Radial Head Fractures
IV – Elbow Reconstruction > Part B – Evaluation and Treatment of
Elbow Disorders > 55 – Radial Head Fractures
of the elbow in the adult population, accounting for 1.7% to 5.4% of
all adult fractures. Approximately 85% of these fractures occur in
young, active individuals ranging in age from 20 to 60 years old.
Radial head fractures may occur in isolation or may be part of a more
extensive traumatic elbow injury. An estimated 20% of all acute elbow
injuries have an associated radial head fracture (Fig. 55-1).
In elbow dislocations, a radial head fracture is commonly associated
with other traumatic pathologies including medial collateral ligament
(MCL) rupture, olecranon fracture, and/or coronoid fracture. Therefore,
in the setting of trauma, the elbow must be carefully evaluated to rule
out associated ligamentous and bony pathology.
the outstretched hand with the elbow slightly flexed and the forearm in
a pronated position. Biomechanical studies have demonstrated that the
greatest amount of force is transmitted from the wrist to the radial
head when the elbow and forearm are oriented in this position. During a
fall, the body rotates internally on the elbow; the weight of the body
contributes an axial load to the radius; and a valgus moment is applied
to the elbow since the hand becomes laterally displaced from the body.
The resultant combination of axial, valgus, and external rotatory
loading mechanisms forces the anterolateral margin of the radial head
to come into contact with the capitellum, resulting in a fracture of
the radial head and/or capitellum.
predicting the surgical management of radial head fractures. Type I
fractures include nondisplaced or minimally displaced fractures of the
head and neck, fractures with intra-articular displacement of <2 mm,
or marginal lip fractures. There should be no mechanical block to
forearm rotation; however, rotation may be limited by acute pain and
swelling. The mainstay of treatment of type I fractures involves
nonoperative measures that encourage early elbow and forearm range of
motion. In the acute setting, the elbow hemarthrosis should be
aspirated and injected with local anesthetic to allow a better
assessment of forearm rotation, improve patient discomfort, and
encourage earlier range of motion. The patient is placed into a sling
for comfort and instructed to begin active and passive range of motion
as tolerated within 7 days. Protected weight bearing of the upper
extremity for a period of 6 weeks is encouraged to prevent fracture
displacement. Serial x-ray views are obtained on a weekly basis to
assess for fracture displacement. Open reduction internal fixation
(ORIF) is indicated if the fracture displacement subsequently occurs.
Good to excellent results are expected in most type 1 fractures managed
nonoperatively with a program of early elbow and forearm range of
motion.
of the radial head or neck without severe comminution. These fractures
may have mechanical block to motion or be incongruous. Nonoperative
management of type II fractures should be considered only if elbow
stability is not dependent on fracture fixation and no significant
block to elbow motion is present. In the absence of comminution, these
fractures are usually amenable to ORIF (Fig. 55-2). Recent data suggest that ORIF should be reserved for minimally comminuted fractures with three or fewer articular fragments.1
These data also suggest that fracture-dislocations of the elbow or
forearm managed with ORIF result in less optimal results, especially
with regard to forearm rotation. Other surgical options for type II
fractures include fragment excision, head excision, or radial head
replacement arthroplasty. Fragment excision alone may be indicated when
a fracture fragment blocks forearm rotation but is too small,
comminuted, or osteoporotic to adequately gain fixation (Fig. 55-3).
The fracture fragment should not involve the lesser sigmoid notch or
involve more than one third of the circumference of the head’s
articular surface. Most elbow surgeons discourage fragment excision
because of the possibility of subsequent radial head subluxation.
 |
|
Figure 55-1 Type III radial head fracture. A: Anteroposterior view. B: Lateral view.
|
head or neck fractures that are deemed unreconstructable based on
radiographic and/or intraoperative appearance. Surgical options include
radial head excision with or without radial head replacement
arthroplasty. Prosthetic head replacement is indicated under associated
conditions of instability such as complex elbow instability,
Essex-Lopresti lesion, Monteggia lesion with instability, or a fracture
of a major portion of the coronoid (Fig. 55-4).
low-demand patients without ligamentous instability. Numerous series
report good to excellent results in terms of pain relief and elbow
range of motion after head excision alone. The potential disadvantages
of head excision include decreased grip strength, weak forearm
rotation, and radial shortening with resultant wrist pain. Altered load
transfer at the elbow joint may also lead to the development of early
ulnar trochlear arthrosis and elbow pain. When compared with head
excision, results of metal prosthetic radial head replacement
demonstrate similar range of motion, better clinical scores, less
proximal radial migration, and decreased elbow arthritis (Fig. 55-5).
management of radial head fractures. A full selection of internal
fixation and reconstructive options should be available at the
surgeon’s disposal. Options for internal fixation include various
combinations of threaded K-wires, screws, and plates. The ultimate goal
of these hardware devices is to obtain rigid fixation and hence, allow
early postoperative range of motion. The surgeon should be prepared to
replace the radial head if indicated, preferably with a metallic
prosthesis. The patient is positioned supine on the operating table and
general or regional anesthesia is administered. A sandbag is placed
under the ipsilateral scapula to facilitate positioning of the upper
extremity across the chest. Prophylactic antibiotics are administered
30 minutes prior to making the incision. An examination under
anesthesia is performed prior to prepping and draping the involved
extremity. Examination under anesthesia is absolutely essential in
evaluating elbow and forearm stability and range of motion prior to
proceeding. A skin incision is centered laterally over the lateral
epicondyle and extended distally over the radial head and neck.
Alternatively, a posterior elbow incision just lateral to the tip of
the olecranon may be used in complex injuries in which access to the
radial head, coronoid, medial collateral ligament, and/or lateral
collateral ligament may be required (Fig. 55-6). Full-thickness flaps are developed down to the level of the fascia.
interval between the anconeus and extensor carpi ulnaris. This approach
is disadvantageous for two reasons. First, the approach tends to expose
the radial head too posteriorly, making internal fixation of the
commonly fractured anterolateral head difficult, if not impossible.
Second, iatrogenic injury to the lateral ulnar collateral ligament is
difficult to avoid and may lead to posterolateral rotatory instability.
An alternative approach that splits the extensor digitorum communis is
the preferred approach. This approach is more anterior and hence avoids
disruption of the posterolateral
collateral ligamentous complex (Fig. 55-7).
The lateral epicondyle is identified, and the elbow capsule is elevated
subperiosteally off its anterior aspect. Anterior capsular elevation is
continued distally to the level of the capitellum and elbow joint
taking care to avoid the collateral ligamentous complex posteriorly.
Dissection next proceeds through the annular ligament exposing the
radial head. If the fracture involves only the radial head, minimal
distal (1 to 2 cm) dissection is usually necessary. If the radial neck
is involved, further distal exposure is required. The forearm is fully
pronated and the posterior portion of the extensor digitorum communis
is divided. To avoid placing the posterior interosseous nerve at risk,
distal dissection should not proceed more than two fingerbreadths from
the radial head. If the location of the posterior interosseous nerve is
in doubt, definitive identification of the nerve may be required.
 |
|
Figure 55-2 A: Lateral radiograph of fracture dislocation of elbow type II fracture radial head. B: Anteroposterior radiograph type II fracture radial head. C: Postoperative view: pin and screw fixation of radial head fracture (lateral view). D: Postoperative view: pin and screw fixation of radial head fracture (anteroposterior view).
|
 |
|
Figure 55-3 Attempted screw fixation of radial head fracture.
|
the fracture is thoroughly assessed. The capitellum is also visually
assessed for the presence of an associated chondral injury or
osteochondral fracture. The decision to proceed with fragment excision,
head excision, ORIF, or radial head replacement arthroplasty can be
made at this point. At the time of closure, the annular ligament and
the posterolateral collateral ligament complex (if disrupted) are
repaired. The fascial layer over the common extensor group is closed to
augment lateral elbow stability. Elbow and forearm range of motion and
stability are carefully assessed and recorded.
 |
|
Figure 55-4
Radial head fracture type III with associated coronoid fracture. The radial head was replaced with a prosthesis and the coronoid fracture repaired with suture (second smaller, posterior incision). |
understood when attempting hardware placement into the radial head.
Hardware may be placed into this zone without causing impingement of
the proximal radioulnar joint. The safe zone is defined by a 110-degree
arc centered anterolaterally over the equator of the radial head with
the forearm in neutral rotation. Alternatively, one may identify the
safe zone as a 90-degree arc defined by the right angle from the radial
styloid to the Lister tubercle. Surface anatomy can also help to
identify the proper location for hardware placement.
for provisional fixation. K-wires should be absolutely avoided for
definitive fixation given their tendency for migration postoperatively.
For fractures that do not involve the radial neck, definitive fixation
is typically obtained by using small screws (sizes 1.5, 2.0, or 2.7 mm)
and 3.0-mm cannulated screws. Screws should be countersunk beneath the
articular surface but not protrude through the opposite cortex.
Fractures involving the radial neck are often impacted and require bone
grafting to elevate the radial head. These fractures may be amenable to
screw and/or plate fixation. One technique that has been successful in
the authors’ experience avoids the inherent problems associated with
plate fixation for impacted neck fractures. In this technique, the
radial head is first elevated to its anatomic position and temporarily
secured using threaded K-wires. Screws are then placed obliquely from
the radial head proximally to the opposite cortex of the radial neck
distally. This arrangement may be likened to a bar stool in which the
seat (the radial head) is supported by the eccentrically
arranged
legs (the screws). The resultant bony defect in the radial neck
secondary to impaction is filled with autogenous bone graft or bone
graft substitute. This technique has several advantages over plate
fixation for radial neck fractures. First, screws are less bulky than
plates and may decrease annular ligament impingement. Second, placement
of screws generally requires less dissection and periosteal stripping,
which may lessen the amount of blood supply disruption to the neck and
decrease risk of injury to the posterior interosseous nerve. These
advantages should theoretically result in decreased postoperative
stiffness, painful hardware, heterotopic ossification, proximal
radioulnar synostosis, and nonunion rates. If plate fixation is chosen,
low-profile plates are necessary given the close proximity of the
annular ligament and paucity of overlying soft tissues. Minicondylar
L-plates, T-plates, and fixed-angled blade plates are all available for
radial head and neck fixation.
 |
|
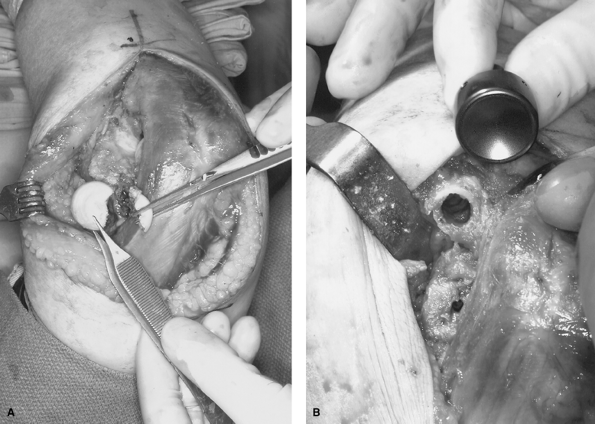
Figure 55-5 A: Type III radial head fracture. Attempt at open reduction internal fixation was unsuccessful. B: Radial neck has been prepared for implantation of radial head prosthesis.
|
 |
|
Figure 55-6
Postoperative photograph of posterior incision for radial head fracture. This is the standard approach used by the authors because of the pleasing cosmetic result. |
devices. A recent biomechanical study compared the average stiffness of
several radial neck fracture plate fixation constructs axially loaded
in compression.2 The study
demonstrated statistically greater stiffness with a 2.7-mm T-plate
modified with a fixed-angle blade when compared with a 2.0-mm T-plate
and 2.0-mm fixed-angle blade. The investigators also noted increased
proximal screw hole toggle when a fixed-angle device was not used.
Contouring of the plate to the radius was observed to be the most
important factor affecting overall construct stiffness. In another
biomechanical study, investigators found no statistically significant
difference in fixation stiffness when a low-profile blade plate and
3.0-mm cannulated screws were compared, but both constructs were
statistically stiffer when compared with a 2.7-mm T-plate.3
have replaced silicone radial heads as the implant of choice in radial
head replacement arthroplasty. When compared with metal radial heads,
silicone implants are associated with worse clinical scores, increased
elbow arthritis, and increased radial shortening. Furthermore, silicone
implants are associated with increased failure secondary to fracture,
fragmentation, and production of silicone synovitis. Both monoblock and
modular radial head prostheses are now available. Anthropometric
studies of cadaver proximal radii demonstrate that the head is
inconsistently elliptical in shape, the head is variably offset from
the axis of the neck, and the head diameter correlates poorly with the
diameter of the medullary canal of the neck.4
These findings may support the use of modular implants that allow
improved sizing options that more closely approximate the anatomy of
the proximal radius.
described. The annular ligament is incised transversely to expose the
radial head. The appropriate radial head resection guide is used to
determine proper alignment and resection level. The neck should be
osteotomized proximal to the bicipital tuberosity. The medullary canal
of the proximal
radius
is then prepared with a starter awl, burrs, and broaches to accept the
implant. Exposure may be improved by applying varus stress and placing
the forearm in supination. Serial sized broaches are used until a snug
fit is obtained in the canal at the appropriate depth. The
appropriate-sized trial stem is inserted, ensuring that the collar of
the prosthesis is flush with the resected neck. In modular designs, the
trial head is secured to the trial stem, and the elbow and forearm are
placed through a full arc of motion. Tracking as well as the
relationship between the prosthesis and the capitellum are carefully
assessed. Once acceptable alignment and tracking are determined, the
trial components are removed and the final prosthesis is inserted. The
stem may be press-fit or cemented in place depending on the design and
stability of the stem in the medullary canal. The head is inserted over
the taper of the stem and secured using an impactor. Final assessment
of motion and stability of the elbow and forearm is performed.
 |
|
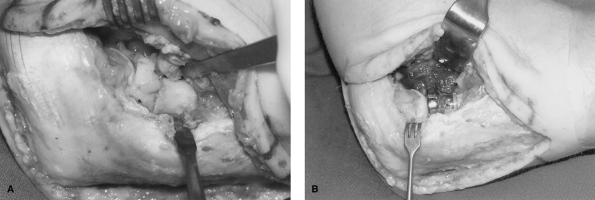
Figure 55-7 A:
Type III fracture. Severe comminution noted at surgery. Surgical approach involved posterior skin incision with split of the extensor digitorum communis (EDC) tendon origin to gain exposure. B: Radial head prosthesis. Note metallic head centered on capitellum. |
require a thorough understanding of elbow anatomy and biomechanics for
proper management. The goals of current management are aimed at
restoring the normal anatomic and biomechanical relationships of the
elbow in an effort to prevent the development of elbow stiffness,
instability, and arthritis. Preservation of the radial head should be
attempted in fractures that are amenable to internal fixation. Severely
comminuted fractures that are not salvageable should be managed with
radial head replacement. Regardless of the type of fracture and chosen
method of management, a program of early range of motion should be
incorporated.
fixation of radial neck fractures: in-vitrobiomechanical analysis.
Transactions of the 44th Annual Meeting, Orthopaedic Research Society. 1998;23: 73 1.
Glabbeek R, Van Riet R, Verstreken J. Current concepts in the treatment
of radial head fractures in the adult a clinical and biomechanical
approach. Acta Orthop Belg. 2001;67: 430–441.
