Posttraumatic Reconstruction—Knee
II – Knee > Part B – Evaluation and Treatment of Knee Disorders >
19 – Posttraumatic Reconstruction—Knee
are among the most common orthopaedic injuries encountered. Although
contemporary methods of ligament reconstruction and open reduction and
internal fixation (ORIF) can result in excellent long-term outcomes,
occasionally posttraumatic arthritis can result. Reconstructive options
include some form of osteotomy, arthrodesis, or arthroplasty.
Challenges include stiffness, scarring, bony defects, malalignment,
presence of extensive (often broken) hardware, and compromised soft
tissues, Reconstructive decision making is based on patient age,
activity, and the anatomic location and extent of damage to the
articular surface. This chapter reviews reconstructive options for
patients with posttraumatic arthritis of the knee.
whether the prior injury involved fracture of the distal femur,
proximal tibia, or patella or was purely ligamentous. Some guiding
principles, however, are common to all such evaluations. First and
foremost, careful evaluation of the patient’s complaints is important.
The location and quality of pain, gait disturbance, and deformity
should be ascertained. Preoperative range of motion (ROM) should be
documented, as multiple studies have demonstrated that postoperative
ROM correlates with preoperative ROM. These knees can be quite stiff
from posttraumatic arthrosis and multiple prior operations.
should be evaluated. The status of the extensor mechanism, any
contractures, and the status of the collateral ligaments should be
documented. The neurovascular status of the limb should be carefully
evaluated and documented.
views are necessary to evaluate alignment, bony deficiency, location of
hardware, and anatomic location of degenerative change. Long-standing
so-called hip-to-ankle radiographs can assist the surgeon in evaluating
angulatory deformity.
status of a fracture union. In this situation, conventional or computed
tomography can assist in evaluation of healing status.
including cessation of tobacco use, if possible. With a history of an
open fracture or failed internal fixation, a complete blood count (CBC)
with differential, sedimentation rate, and C-reactive protein should be
obtained if there is any suspicion of infection. Aspiration of the knee
may provide useful information in selected cases.
reconstruction around the knee is choosing the right operation for the
patient. In most instances arthroplasty is chosen; occasionally the
decision making is more complex (Fig. 19-1).
Consider, for example, a 30-year-old overweight laborer with painful
tricompartmental disease after an open knee dislocation with a prior
vascular repair and free flap with current range of motion of 30 to 60
degrees. Although treatment should be individualized after a thorough
discussion of various options with the patient, some general principles
should be followed.
arthroplasty and younger, more active patients are offered osteotomy or
arthrodesis. In general, younger patients with single-compartment
degenerative change and angular malalignment are selected for
corrective osteotomy. Patient expectations, age, activity, and status
of the articular
surface all guide decision making. The author has found that most patients are not willing to accept an arthrodesis.
 |
|
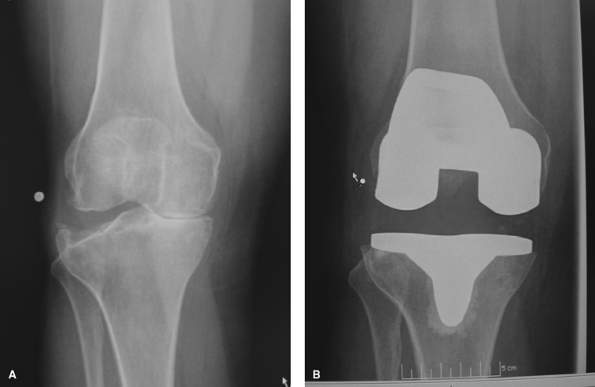
Figure 19-1 A: Posttraumatic degenerative joint disease (DJD) after tibial plateau fracture. B: Treated with total knee arthroplasty.
|
elsewhere in this text. Therefore, we will focus on the specific
technical considerations for arthroplasty in this setting.
implants used to treat fractures about the knee. Typically it is wise
to remove hardware that is symptomatic or that will interfere with the
arthroplasty. In certain situations, it may be preferable to remove
only a portion of the hardware. For example, a long lateral plate on
the tibia may be left in situ, simply removing the proximal screws that
interfere with tibial tray implantation. This avoids the need for
extensive soft tissue dissection and avoids the need to bypass multiple
stress risers distally in the tibial shaft. These can be sites of
cement extravasation or postoperative fracture. In situations where
extensive hardware must be removed, especially through multiple
incisions, it may be best to remove the hardware in a first operation,
then perform the definitive reconstruction after the soft tissue has
recovered. When infection is a concern, the reconstruction should be
staged. The author prefers to remove hardware only if it precludes
performance of the arthroplasty or if it is symptomatic.
nonideal location for total knee arthroplasty (TKA). Typically the most
recent or most lateral incision should be chosen that avoids the
elevation of a large subcutaneous flap. A preoperative consultation
with a plastic surgeon may be helpful in more complex cases. In some
cases, especially those with prior skin grafts or very adherent skin
over the patellar tendon or tibial tubercle, one may consider
preparatory gastrocnemius flap coverage prior to arthroplasty. The TKA
is then planned after flap maturation and soft tissue recovery. This
may avoid a situation in which a flap is required after skin breakdown
with the prosthesis already implanted.
arthritis, and it makes exposure more difficult. General principles for
safe exposure include careful protection of the patellar tendon with
sequential release of scarring in the suprapatellar area, gutters, and
peritendinous tissue. The so-called quadriceps snip can be a useful
technique. The author prefers to perform an arthrotomy gradually
traversing the quadriceps tendon and extending laterally into the
vastus lateralis musculature. This leaves a long area of tissue for
subsequent repair. Combined external
rotation
of the tibia, resection of the cruciate ligaments, and a proximal
medial tibial “peel” is generally adequate. Patellar subluxation,
rather than eversion, may be preferred. These typical exposure
techniques are commonly used during revision arthroplasty and are
covered in greater detail elsewhere in this text. The author prefers to
avoid the so-called quadriceps turn down and tibial tubercle
osteotomies when possible. The turn down may devascularize the tendon
and patella, and the tubercle fragment may be difficult to reattach
with a previously fractured tibia.
reduction and internal fixation (ORIF) techniques and implants.
However, occasionally the patient may present with a malunion that
makes traditional TKA difficult or impossible. Long-standing
hip-to-ankle radiographs are essential. By templating the amount of
bone resection necessary to achieve a normal limb axis and horizontal
joint line, the surgeon can determine whether corrective osteotomy
should be performed prior to arthroplasty (Figs. 19-2A, B).
If excessive bone would need to be resected to perform the arthroplasty
(for example, the distal femoral resection would compromise a
collateral ligament), the malunion should be corrected prior to TKA.
Although rare, rotational malunion can occur, typically of the distal
femur. A CT scan, including cuts through both femoral necks and both
distal femoral epicondyles, can quantify the rotational deformity
preoperatively. Because component rotation affects patellar tracking
and long-term performance of the arthroplasty, malunions such as
malrotations may be corrected prior to surgery. The author has found
retrograde nailing after intramedullary osteotomy and derotation useful
in this setting. This allows visualization of the epicondylar axis and
simplifies hardware removal during later arthroplasty. Angular
deformity of the femur and tibia are also effectively managed by
oblique osteotomy and plating, especially if translation of the
medullary canals precludes nailing techniques. Performing a TKA even in
the case of a minor malunion can be challenging, and extra medullary
alignment guides are often needed (Fig. 19-2).
Alternatively, computer-assisted navigation systems may be considered
when conventional jigs cannot be reliably applied. A comprehensive
discussion of deformity correction about the knee is beyond the scope
of this chapter.
 |
|
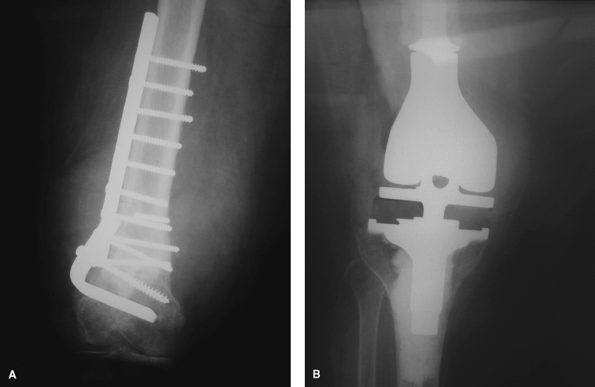
Figure 19-2 Total knee arthroplasty after distal femur malunion, anteroposterior (A) and lateral (B) views.
|
regarding TKA versus revision ORIF is based on patient age, status of
the articular surface, and remaining articular bone stock. Nonunions of
fractures of the proximal tibia are rare. If they occur, the options
include revision ORIF and bone graft, or a TKA. No large series of TKA
performed in this setting has been reported. Some have recommended
bypassing the nonunion with a long stem and bone grafting the nonunion
with autologous bone from the bony cuts.
challenges and are more common. Usually it is preferable to obtain
fracture union with revision ORIF if sufficient bone stock remains
distally. Some authors have recommended TKA with intramedullary
fixation of the nonunion using the cut bony fragments as autograft.
Kress et al. reported a series of nine patients treated for
periarticular nonunions with TKA and stems with excellent results.
Haidukewych et al. reported a series of 17 patients undergoing TKA for
failed ORIF or nonunion of the distal femur. Two of three patients
treated with TKA with intramedullary stem stabilization of the nonunion
healed. Anderson et al. achieved successful union in ten patients with
long-stem fixation and autograft. These limited series document that
TKA with stem fixation used to “nail” the nonunion can be effective in
selected cases.
bone stock for conventional arthroplasty or revision ORIF, the use of
distal femoral replacements, so-called tumor
prostheses may be the most predictable option (Fig. 19-3).
These offer the advantage of immediate weight bearing for the typically
elderly population undergoing these surgeries. Cemented fixation in
this setting allows secure initial component fixation in diaphyses that
are typically capacious and osteopenic.
 |
|
Figure 19-3 A, B:
Multiply operated distal femoral nonunion with posttraumatic degenerative joint disease treated with a distal femoral replacement. |
posttraumatic setting are similar to those used during revision
arthroplasty. Generally, defects are managed incrementally with
techniques such as cement fill, cement and screws, metal augmentation
with wedges or cones, or structural allograft as the defect size
increases. Large cavitary deficiencies are rare in this setting but, if
present, can be managed with commercially available metal metaphyseal
cones or impaction bone grafting techniques.
stress risers and unload deficient periarticular bone. In general, if a
metal augment is used, a stem should be used as well. Cemented and
cementless stems can be used effectively, and there are advantages and
disadvantages to each choice. If a long diaphyseal engaging stem is
necessary (for example, to bypass empty screw holes after plate
removal), cementless stems are generally preferred. Cement is used on
the cut bony surfaces and exposed metaphysis, but the diaphyseal
fixation is uncemented. Recent data on the use of this so-called hybrid
stem fixation technique documented excellent results in the revision
setting. Careful preparation of the diaphysis and intraoperative
radiographs are recommended owing to the risk of iatrogenic femur
fracture. Short, uncemented, metaphyseal engaging stems have
demonstrated a concerning rate of failure in recent series and should
not be used. If a short stem is chosen, cementing is a prudent choice.
of translational deformity to avoid component malposition. Commercially
available stems exist that allow the surgeon to choose the optimum stem
position. This may be most useful for diaphyseal engaging stems.
Shorter, cemented stems often can be “cheated” after overreaming to
afford good stability in the face of angular and translational
deformities. Again, careful preoperative templating is critical to
fully understand the deformity and avoid intraoperative difficulties.
Very rarely, a custom component may be necessary.
dislocation is among the most challenging of reconstructions. Residual
tibiofemoral subluxation and varying amounts of ligamentous damage can
make achieving a balanced arthroplasty in this setting very
unpredictable. Careful preoperative examination can alert the surgeon
to ligamentous insufficiency that may require the use of more
constrained implants.
satisfactory knee stability should be used. Although posterior cruciate
ligament (PCL)–retaining designs may be used in selected situations
with minimal deformity, in most posttraumatic cases substitution of the
PCL will facilitate correction of deformity and accurate ligament
balancing.
|
TABLE 19-1 Total Knee Arthroplasty for Posttraumatic Conditions
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
the status of the collateral ligaments. If these designs are chosen,
consideration should be given to the use of a stem on the components
owing to the increased forces the bone/implant interface will
experience. The young patient with the deficient medial collateral
ligament (MCL) presents perhaps the greatest challenge. Advancement of
the native MCL or allograft reconstruction of the MCL may be considered
in this setting. Data are limited on the optimum reconstruction in this
setting. A more neutral limb axis (less overall valgus) should be
considered as well.
low-demand patients with global ligamentous and bony deficiency.
Younger active patients may be better served with arthrodesis; however,
few are willing to accept this option.
having effective reconstruction strategies is important. Younger
patients are typically candidates for joint-preserving options such as
osteotomy or arthrodesis, whereas older patients typically are salvaged
with TKA. Attention to specific details preoperatively and
intraoperatively is necessary to minimize complications. The vast
majority of published series document predictable functional
improvement but higher complication rates when compared with primary
TKA.
SP, Matthews LS, Kaufer H. Treatment of juxtaarticular nonunion
fractures at the knee with long-stem total knee arthroplasty. Clin Orthop. 1990; 260:104-409.
MG, Ballance J, Brick GW, et al. The use of structural allograft for
uncontained defects in revision total knee arthroplasty. J Bone Joint Surg Am. 2001; 83-A:404-411.
J, Malkani A, Paiso JM. Supracondylar distal femoral nonunions treated
with a megaprosthesis in elderly patients: a report of two cases. J Orthop Trauma. 2001; 15:574-578.
EL, Hick DJ, Johnson EE, et al. Total knee replacement including a
modular distal femoral component in elderly patients with acute
fracture or nonunion. J Orthop Trauma. 1995; 9:231-237.
GJ, Berry DJ, Jacofsky DJ, et al. Treatment of supracondylar femur
nonunions with open reduction and internal fixation. Am J Orthop. 2003; 32:564-567.
GJ, Springer BD, Jacofsky DJ, et al. Total knee arthroplasty for
salvage of failed internal fixation or nonunion of the distal femur. J Arthroplasty. 2005; 20:344-349.
KJ, Scuderi GR, Windsor RE, et al. Treatment of nonunions about the
knee utilizing custom total knee arthroplasty with press-fit
intramedullary stems. J Arthroplasty. 1993; 8:49-55.
KJ, Sherman P. Katkin P, et al. Total knee arthroplasty after open
reduction and internal fixation of fractures of the tibial plateau: a
minimum five-year follow-up study. J Bone Joint Surg Am. 2001; 83-A:1144-1148.
