Lisfranc Fracture-Dislocation
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Lisfranc Fracture-Dislocation
Lisfranc Fracture-Dislocation
Simon C. Mears MD, PhD
Clifford L. Jeng MD
Description
-
Dislocation of the TMT joints of the foot (Fig. 1).
-
Can occur at any age
-
Often accompanied by fractures around the TMT joints
-
-
Classification (1):
-
Type A: Total incongruity of TMT joint
-
Type B: Partial incongruity of TMT joint complex, either medial or lateral
-
Type C: Divergent (1st metatarsal medial, 2nd–5th lateral)
-
Epidemiology
Incidence
Lisfranc injuries account for ~1/3 of midfoot injuries (2).
Risk Factors
-
Car accidents
-
Motorcycle accidents
Etiology
-
The mechanism of injury includes a wide
spectrum of causes from low-energy compression and twisting to
high-energy crush injuries. -
Common cause: Car and motorcycle accidents (3):
-
Pressure on a brake pedal with a plantar flexed foot leads to the Lisfranc pattern of injury (4).
-
-
Sporting events (5)
Associated Conditions
-
Comminuted fractures of the metatarsal bases or cuneiforms
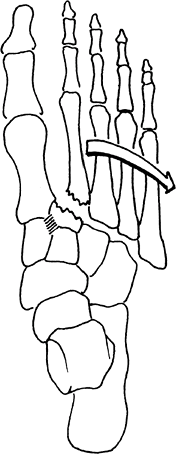 Fig. 1. Lisfranc dislocation occurs at the midfoot joints, usually with substantial trauma.
Fig. 1. Lisfranc dislocation occurs at the midfoot joints, usually with substantial trauma. -
Severe soft-tissue injury
-
Compartment syndrome
-
Open fractures
Signs and Symptoms
-
Pain
-
Swelling
-
Deformity
-
Ecchymosis
-
Difficulty bearing weight
-
Tenderness over midfoot
-
Possible spontaneous reduction
Physical Exam
-
Rotational stress on the forefoot causes pain at Lisfranc joint.
-
Palpation over the 2nd metatarsal base also can cause pain.
Tests
Imaging
-
Radiography:
-
Plain films usually are diagnostic.
-
AP, lateral, and oblique projections are mandatory.
-
On the AP view, the medial margin of the 2nd metatarsal base should be aligned with the middle cuneiform.
-
On the oblique view, the medial base of the 4th metatarsal should be aligned with the medial margin of the cuboid.
-
On the lateral view, an unbroken line should run from the dorsum of the 1st and 2nd metatarsals to the corresponding cuneiform.
-
-
Avulsion fracture of the 2nd metatarsal
base (“fleck” fracture) and compression fracture of the cuboid are
pathognomonic of this condition (6). -
If the diagnosis is uncertain on plain
film, especially if the Lisfranc joint has reduced spontaneously,
stress radiography with fluoroscopy may be helpful in further defining
the instability pattern.
-
-
CT is an important adjunct to plain radiographs.
-
Shows small fractures and displacements that are not visible on plain films
-
In 1 study, radiographs missed the Lisfranc injury in 24% of cases and CT scan revealed the injury (7).
-
Differential Diagnosis
-
Soft-tissue contusion
-
Ligament sprain
-
Isolated metatarsal or midfoot fractures
General Measures
-
Before the patient is taken to the operating room:
-
Compartment syndrome and neurovascular injury should be assessed.
-
The foot is splinted and kept elevated until surgery.
-
-
The goal of treatment is to achieve and maintain anatomic reduction of the joints while the ligaments heal.
-
Usually requires surgical intervention
-
-
Before and after surgery: Ice, elevation, and a compression dressing
-
Foot pumps may help reduce foot swelling.
Special Therapy
Physical Therapy
-
Patients should be referred for gait training on a nonweightbearing basis postoperatively.
-
Edema control and ROM of the toes and ankle are important to decrease late stiffness.
Surgery
-
Open reduction and internal fixation of joints:
-
Through 2–3 dorsal longitudinal incisions
-
Fixation may consist of Kirschner wires or 3.5-mm cortical screws.
-
If Kirschner wires are used as fixation,
they can be removed in the office at 6 weeks, and the patient may begin
protected weightbearing. -
If screws are used as fixation,
unprotected weightbearing is not permitted until the screws have been
removed, at 10–12 weeks after surgery.
-
-
-
Fusion of the joints with 3.5-mm cortical screws has been advocated by some as primary treatment (8) or as a salvage procedure for later arthritis of the midfoot (9).
P.231
Prognosis
-
Patients with anatomic reduction generally have good results.
-
In 1 study, 11 of 24 patients had a good to excellent result (10).
-
-
Outcomes are worse with nonanatomic reduction and extensive joint injury (11).
-
Patients with worker compensation claims have poorer outcomes (12).
-
The role of joint fusion is controversial.
-
Recently, a randomized study showed that joint fusion gave better results than did reduction and fixation (8).
-
-
Patients with posttraumatic arthritis can undergo salvage procedures with arthrodesis.
Complications
-
Traumatic arthritis
-
Fixed deformity
-
For injuries diagnosed late (7–8 weeks):
-
Poor prognosis
-
Patients may be candidates for primary arthrodesis (13).
-
Patient Monitoring
Follow-up radiographs (at 1-month intervals) should be taken to check for maintained alignment of the Lisfranc complex.
References
1. Hardcastle
PH, Reschauer R, Kutscha-Lissberg E, et al. Injuries to the
tarsometatarsal joint. Incidence, classification and treatment. J Bone Joint Surg 1982;64B:349–356.
PH, Reschauer R, Kutscha-Lissberg E, et al. Injuries to the
tarsometatarsal joint. Incidence, classification and treatment. J Bone Joint Surg 1982;64B:349–356.
2. Richter
M, Wippermann B, Krettek C, et al. Fractures and fracture dislocations
of the midfoot: occurrence, causes and long-term results. Foot Ankle Int 2001;22:392–398.
M, Wippermann B, Krettek C, et al. Fractures and fracture dislocations
of the midfoot: occurrence, causes and long-term results. Foot Ankle Int 2001;22:392–398.
3. Jeffers RF, Tan HB, Nicolopoulos C, et al. Prevalence and patterns of foot injuries following motorcycle trauma. J Orthop Trauma 2004;18: 87–91.
4. Smith BR, Begeman PC, Leland R, et al. A mechanism of injury to the forefoot in car crashes. Traffic Inj Prev 2005;6:156–169.
5. Nunley JA, Vertullo CJ. Classification, investigation, and management of midfoot sprains: Lisfranc injuries in the athlete. Am J Sports Med 2002;30:871–878.
6. Pearse EO, Klass B, Bendall SP. The “ABC” of examining foot radiographs. Ann R Coll Surg Engl 2005;87:449–451.
7. Haapamaki VV, Kiuru MJ, Koskinen SK. Ankle and foot injuries: analysis of MDCT findings. AJR Am J Roentgenol 2004;183:615–622.
8. Ly
TV, Coetzee JC. Treatment of primarily ligamentous Lisfranc joint
injuries: primary arthrodesis compared with open reduction and internal
fixation. A prospective, randomized study. J Bone Joint Surg 2006;88A:514–520.
TV, Coetzee JC. Treatment of primarily ligamentous Lisfranc joint
injuries: primary arthrodesis compared with open reduction and internal
fixation. A prospective, randomized study. J Bone Joint Surg 2006;88A:514–520.
9. Komenda GA, Myerson MS, Biddinger KR. Results of arthrodesis of the tarsometatarsal joints after traumatic injury. J Bone Joint Surg 1996;78A: 1665–1676.
10. O’Connor PA, Yeap S, Noel J, et al. Lisfranc injuries: patient- and physician-based functional outcomes. Int Orthop 2003;27:98–102.
11. Kuo RS, Tejwani NC, Digiovanni CW, et al. Outcome after open reduction and internal fixation of Lisfranc joint injuries. J Bone Joint Surg 2000;82A:1609–1618.
12. Calder JDF, Whitehouse SL, Saxby TS. Results of isolated Lisfranc injuries and the effect of compensation claims. J Bone Joint Surg 2004; 86B:527–530.
13. Aronow MS. Treatment of the missed Lisfranc injury. Foot Ankle Clin 2006;11:127–142.
Additional Reading
Sands AK, Grose A. Lisfranc injuries. Injury 2004;35:B71–B76.
Codes
ICD9-CM
825.25 Metatarsal fracture
Patient Teaching
Patients must be warned about the risks of traumatic arthritis and fixed deformity, which may require later arthrodesis.
FAQ
Q: How long will it take to recover from a Lisfranc injury?
A:
Lisfranc injuries are severe injuries to the midfoot and commonly
require surgery. Recovery takes at least a year. Patients may require
hardware removal. ~25% develop arthritis and may require later fusion.
Lisfranc injuries are severe injuries to the midfoot and commonly
require surgery. Recovery takes at least a year. Patients may require
hardware removal. ~25% develop arthritis and may require later fusion.
