B: Introduction of the index fingertip into the resection site. C: Stabilization of the digits with intramedullary K-wires. D: Second and third metatarsals of equal length, and fourth and fifth metatarsals progressively slightly shorter.
Figure 117.9. Metatarsal head resection. A: Excision of the four lesser metatarsal heads through two longitudinal intermetatarsal incisions. B: Introduction of the index fingertip into the resection site. C: Stabilization of the digits with intramedullary K-wires. D: Second and third metatarsals of equal length, and fourth and fifth metatarsals progressively slightly shorter. -
With longitudinal tension on the toe,
insert the tip of your index finger into the resection arthroplasty
site and gauge the adequate amount of resection (Fig. 117.9B).
There should be room for the tip of your finger to be placed
comfortably in this interval. It is important to resect the metatarsal
heads and metaphysis symmetrically. I prefer that the first and second
metatarsals be of equal length, with the third, fourth, and fifth
metatarsals being progressively shortened from medial to lateral. This
helps to avoid an abnormally long metatarsal with consequent
development of intractable plantar keratoses. -
Following metatarsal head resection, correct hammer-toe deformities with a closed osteoclasis or an open hammer-toe repair (see Chapter 113). Introduce an 0.045 K-wire at the PIP joint and drive it in a distal direction to exit the tip of the toe (Fig. 117.9C). Advance it proximally into the metatarsal diaphyses and metaphyses.
-
Embed the K-wire in the proximal
metatarsal base to give stability to the arthroplasty site. Bend the
pin at the tip of the toe to prevent proximal migration. -
Approximate the arthroplasty sites with the skin closure (Fig. 117.9D).
Change it weekly for approximately 6 weeks. Remove K-wires and sutures
3 weeks after surgery. Allow the patient to ambulate in a wooden-soled
postoperative shoe. Immediately after surgery, observe the circulatory
status of the toes. With severe deformities, vascular compromise may
develop, necessitating removal of the K-wires.
showed 89% good and excellent results at final follow-up. Of 1,874
cases reported in many series using various surgical techniques, an
overall satisfaction rate of 81% has been reported (4,5,9,13,16,26,30,35,44,54,55,59,60,62,63,66,68,79,80,91,92,95).
 |
|
Figure 117.10. A: Preoperative radiograph demonstrating hallux valgus and dislocation of lesser metatarsophalangeal joints. B,C: Radiographs taken after MTP fusion and lesser MTP joint forefoot arthroplasty.
|
Metatarsal head excision (Hoffman procedure) has achieved the highest
published success rate—89% good and excellent results (748 of 843
cases) (4,5,9,24,28,33,37,38,43,44,49,66,80,85,91,92,95). I prefer metatarsal head resection to achieve decompression of the MTP joint.
arthroplasty is recurrence of intractable plantar keratoses or recurrent pain due to inadequate resection. Clayton (13,14)
reported a 10% reoperation rate resulting from inadequate resection of
the lesser metatarsal heads. Thus, adequate decompression at the MTP
joint is extremely important to avoid recurrent deformity. While
chronic swelling of the forefoot postoperatively is a frequent
complaint, it usually subsides with time. On the other hand, isolated
resection of one or two metatarsal heads should be avoided, as
intractable plantar keratoses often develop beneath the remaining
metatarsal heads. I believe that revision surgery for the rheumatoid
forefoot becomes necessary most frequently for the following reasons:
(a) irregular lesser metatarsal head resection, (b) limited surgery
with resection of only one or two metatarsal heads, (c) bony regrowth
in the area of the lesser metatarsal head resection, and (d) recurrent
deformity following development of hindfoot or ankle joint problems.
special attention to the resection of the metatarsal heads in a line in
which the first and second metatarsals are of equal length and the
third, fourth, and fifth are progressively shorter, to help avoid
recurrent plantar keratoses. Likewise, meticulous debridement in the
area of the metatarsal head resection is necessary because complete
removal of all bone fragments will minimize bony regrowth. All four
lesser metatarsal heads should be resected: Avoid limited surgery in
which only one or two metatarsal heads are resected. Likewise, in the
presence of hindfoot or ankle joint dysfunction, treat these problems
first. Reserve surgery to correct rheumatoid forefoot deformities for
patients with significant pain and disability, because this is truly a
salvage procedure, and after surgery the lesser toes will have little
active function.
resection arthroplasty for the rheumatoid forefoot frequently fails. McGarvey and Johnson (63)
reported a 67% level of dissatisfaction after Keller arthroplasty
combined with lesser MTP forefoot arthroplasty. They noted recurrent
hallux valgus in 53% and forefoot instability in 27%, and only one
third of their patients reported satisfactory results. They concluded
that first-MTP-joint arthrodesis was preferable to resection
arthroplasty. Later, van der Heijden et al. (91)
reported that 71% of resection arthroplasties of the first MTP joint
were unsatisfactory. Likewise, silastic implant arthroplasty of the
first MTP joint has been recommended as an alternative treatment (23,41).
However, silastic implants have been fraught with both long- and
short-term complications, including implant fracture, synovitis,
recurrent osteolysis, and recurrent pain (81). First-MTP-joint arthrodesis is recommended for the stability that it affords the first ray (17,26,53,57,58,60,67,95).
A resection arthroplasty of the lesser MTP joints affords little
lateral stability to the hallux, allowing lateral displacement. With an
arthrodesis, the first ray bears increased pressure, and a permanently
stable construct is created. Henry and Waugh (36) observed improved weight-bearing function of the great toe following first-MTP arthrodesis, and Watson (95) concluded that arthrodesis was the treatment of choice for correction of a forefoot deformity (Fig. 117.11).
 |
|
Figure 117.11. Arthrodesis of the first metatarsophalangeal joint. A dorsal incision exposing the MTP joint of the hallux (A). Resection of the MTP articular surfaces (B). A small dorsal compression plate fixing the arthrodesis site (C). AP (D) and lateral (E)
radiographs demonstrating compression-plate fixation of the first MTP joint arthroplasty. The excisional arthroplasty of the lesser MTP joints has been stabilized with K-wires. |
stability of the great toe determine the ultimate level of patient
satisfaction. Fitzgerald (29) noted a high
correlation between degenerative IP joint arthritis and the magnitude
of MTP valgus, and he recommended arthrodesis for 20° of valgus or
more. Recommendations for valgus alignment vary from 15° to 30°, and
whereas a straight position (minimal valgus or slight varus) may lead
to pain along the medial border of the hallux as it strikes the toe
box, excessive valgus is often poorly tolerated as well. I usually
recommend arthrodesis in 15° to 20° of valgus because it tends to
attain a more acceptable first-ray alignment in relationship to the
lesser metatarsals. Recommendations for dorsiflexion (in relationship
to the plantar surface of the foot) vary from 10° to 30°, with 20°
being the average recommendation. Women desiring to wear higher-heeled
shoes may desire increased dorsiflexion. Minimal dorsiflexion (less
than 10°) may leave the patient with a complaint of pressure at the tip
of the toe with ambulation, and dorsiflexion greater than 40° may lead
to increased pressure beneath the first metatarsal head. In measuring
the dorsiflexion at the fusion site, take into account the average
plantar inclination of the first metatarsal, which is 15°. Combined
with dorsiflexion of the phalanx of 5° to 15°, this translates into 20°
to 30° of dorsal angulation at the arthrodesis site.
the toe in neutral rotation when arthrodesed. Excessive pronation may
lead to pressure on the medial border of the toenail, causing an
ingrown toenail.
second is not a contraindication for MTP arthrodesis. Harrison and
Harvey (34) and others (54,58,64,67) have reported significant reduction in the 1–2 intermetatarsal angle following fusion. Mann and Katcherian (58) and Humbert et al. (39)
have noted an average decrease in the 1–2 intermetatarsal angle of
approximately 6° following arthrodesis. Thus, a first metatarsal
osteotomy is rarely indicated after MTP fusion.
-
For an MTP arthrodesis, exsanguinate the foot and use a tourniquet.
-
Center a 5 cm dorsal longitudinal
incision over the first MTP joint and protect the adjacent
neurovascular bundles. They are often ill defined in the presence of
chronic soft-tissue inflammation or where previous surgery has been
performed. -
Deepen the dissection along the medial aspect of the extensor hallucis longus tendon to the MTP joint (Fig. 117.11A). Enhance the exposure with a self-retaining retractor.
-
Release the collateral ligaments and the
adductor hallucis. Release the medial and lateral capsules, and resect
the proliferative synovial tissue. -
Initially, soft-tissue release adequately
decompresses the joint. The amount of bony resection depends on the
shortening achieved with the lateral MTP joint arthroplasties. -
Use transverse osteotomies to resect the articular surfaces of the base of the proximal phalanx and the metatarsal head (Fig. 117.11B).
Make these cuts with a small oscillating saw or osteotome. The first
ray at the conclusion of surgery should not be significantly longer
than the adjacent second ray. Usually, if the lateral forefoot
arthroplasties have been performed before first-ray surgery,
appropriate postoperative length is achieved. Frequently, you must
resect additional bone to shorten the first ray. More bone is usually
removed from the distal metatarsal than from the proximal phalanx. -
Resect the medial eminence of the metatarsal.
-
The angle of the osteotomy of the
articular surface of the proximal phalanx and first metatarsal
determines the position of fusion. Valgus of 10° to 20° and
dorsiflexion of 15° to 25° are most common. Usually, women prefer more
MTP dorsiflexion than men. Determining the valgus position of the
arthrodesis site can be difficult. -
Once the MTP joint has been decompressed,
ascertain the flexibility of the metatarsocuneiform joint by
compressing the transverse metatarsal joint. With adequate flexibility,
fixation in 10° to 20° of valgus is appropriate (Fig. 117.11C, Fig. 117.11D and Fig. 117.11E).An alternative to preparing flat arthrodesis surfaces is
P.3109P.3110
to create curved, cup-shaped surfaces. I have designed cannulated reamers (18,19 and 20)
that prepare the phalangeal and metatarsal surfaces so that rotation,
valgus/varus, and dorsiflexion/plantar flexion can be varied
independently without changing other alignment factors. -
First, employ a barrel-shaped reamer to shape the metatarsal metaphysis into a cylinder (Fig. 117.12A), and then use a cup-shaped reamer to create a convex metatarsal surface (Fig. 117.12B). Ream the base of the phalanx to create a concentric concave surface (Fig. 117.12C).
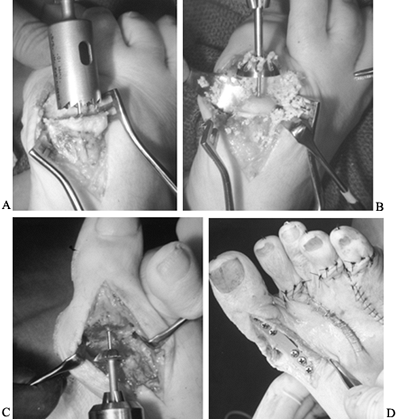 Figure 117.12. Preparing the metatarsophalangeal arthrodesis site with power reamers. A: Shaping the metatarsal metaphysis into a cylinder. B: Creating a convex metatarsal surface. C: Reaming the base of the phalanx to create a concentric concave surface. D: Stabilizing the first MTP joint with a dorsal Vitallium plate. (From Coughlin M. Arthritis. In: Coughlin M, Mann R, eds. Surgery of the Foot and Ankle, 7th ed. St. Louis: CV Mosby, 1999, with permission.)
Figure 117.12. Preparing the metatarsophalangeal arthrodesis site with power reamers. A: Shaping the metatarsal metaphysis into a cylinder. B: Creating a convex metatarsal surface. C: Reaming the base of the phalanx to create a concentric concave surface. D: Stabilizing the first MTP joint with a dorsal Vitallium plate. (From Coughlin M. Arthritis. In: Coughlin M, Mann R, eds. Surgery of the Foot and Ankle, 7th ed. St. Louis: CV Mosby, 1999, with permission.) -
Fixation is possible with crossed
K-wires, compression screws, and multiple intramedullary Steinmann
pins. Application of a Vitallium mini-fragment plate dorsally gives
increased strength of fixation (Fig. 117.12D) (21).
In younger patients who do not have significant osteoporosis, fix the
arthrodesis site with a small Vitallium compression plate. Other
methods may be necessary in older patients with osteoporotic bone. -
Once the MTP joint has been placed in the
appropriate amount of valgus and dorsiflexion, stabilize the fusion
site with an 0.062 K-wire. Introduce it from a plantar/medial direction
and drive it proximally across the MTP joint. It may be used
temporarily during the plate application, or it may be left in place
for 3–4 weeks to augment fixation. -
Alternatively, replace the K-wire with a cross-compression screw. In using the dorsal six-hole mini-compression plate (Fig. 117.12D), bend it to 10° to 20° of dorsiflexion and fix it dorsally with six bicortical screws.
-
Take biplanar radiographs to ensure that the IP joint has not been violated.
-
Approximate the wound with interrupted subcutaneous and skin sutures.
and change it weekly. Permit the patient to ambulate in a wooden-soled
postoperative shoe, initially bearing weight on the heel and the outer
aspect of the foot. A below-knee walking cast is an alternative.
Discontinue dressings or casting 8–12 weeks after surgery, when there
is radiographic evidence of successful arthrodesis.
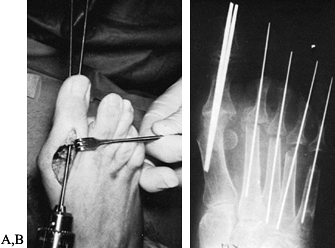
arthroplasty or in the presence of significant osteoporosis,
intramedullary fixation may be necessary to stabilize an arthrodesis
site. Use two double-pointed, threaded 1/8-inch Steinmann pins for fixation (Fig. 117.13).
 |
|
Figure 117.13. Intramedullary fixation of first-MTP-joint arthrodesis. A: Introduction of double-pointed threaded Steinmann pins. B: Radiograph showing the pins stabilizing the MTP joint.
|
-
Attach a drill to the distal end of the
pin, and pull this pin, under power, farther distally until its
proximal tip is flush with the prepared phalangeal surface. Use a pin
cutter to remove 4 inches of the distal aspect of the pin so that it
will not interfere when a second pin is drilled distally. -
Center a second double-pointed, threaded
Steinmann pin just to the medial side of the first pin, and drive it in
a similar fashion across the IP joint and out the tip of the toe. -
Attach the drill to the distal end of the
second pin, and pull this pin distally until its proximal point is
flush with the prepared phalangeal surface. -
Position the toe in the desired amount of
rotation, valgus, and dorsiflexion. With axial compression pressure on
the phalanx across the joint, drive the longest pin in a retrograde
fashion across the MTP joint and into the metatarsal shaft. After it
penetrates the proximal metatarsal plantar medial cortex, further
advancement is not necessary. Use a pin cutter to sever the pin,
leaving 1/8 to ¼ inch extending beyond the tip of the toe for ease of removal after successful fusion occurs (Fig. 117.13B). -
Attach the power drill to the first pin that was placed, and drive it proximally in a similar manner.
-
Following placement, cut the pin with 1/8 inch protruding beyond the tip of the toe.
-
Carry out the subcutaneous and skin closures as previously described. Apply a compression dressing.
is solidly healed, remove the pins under a digital nerve block in an
office setting. Oral analgesics are helpful as well. Use a pin remover
or power drill to remove the Steinmann pins.
reported on MTP arthrodesis in 18 feet with an average 4-year
follow-up. Their results were classified as good or excellent in 16 of
18. Seventeen of 18 went on to successful arthrodesis. Degenerative
arthritis of the IP joint was noted radiographically but was not
believed to be clinically significant (Fig. 117.14). A 92% fusion rate (1,074 of 1,164) with the use of conical reamers has been reported (8,19,21,29,40,42,61,64,75,76,82,96,98). Coughlin and Abdo (21)
reported on 47 patients (58 feet) who were evaluated after
first-MTP-joint fusion. Twenty-eight patients had rheumatoid arthritis.
A 98% fusion rate was achieved. The average correction of the 1–2
intermetatarsal angle was to 9.5° and the hallux valgus angle was
corrected to 17.1°.
 |
|
Figure 117.14. Degenerative arthritis of the interphalangeal joint associated with first-MTP-joint arthrodesis in minimal valgus.
|
nonunion and malunion. Unsuccessful arthrodesis does not necessarily
lead to a painful pseudoarthrosis, and McKeever (64) noted that a nonunion may still give an acceptable result (Fig. 117.15).
Results tend to vary depending on the method of internal fixation and
operative technique utilized. The highest rate of nonunion (23%) (31)
follows crossed K-wire fixation. Malunion in any plane—whether
rotation, varus/valgus, or dorsiflexion/plantar flexion—is poorly
tolerated. IP joint arthritis may develop following MTP fusion and has
been reported to vary from 6% to 60% (6,12,21,22,36,67,76). Coughlin and Abdo (21) reported a 10% incidence of progressive IP joint arthritis, but only 2% were symptomatic.
 |
|
Figure 117.15. Nonunion following arthrodesis. A:
Dislocation of the first and second metatarsophalangeal joints with severe hallux valgus, associated with long-term rheumatoid arthritis. B: Attempted first-MTP-joint arthrodesis. C: Seven years after surgery, the result was successful: painless nonunion with marked improvement in alignment. (From Coughlin M. Arthritis. In: Coughlin M, Mann R, eds. Surgery of the Foot and Ankle, 7th ed. St. Louis: CV Mosby, 1999, with permission.) |
degenerative arthritis of the IP joint and bony insufficiency due to
previous excisional arthroplasty or severe osteoporosis. Arthrodesis in
these situations can be more difficult to achieve.
the compliance required for MTP arthrodesis or in the presence of
recurrent infection or atrophic skin, excisional arthroplasty may be a
simple and expeditious procedure. Resection of the base of the proximal
phalanx detaches both the intrinsic muscle insertions and the plantar
aponeurosis. Although this salvage procedure allows correction of the
deformity by decompression of the MTP joint, it shortens the toe and
impairs strength and control of the hallux. Preoperative counseling is
important to ensure that the patient is aware of these factors.
-
Deepen a longitudinal incision on the
dorsomedial aspect of the first MTP joint along the medial aspect of
the extensor hallucis longus tendon. Take care to protect the dorsal
and plantar neurovascular bundles. -
Incise the MTP joint capsule, and expose the base of the proximal phalanx.
-
Elevate the capsule off the medial eminence, and resect the medial eminence.
-
Dislocate the base of the proximal phalanx. With a power saw, resect approximately one third of the proximal
P.3114
phalanx (Fig. 117.16A). Excessive resection may lead to a weakened or flail toe or a cock-up deformity (22).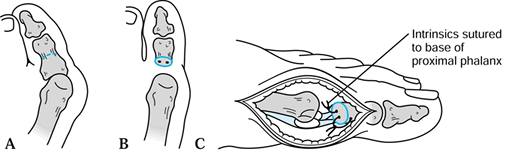 Figure 117.16. An excisional arthroplasty of the hallux (Keller procedure). A: Removal of one third to one half of the proximal phalanx. B: Fixation holes in the base of the proximal phalanx for reattachment of the plantar plate. C: Reattachment of the plantar plate.
Figure 117.16. An excisional arthroplasty of the hallux (Keller procedure). A: Removal of one third to one half of the proximal phalanx. B: Fixation holes in the base of the proximal phalanx for reattachment of the plantar plate. C: Reattachment of the plantar plate. -
I prefer to reattach the plantar plate
and sesamoids to the base of the proximal phalanx. Place the drill
holes 2–3 mm distal to the osteotomized surface (Fig. 117.16B). Reattach the plantar plate to the remaining proximal phalanx with interrupted nonabsorbable sutures (Fig. 117.16C). -
Introduce an 0.062 intramedullary K-wire
at the MTP joint. Drive it distally through the tip of the toe, and
then advance it in a retrograde fashion into the metatarsal head to
stabilize the repair. Bend the pin at the tip of the toe to prevent
proximal migration. -
Reapproximate the capsule and the
subcutaneous tissues with several interrupted absorbable sutures.
Approximate the skin with an interrupted closure.
and change it weekly for approximately 6 weeks. Remove sutures and the
intramedullary K-wire 3 weeks after surgery.
metatarsalgia are major complaints following excisional arthroplasty.
Henry and Waugh (36) reported lateral
metatarsalgia following the Keller procedure and advocated MTP fusion.
You may note a recurrence of hallux valgus after excisional
arthroplasty, especially with progression of the inflammatory process (Fig. 117.17A). A cock-up or claw-toe deformity of the hallux, with detachment of the intrinsic muscle insertion on the base of the
proximal phalanx, has also been reported as a postoperative result of excisional arthroplasty (Fig. 117.17B) (22).
 |
|
Figure 117.17. A: A postoperative recurrence of valgus deformity following a Keller procedure in a patient with rheumatoid arthritis. B: A cock-up deformity following a Keller procedure.
|
 |
|
Figure 117.18. A: Cystic changes of the inferior aspect of the talus associated with hindfoot rheumatoid arthritis. B:
Isolated talonavicular arthritis may be one of the earliest findings with rheumatoid arthritis. (From Coughlin M. Arthritis. In: Coughlin M, Mann R, eds. Surgery of the Foot and Ankle, 7th ed. St. Louis: CV Mosby, 1999, with permission.) |
are midfoot and hindfoot pain, swelling, flattening of the longitudinal
arch, and progressive valgus of the hindfoot. Again, conservative care
includes proper footwear, rest to relieve swollen and inflamed joints
from the stresses of weight bearing, padding, and longitudinal arch
supports. When progressive deformity occurs or unrelenting pain is
refractory to conservative treatment, surgery of the hindfoot may be
necessary.
foot. Rheumatoid vasculitis, while uncommon, may present an increased
risk to wound healing. Recognition of the degree of involvement of
other joints necessitates planning various lower-extremity operations.
With isolated forefoot involvement, occasionally a repair of the
rheumatoid forefoot will precede total hip and knee arthroplasty to
improve ambulatory capacity after surgery. Therefore, if the hindfoot
is mobile and relatively uninvolved, forefoot reconstruction usually
proceeds first. When the midfoot and hindfoot are significantly
involved with rheumatoid arthritis, you may delay surgical intervention
so that total knee and total hip arthroplasty may be performed first.
Then align the hindfoot with respect to the overall axial alignment of
the lower extremity. If both forefoot and hindfoot are involved, the
hindfoot reconstruction should precede the forefoot reconstruction.
that are present help in decision making. When an isolated
talonavicular joint is involved (Fig. 117.18B),
arthrodesis of this joint may give good results. Early talonavicular
fusion may arrest the progression of insidious pes planus and eliminate
a later need for more extensive hindfoot correction (27,71). Involvement of the metatarsocunei form joint also may be treated with isolated arthrodesis of the Lisfranc joint.
relatively uninvolved, and when the valgus deformity of the hindfoot
can be passively corrected, subtalar fusion may be indicated. In this
situation, where valgus is usually not excessive, an in situ
fusion with an iliac crest graft can be performed without significant
alteration of the transverse tarsal joint. The development of a valgus
deformity of the hindfoot can occur because of various pathologic
conditions. It may be associated with erosion of the lateral subtalar
joint, hindfoot ligamentous laxity, or both. It may also be associated
with a valgus deformity of the ankle. When a unilateral valgus
deformity occurs suddenly, suspect a rupture of the posterior tibial
tendon. Whether a soft-tissue reconstruction or hindfoot arthrodesis is
preferable depends on the condition of other hindfoot joints and the
severity of the deformity. See Chapter 118 for a
discussion of the treatment of rupture of the posterior tibial tendon, and Chapter 115 for a description of hindfoot arthrodesis.
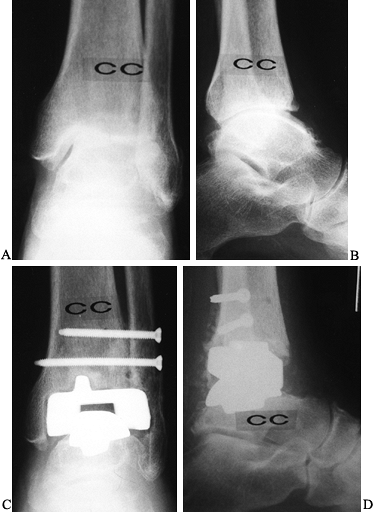
joint or with more severe and irreducible valgus of the hindfoot,
perform a triple arthrodesis, not only to stabilize the hindfoot but
also to correct the deformity (Fig. 117.19). In the patient with hindfoot involvement and a rigid forefoot (Fig. 117.20A), the objective is to obtain a plantigrade foot. Therefore, a triple arthrodesis is usually necessary (Fig. 117.20B) (1).
However, after completion of the subtalar component of this fusion, you
must pronate the forefoot or a plantigrade foot will not be obtained.
This correction is achieved at the transverse tarsal joint.
 |
|
Figure 117.19. A,B: Triple arthrodeses performed for rheumatoid arthritis of the hindfoot.
|
 |
|
Figure 117.20. A:
Preoperative radiograph demonstrating severe pes planovalgus deformity and forefoot deformity associated with rheumatoid arthritis. B: Radiograph following triple arthrodesis and forefoot arthroplasty with correction of deformity. (From Coughlin M. Arthritis. In: Coughlin M, Mann R, eds. Surgery of the Foot and Ankle, 7th ed. St. Louis: CV Mosby, 1999, with permission.) |
forefoot, a subtalar fusion may be feasible, but in all probability a
bone graft to realign the excessive valgus deformity will be necessary.
The objective is to obtain heel valgus of 5° at the completion of the
arthrodesis. Failure to perform a bone graft with a severe valgus
deformity may lead to a recurrence of valgus.
rheumatoid arthritis. When progressive hindfoot valgus has occurred,
hindfoot stabilization is often indicated. The choice between subtalar
and triple arthrodesis depends on several factors, including the
severity of joint involvement, the degree of joint deformity, and the
ankle involvement. Nonetheless, attention to the ankle joint is
necessary, since subtalar or triple arthrodesis with concurrent ankle
disease may eventually progress to a pantalar arthrodesis.
fusion is rarely indicated in rheumatoid arthritis. When significant
degeneration has occurred, surgical intervention may be necessary (Fig. 117.21). Whereas long-term evaluation of total ankle arthroplasty has revealed suboptimal results (47,69,88,99), newer uncemented components have yielded encouraging results (Fig. 117.22) (3,48).
Ankle arthrodesis also may be an alternative for the treatment of
end-stage ankle arthritis refractory to conservative care. On the rare
occasion that subtalar and ankle joints are involved, perform pantalar
arthrodesis. However, even with significant chondrolysis of the ankle
joint, surprisingly good function may be retained.
 |
|
Figure 117.21. AP (A) and lateral (B)
radiographs demonstrating ankle arthrodesis in a rheumatoid patient following spontaneous subtalar arthrodesis at an early age. |
 |
|
Figure 117.22. Rheumatoid arthritis of the ankle. A: AP radiograph. B: Lateral radiograph. C: Postoperative lateral radiograph after total ankle arthroplasty. D: Lateral radiograph.
|
The use of autogenous iliac crest graft depends on the deformity and
the fusion that is attempted. If correction is desired, bone grafting
may be necessary. Occasionally, a bone mill is used in the preparation
of bone. This graft is then placed in the realigned subtalar joint,
which is then stabilized with internal fixation.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
A, Waugh W. The Use of Footprints in Assessing the Results of
Operations for Hallux Valgus. A Comparison of Keller Operation and
Arthrodesis. J Bone Joint Surg Br 1975;57:478.
J, Bourbonniere C, Laurin C. Metatarsophalangeal Fusion for Hallux
Valgus: Indications and Effect on the First Metatarsal Ray. Can Med Assoc J 1979;120:937.
M, Peabody T, Gronley J, Perry J. Valgus Deformities of the Feet and
Characteristics of Gait in Patients Who Have Rheumatoid Arthritis. J Bone Joint Surg Am 1991;73:237.
P, Benson G, Sones D. Resection of Proximal Phalanges and Metatarsal
Condyles for Deformities of the Forefoot due to Rheumatoid Arthritis. Clin Orthop 1972;82:24.
M, Mann R. Arthrodesis of the First Metatarsophalangeal Joint Utilizing
a Dorsal Plate. Presented at the 7th Annual Summer Meeting of the
American Orthopaedic Foot and Ankle Society, Boston, Mass., July 17,
1991.
S, Johnson K. Keller Arthroplasty in Combination with Resection
Arthroplasty of the Lesser Metatarsophalangeal Joints in Rheumatoid
Arthritis. Foot Ankle 1988;9:75.
C, Johnson K, Donnelly R. Surgical Treatment for Mild Deformities of
the Rheumatoid Forefoot by Partial Phalangectomy and Syndactylization. Foot Ankle 1993;14:325.
Loon P, Ariea R, Karthaus R, Steenaert B. Metatarsal Head Resection in
the Deformed, Symptomatic Rheumatoid Foot. A Comparison of Two Methods.
Acta Orthop Belg 1992;58:11.