FRACTURES AND DISLOCATIONS OF THE MIDFOOT AND FOREFOOT
rehabilitation of polytrauma patients has documented that patients with
foot injuries often had more long-term morbidity (39).
This research suggests that more attention needs to be paid to what may
have been seen as less serious injuries. Recent publications provide
excellent reviews of this important topic (1,18,29,30,37,40).
navicular, cuboid, three cuneiforms, metatarsals, phalanges, and
sesamoids. The joints discussed are Chopart’s joint, Lisfranc complex,
metatarsophalangeal (MTP) joints, and the interphalangeal joints. It is
important to recognize the close relation of nerves and blood vessels
to the bones and joints in the foot (33). In
particular, the dorsalis pedis artery and the deep peroneal nerve are
at risk in both injuries to and surgery for the Lisfranc complex.
Incisional neuromas are relatively common complications of surgery in
the foot and ankle. A variable number of compartments have been
described in the foot (22,35) that must also be understood
in these injuries. See Chapter 3 on surgical approaches to the lower extremity.
injuries and lawnmower injuries make up a significant subset of
injuries to the foot and ankle (26). Crush
injuries may be combined with degloving when the foot is run over by a
heavy vehicle, but they also occur with direct impact such as dropping
a heavy object on the foot. Lawnmower injuries are heavily contaminated
open wounds with or without fractures and often some soft-tissue
avulsion. These injuries not only damage bones and joints but also
nerves and vascular structures, and can lead to skin necrosis, which is
not evident acutely. Therefore, these wounds often need repeated
debridements and delayed primary closure of the skin. Lawnmower
injuries require urgent treatment, with thorough debridement and
irrigation, and then reassessment of the viability of the affected part
(26). Early administration of intravenous
antibiotics is essential. The principles of management of open
fractures are discussed in Chapter 12.
This makes reduction of a displaced dislocation in this area urgent.
Compartment syndrome in the foot has been well described by Manoli (22), Shereff (35), and others. Diagnosis and investigation of compartment syndrome are discussed in Chapter 13.
Compartment syndrome can occur without bony injury in the foot, but
when it is associated with a Lisfranc fracture dislocation, the
surgical approach for decompression needs to take into consideration
the approach for internal fixation of the underlying bony injury.
Compartment syndrome release can be performed through a single medial
incision, but my preference when it is associated with Lisfranc’s
fracture dislocation is to combine a medial incision with one or two
dorsal incisions. There may be a role for foot pumps to decrease the
incidence of foot compartment syndrome. Patients with calcaneal and
more proximal fractures tolerate this treatment modality more readily.
peripheral neuropathy, particularly in diabetics, a forefoot or midfoot
fracture can lead to the development of a Charcot arthropathy. This is
discussed in detail in Chapter 116 and Chapter 124.
In some acute injuries, the underlying neuropathy may not be
recognized; in other cases, the patient may present with a
well-established neuropathy and advanced deformity so that the
diagnosis of neuropathy is obvious.
In the midfoot and forefoot the most common sites for stress fractures
are the navicular, the base of the fifth metatarsal, the shaft of the
second and third metatarsals, and the sesamoids. Those most resistant
to treatment are the navicular and base of the fifth metatarsal.
Fractures of the sesamoid and middle metatarsals are addressed
elsewhere in this chapter.
 |
|
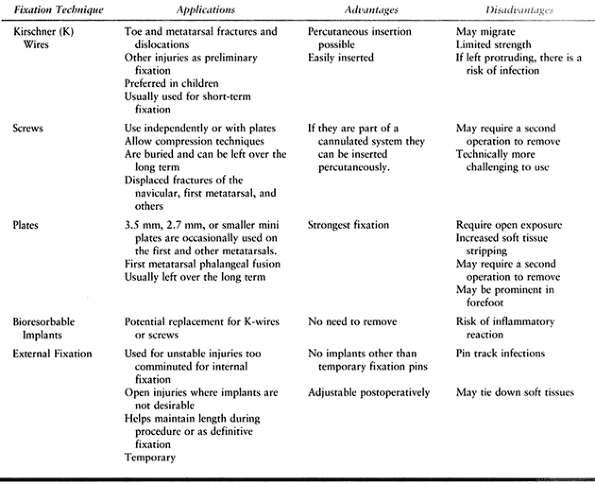
Table 111.1. Applications, Advantages and Disadvantages of Foot Fixation Techniques
|
stabilize forefoot fractures. They are particularly useful where their
role is short-term fixation, particularly of a metatarsal or a toe.
Their role in Lisfranc injuries remains controversial, however. The
disadvantages of using smooth K-wires are migration if they are left
buried and infection if they are left through the skin for prolonged
periods. Therefore, when I repair primarily ligamentous injuries that
require 3 months of immobilization, I prefer to use either a screw or a
threaded K-wire and bury it beneath the skin.
compression and more solid fixation, which is particularly important
for rigid stabilization of the medial three tarsal-metatarsal joints
and for those fractures in which inadequate fixation is likely to lead
to nonunion or delayed union. Cannulated screw systems allow
percutaneous insertion of the implant. When a screw is placed across a
joint, which is particularly relevant in Lisfranc’s injuries, the other
concerns are damage to the articular surface by the larger diameter and
the need to remove the implant. If the screw is placed across a joint
that is essential to the function of the foot, removal is indicated;
otherwise, removal remains controversial unless the implant causes
symptoms. Details of the recommended methods of fixation for individual
injuries are discussed later in this chapter.
time are now available (5).
These implants initially caused some concern because of local
soft-tissue reactions, particularly seromas. The more recent implants
produce less reaction and do have a role, especially for
intra-articular fractures or for temporary (i.e., 6-week to 3-month)
fixation of joints such as Lisfranc’s injuries. Their role in long-term
fixation of the foot and ankle, however, remains to be seen.
cuneiforms, navicular, and cuboid), which when fractured, may be
comminuted and difficult to stabilize with internal fixation. It is
occasionally useful to bridge the area with an external fixator, such
as medially from the talar neck to the first metatarsal (Fig. 111.1C, Fig. 111.1D) (11,15)
to restore the length of the column and reduce the fractures using
ligamentotaxis. External fixation may be used as a temporary device to
provide the reduction. The fracture can then be stabilized by internal
fixation or percutaneous fixation as the definitive method of
treatment, or the fixator can be left in situ.
I have found this particularly helpful in a comminuted navicular
fracture for which such extensive comminution occurred that stripping
the soft tissues to allow adequate reduction might have led to
avascular necrosis. The other role for external fixation is when the
soft tissues are compromised, such as an open fracture or severe
crushing, to provide temporary fixation while the soft-tissue situation
is resolved.
 |
|
Figure 111.1. Lateral (A) and oblique (B) radiographs of a comminuted subtalar and talonavicular fracture dislocation. AP (C) and lateral (D) radiographs demonstrating external fixation to stabilize the medial column.
|
 |
|
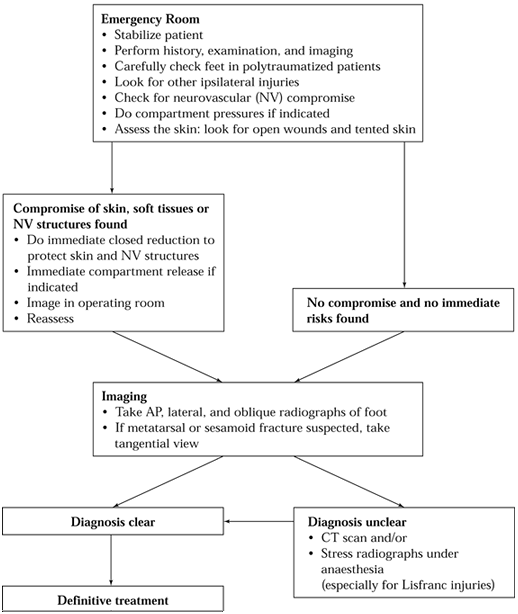
Figure 111.2. Algorithm for assessment of midfoot and forefoot injuries.
|
 |
|
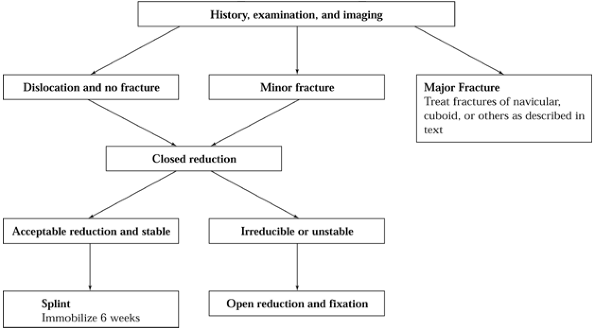
Figure 111.3. Algorithm for Chopart’s joint injuries.
|
of its importance to the function of the foot, particularly in linking
the hindfoot to the forefoot, damage in this area can have significant
consequences to the function of the foot. Main and Jowett (21)
classified midtarsal joint injuries based on the direction of the force
of injury and the deformity that occurred. They described five patterns
of injury; within each, the injuries varied in severity. However, their
classification is not helpful in prognosis or management decisions.
Take a careful history, and ask about the amount of force applied, the
direction of the force, and whether the patient felt a “clunk” as the
joint dislocated or relocated. These injuries are often found in
polytrauma
patients,
in whom the details of the injury may not be available; therefore, any
polytrauma patient with a swollen foot needs careful assessment.
Localize sites of maximum tenderness; test motor and sensory function,
if possible, and gently stress the transverse tarsal joints to look for
excessive mobility.
radiographs of the foot. Findings may include avulsion of the navicular
tuberosity, fractures through the body of the navicular, compression of
the cuboid, or anterior calcaneus. Hermel and Gershon-Cohen (17)
applied the term “nutcracker fracture” to the compression fracture of
the cuboid. True dislocations may be seen on plain radiographs, but
most often, spontaneous reduction of the transverse tarsal joint has
occurred. For this reason, examination under anesthesia is occasionally
warranted if the patient is undergoing surgery for other injuries.
Alternatively, if the patient does not have other major injuries and it
is clinically indicated, local anesthetic injection may allow weight
bearing or stress films to be taken. Further investigation such as
computerized tomography (CT) may be warranted if a significant
intra-articular fracture requires documentation or if the plain
radiographs are not diagnostic. If the patient is seen late with
persistent medial midfoot pain, a bone scan may be warranted to
document an otherwise unrecognized injury (7,12).
to restore the normal anatomy and stability without producing excessive
stiffness. As shown in Figure 111.2, assess
whether immediate treatment is warranted. Treatment may consist of
closed reduction, external fixation, open reduction and internal
fixation, or late reconstruction.
 |
|
Figure 111.4. AP (A) and lateral (B)
radiographs of residual subluxation following closed reduction of a Chopart’s fracture and dislocation in a 9-year-old girl. AP (C) and lateral (D) radiographs of post-open reduction and K-wire fixation. The dorsal capsule was blocking reduction. |
without a major fracture is relatively stable. Immobilize with a
splint, and elevate (no weight bearing) for 1 to 2 weeks to allow pain
to resolve. I recommend using a removable splint or removable cast to
allow range of movement while protecting the foot from loading. If,
however, there is a fracture associated with a dislocation,
particularly a fracture of the navicular, then the injury may be
unstable. If a fracture of the navicular is undisplaced and if closed
reduction produces satisfactory alignment, splint until the swelling is
reduced, followed by a period of immobilization in a short-leg cast for
approximately 6 weeks. Weight bearing depends on the stability of the
fracture. Then encourage range of movement.
avulsion of the navicular tuberosity, open reduction and anatomic
fixation are warranted. Immobilize for 6 weeks until
fracture
healing occurs. Weight-bearing status depends on the stability of the
fracture and the fixation but is generally non-weight bearing for 6
weeks.
unstable, but a compression fracture of the cuboid may shorten the
lateral column, which will have a long-term effect on foot function.
When the lateral column fractures are minor avulsions, such as the
anterior process of the calcaneus or the dorsal lip of the cuboid,
treat symptomatically. Occasionally, late excision of bony fragments is
necessary if they are problematic. If there is a crush injury of the
lateral column with loss of height of the cuboid, however, then
reduction and stabilization are indicated. The same pattern of cuboid
injury may be seen with Lisfranc’s dislocations. The principles of the
different methods of treatment are discussed in relation to the
different fracture patterns.
there is significant loss of medial column length, and when other
methods of fixation are not an option. It is more common to have
lateral column shortening. External fixation may be used if the
fragments are too small to obtain stable reduction with internal
fixation.
-
Plan the insertion of two pins in the calcaneus and two in the fifth metatarsal.
-
Make stab incisions in the skin; be careful to avoid injury to the sural nerve.
-
Insert two pins in a half pin fashion
into the calcaneus and two into the fifth metatarsal using the
technique appropriate for the external fixator that is being used.
Apply the fixator and distract the fracture. -
Expose the fractured bone through a short
longitudinal incision and elevate the articular surface, which can
usually be elevated and aligned to the remaining medial or plantar
articular surface. -
Use a small amount of bone graft, which
can be harvested locally from the calcaneus or malleoli, to fill any
resulting defect and stabilize the fragment. -
Stabilize the fracture with one or two
small threaded K-wires running in the subchondral bone into the
remaining cuboid. Cut the wires off just outside the bone.
fixation, in which case simply elevate the fracture, pack in bone
graft, and use external fixation to control the fracture. If the
fracture fragments are large enough, a screw may be used to stabilize
the fracture fragments. In this case, the external fixator may be
removed or a plate may be applied (see the next section), depending on
the stability of the construct.
fixation are used for displaced fractures of the navicular tuberosity
or displaced fractures of the body of the navicular. The most common
injury is an avulsion fracture of the navicular tuberosity, which can
be treated by the following technique:
-
Make a longitudinal medial incision,
centered over the navicular tuberosity. Dissect along the line of the
incision straight down to the navicular. -
Identify the talonavicular and
naviculocuneiform joints. Owing to the curved shape of the navicular,
screws or pins placed from the medial aspect of the foot may
inadvertently transgress one or both of these joints. -
If the fracture is not comminuted,
reduction can often be achieved by inverting the foot. The navicular
tuberosity is not primarily articular, so the main concern is
restoration of the insertion of the tibialis posterior tendon and
restoring medial stability. -
Once stabilization and reduction are
achieved, insert a screw from proximal to distal using compression
technique to stabilize the fracture.
inversion and plantar flexion for 2 weeks and then reapply a splint or
cast in neutral alignment. Time to weight bearing depends on the size
of the fragment and the stability of the fixation, but most patients
can bear full weight by 6 to 8 weeks.
particularly those with severe comminution, are discussed in this
chapter under the section titled Isolated Navicular Fractures,
but in this context, it is important to note the initial aim in
treatment is to restore normal forefoot–hindfoot alignment and to
maintain the lengths of the medial and lateral columns. Many of these
patients may require later arthrodesis, which will be much easier if
the anatomy is preserved. Primary arthrodesis is occasionally indicated
(11,12,15);
however, my preference is to attempt to obtain healing in appropriate
alignment in order to maintain the function of the transverse tarsal
joints and perform arthrodesis only as a later reconstruction if
symptoms cannot be controlled with nonoperative methods.
-
Make a longitudinal lateral approach to
the anterior calcaneus, cuboid, and base of the fourth and fifth
metatarsals with variations in the exposure depending on the fracture
pattern in the cuboid and whether the anterior calcaneus is involved. -
The cuboid is generally crushed between
the calcaneus and the metatarsals. The injury may be simply to the
lateral half of the cuboid and often is primarily dorsal. Similar to
tibial plateau fractures, the articular surface
P.2991
has been driven into the body of the cuboid with a thin rim of subchondral bone preserved. -
An alternative to using an external
fixator for the previously discussed “nutcracker” fracture of the
cuboid is to use a plate spanning from the calcaneus to the fifth
metatarsal to distract and unload the cuboid fracture. Leave the plate in situ for approximately 3 months and then remove it (Fig. 111.5).![]() Figure 111.5. A: Cuboid fracture with impaction of the proximal articular surface. B: Operative radiograph showing the use of a bridging plate, threaded K-wire, and bone graft.
Figure 111.5. A: Cuboid fracture with impaction of the proximal articular surface. B: Operative radiograph showing the use of a bridging plate, threaded K-wire, and bone graft. -
Application of a plate requires elevation of the peroneal tendons and protection of the sural nerve.
-
Primary arthrodesis of the calcaneal
cuboid joint is not generally indicated, but if necessary, loss of
movement of the calcaneal cuboid joint results in about a 30% loss of
subtalar motion (8).
injuries may be due to initial misdiagnosis of the injury as a minor
sprain. The more severely displaced injuries are generally recognized
immediately. Treat late presentation of a primarily soft-tissue injury
with in-shoe devices combined with shoe modifications. Medial or
lateral column shortening combined with degenerative changes in the
affected joints is more serious and generally requires surgery.
calcaneocuboid joint and subluxation of the talonavicular joint,
lengthen the lateral column and perform an arthrodesis of the
calcaneocuboid joint.
talonavicular and naviculocuneiform joints are affected. Plan an
arthrodesis for the entire medial column from the talus to the medial
and intermediate cuneiforms. Quite commonly all three cuneiforms must
be included in the arthrodesis to form a solid block with the
navicular. There is relatively little motion between the cuneiforms,
and it is easier to get a solid fusion by involving all three. If
alignment is satisfactory, perform an in situ arthrodesis (20). If the medial column has been shortened, restoration of length is necessary and will require tricortical iliac crest graft (12).
The aim is to restore the longitudinal axis of the foot so that the
second metatarsal bisects the angle between talus and the calcaneus on
an AP radiograph of the foot. Comparison radiographs of the other foot
are helpful. Arthrodesis of the medial column is much more difficult to
achieve than for the lateral column. Good-quality bone graft is
essential, combined with rigid internal fixation, generally using
multiple screws occasionally supplemented
by a plate followed by non-weight bearing for 6 weeks and total immobilization of 3 months.
forced plantarflexion injury or a direct blow to the foot and are
essentially a dorsal midfoot sprain (7,9,11,41).
An avulsion fracture may be an indicator of a more serious fracture
dislocation. If the mechanism of injury is relatively clear, symptoms
and signs are localized at a small area on the dorsum of the foot, and
there is no tenderness over the calcaneocuboid or navicular tuberosity,
the fracture can be considered a localized injury. Check the function
of the deep peroneal nerve, which generally lies immediately adjacent
to this fracture. The tibialis anterior tendon does not insert in this
area, but isolated ruptures of the tibialis anterior do occur, so look
for this injury. Plain AP and lateral radiographs are usually
sufficient. A typical avulsion fracture has sharp edges and irregular
margins. Look for a fractured dorsal osteophyte. Do not mistake an
accessory ossicle for a fracture.
for 1 to 2 weeks. Once the acute pain and swelling have resolved, apply
a walking cast or removable orthosis (“cam-walker”) for another 3 to 4
weeks, followed by mobilization. Warn patients at the onset of
treatment that the small fragment may not heal, and that the aim of the
treatment is to allow the ligaments and soft tissues to heal. If the
bony fragment is symptomatic, particularly irritation of the deep
peroneal nerve, then surgical excision may be warranted at a later
date. It may also be useful to teach the patient how to skip-lace their
shoe.
It is important to rule out a more complex associated injury. Take a
good history to make sure the mechanism of injury is consistent with
the clinical findings. Rule out other associated injuries, particularly
to Chopart’s and Lisfranc’s joints. Assess the tibialis posterior
tendon for continuity.
navicular tuberosity, a reverse oblique will demonstrate a fracture
better than the normal medial oblique view. It is important to
differentiate between an acute fracture and an accessory navicular. An
accessory navicular usually has smooth edges rather than the sharper,
irregular margins of an acute fracture. It is possible, however, for
the fibrous syndesmosis between the accessory navicular and the
navicular body to become disrupted, and that area may be symptomatic.
An ultrasound scan may also be useful to assess the tendon at its
insertion.
nondisplaced or minimally displaced. If so, initially splint the foot
into slight inversion to take the tension off the posterior tibial
tendon and ease pain, followed by a period of 4 to 6 weeks in a
short-leg walking cast. Base the total treatment time on evidence of
clinical and radiographic union. In athletes, some recommend simple
bandaging (41). Because of the continuous pull of the tendon, nonunion may occur, but it is often asymptomatic.
especially in the adolescent, in which case, 6 weeks in a short-leg
walking cast is recommended to determine whether the syndesmosis will
heal. If the nonunion of an accessory navicular produces persistent
pain or loss of function of the tibialis posterior tendon, surgical
intervention is indicated. For displaced fractures, surgical repair is
warranted.
-
Make a medial slightly curved
longitudinal incision centered on the navicular tuberosity, curving
proximally along the posterior tibial tendon and extending
longitudinally distally along the plantar border of the medial
cuneiform. -
By blunt dissection, expose the wide
insertion of the tibialis posterior tendon with its extensive
ligamentous insertion medially and plantarward. -
For acute fractures, clean the fracture ends, reduce the fracture, and generally fix it with a single compression screw.
-
K-wire fixation may be necessary if the
fracture is comminuted and no individual fragment is large enough to
take screw fixation. If the bony fragment is small, an alternative is
to excise the fragment and repair the remaining tibialis posterior
tendon to the navicular.
foot in inversion and plantarflexion for 7 to 10 days, followed by a
short-leg non-weight-bearing cast in neutral for 4 to 6 weeks and then
a removable weight-bearing orthosis for up to 12 weeks.
frequently in the longitudinal stress pattern described by Main and
Jowett (21). Typically, vertical splits
occurring in line with the cuneiform. The pattern varies, depending on
the amount of plantar flexion the foot is in at the time of injury.
Sangeorzan (31) described three fracture patterns in 1989:
-
Type II fractures are oblique fractures
with fracture lines running dorsolateral to plantarmedial and the
forefoot is displaced medially. More extensive comminution is noted. -
Type III fractures are comminuted with the main damage being centrally or laterally and the forefoot is displaced laterally.
be helpful in distinguishing type II and type III fractures if that
influences the surgical decision making.
maintaining the length of the medial column and foot function.
Therefore, the goals of treatment are to restore an anatomic alignment
of the talar articular surface of the navicular and to restore medial
column length. Nonoperative treatment would be indicated only for an
undisplaced fracture. If the fracture is a longitudinal split, consider
a stress fracture.
injuries for comminuted type II or III fracture patterns. For type II
fractures in which there is primarily lateral comminution of the
navicular with one relatively large dorsal medial fragment, two
incisions may be indicated.
-
Make a medial incision running from the
navicular tuberosity toward the medial malleolus, above the tibialis
posterior tendon, avoiding the saphenous nerves and veins, to expose
the talar neck. The incision can be continuous, or separate incisions
can be made distally over the medial cuneiform, or depending on the
fracture pattern, the base of the first metatarsal. -
Then under direct vision, place external
fixator pins in the talar neck and medial cuneiform, apply longitudinal
traction, and tighten the external fixator while applying distracting
forces across the navicular (Fig. 111.1). If
the fracture is fixable, then either through the same medial incision
or a second dorsal lateral incision, reduce and fix the fracture. -
If the lateral fragment is too comminuted
for fixation, then reduce the dorsal medial fragment between the
cuneiforms and transfix the talus in that position with either K-wires
or fully threaded cortical screws. An alternative is to fix the
fragments only to the cuneiforms to try and preserve talonavicular
motion (11,15,31). -
For type III fractures in which the
extent of comminution is such that stable internal fixation cannot be
achieved, use the external fixator and apply longitudinal traction. By
direct pressure, attempt to manipulate the fragments into satisfactory
alignment, particularly aiming to align the forefoot to the hindfoot
and maintain the medial column length. -
When there is widespread comminution of
the fracture, do not expose it because it simply devascularizes the
fracture fragments and may predispose the patient to avascular
necrosis. Percutaneous fixation may add to the stability.
in the displaced type I and type II and some type III fractures. With
comminuted type II and III fractures, open reduction and stable
internal fixation are difficult to achieve and may need to be combined
with some form of external fixation.
-
Make a dorsomedial longitudinal incision
through the tibialis anterior tendon sheath, down through the inferior
margin of the sheath, and onto the navicular, being careful to identify
the talonavicular joint and the medial cuneiform. -
Retract the tendon either medially or laterally to better visualize the fracture.
-
Reduce the fracture and, if possible, fix
it with screws inserted dorsally. It is important to remember the curve
of the navicular and identify the joints on either side to avoid the
screw impinging on either joint.
non-weight bearing for at least 6 to 8 weeks and occasionally for 12
weeks. Patients, particularly those with type II and III fracture
patterns, should be advised that there is a high likelihood of a fair
to poor outcome (9,10,11 and 12,15,21,27,31)
due to degenerative changes, malunion, nonunion, or avascular necrosis,
and that even with good fracture healing, stiffness is a likely outcome.
primarily for degenerative arthritis of the talonavicular joint due to
avascular necrosis or shortening of the medial longitudinal arch
causing dysfunction of the forefoot. The primary reconstruction option
for all of these problems is arthrodesis, extending from the talar neck
into the cuneiforms. If alignment is satisfactory, an in situ arthrodesis can be performed. Two techniques are described for this.
-
Expose the involved joints through a longitudinal medial incision.
-
In the first technique, create a
longitudinal channel in the bones and joints to be fused. Take iliac
crest graft, split it, and reverse it so that the cancellous surfaces
face out. Place them in the channel in the talar neck, navicular, and
into the cuneiforms. Fix with either screws or K-wires.
lengthening is required, then the second technique is preferred because
the tricortical iliac crest struts are strong enough to lengthen the
medial column. Both of these techniques are described in the article by
Ferris et al. (12).
cuboid injuries are associated with either Chopart’s joint fracture
dislocations or as part of a Lisfranc injury. Both of these injuries
produce a “nutcracker” type of fracture (17),
as described in the previous section. Isolated fractures can occur with
a direct blow; these fractures are generally minimally displaced and
can be treated in a short-leg cast. As long as the plantar and medical
cortices are intact, a walking cast used for approximately 6 weeks is
sufficient. Other isolated cuboid fractures are some of the minor
avulsions seen with inversion or plantarflexion injuries (7).
These fractures generally can be treated symptomatically. It is
important to be aware of the os peroneum because it can be mistaken for
a fracture of the cuboid. The os peroneum is a sesamoid bone in the
peroneus longus tendon as it curves around the cuboid. It can be
painful.
a source of pain in the lateral foot that is not usually due to acute
trauma but is seen primarily in athletes and dancers (23).
commonly an avulsion fracture due to plantar flexion force or from a
direct blow. The most severe isolated cuneiform fractures are from
direct trauma, particularly from gunshot wounds or propellers (26),
which produce open fractures with bone loss. Otherwise, any injury to
the cuneiform needs to be a warning sign to look for injury to the
Lisfranc complex in particular. Note that Lisfranc’s variants can
extend to the intercuneiform joints (3,11,25). Isolated dislocations of the cuneiforms have been described (9,11). Charcot’s arthropathy can result in isolated injuries as well.
foot. If there is suspicion of a Lisfranc injury, a CT scan may
identify the small plantar fractures associated with disruption of the
strong plantar ligaments. Manipulation of the foot under anesthesia may
be necessary to detect instability.
of the fracture. Treat isolated dorsal avulsion fractures with initial
splinting, followed by a walking cast or a removable cast boot. Treat
fractures of the body of the cuneiform non-weight bearing for at least
6 weeks and longer if severe comminution delayed healing, or undetected
ligament injury (9,15). Treat open fractures as described in Chapter 12 and use external fixation if necessary to stabilize the foot (26).
If bone loss has occurred, then late arthrodesis and bone grafting may
be required. Even some apparently minor injuries may eventually require
arthrodesis to treat a painful joint (12).
The frequency of this injury is increasing owing to motor vehicle
injuries and falls secondary to sports and work activities. Although it
was thought to be a rare injury, this was because the injury is
difficult to diagnose. Injuries that were previously undetected are now
being recognized. Still today, approximately 20% of these injuries are
undiagnosed at initial presentation, particularly in the polytrauma
patient (13,39).
Variants of the Lisfranc injury involving the cuneiforms has increased
so that now the term “Lisfranc’s complex” rather than “Lisfranc’s
joint” is more appropriate. Lisfranc’s fracture-dislocations can
include the tarsometatarsal (TMT) joints, cuneiforms, cuboid, and
occasionally even the navicular.
injuries, management of the soft tissues may be the most challenging
aspect of treatment. Indirect trauma is more common. Generally, a
longitudinal or axial load is applied to a plantarflexed foot such as
in a football player being tackled, or from windsurfing and
snowboarding. More severe injuries result from the high-energy forces
of motor vehicle or motorcycle accidents (39).
The base of the second metatarsal is the “keystone” of the Lisfranc
complex, being inset so that the medial and lateral cuneiform bones
provide support on either side of the base of the second metatarsal,
locking it in place. The other four metatarsals have relatively little
bony support. It is also important to understand that the dorsal TMT
ligaments and capsule are relatively weak compared to the strong
plantar ligaments. The Lisfranc ligament itself is a strong oblique
ligament from the lateral aspect of the medial cuneiform to the base of
the second metatarsal (33). Anatomically and radiographically, Stein (36) described five features that are radiographic constants and are helpful in assessing this area.
-
The intermetatarsal space between the
third and fourth metatarsals is continuous with that between the
lateral cuneiform and the cuboid. -
On the medial oblique view, the
intermetatarsal space between the second and third metatarsals is a
continuous straight line with the open space between the lateral and
medial cuneiform. -
On the AP view, the medial border of the
second metatarsal forms an unbroken line with the medial border of the
middle cuneiform. -
On the AP view, the space between the first and second metatarsals matches that between the medial and intermediate cuneiforms.
-
On a lateral view, the base of the metatarsals should not be more dorsal than the adjacent cuneiform or cuboid (Fig. 111.6 and Fig. 111.7).
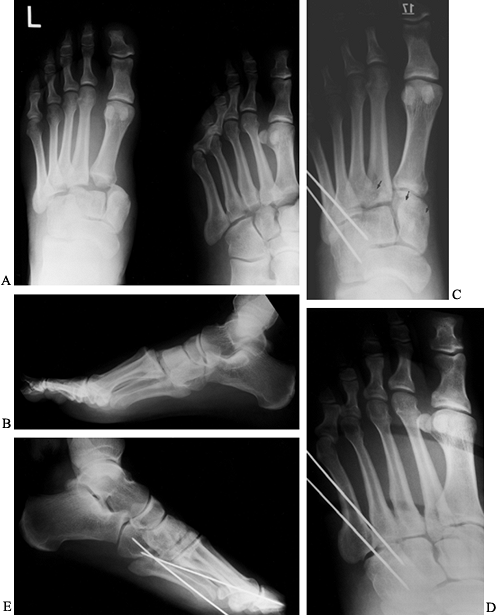 Figure 111.6. Lisfranc’s dislocations with predominantly ligamentous injuries. A: AP views. B: lateral view. C:
Figure 111.6. Lisfranc’s dislocations with predominantly ligamentous injuries. A: AP views. B: lateral view. C:
Postoperatively on this AP view, two absorbable screws stabilize the
medial column and two K-wires stabilize the lateral column. Arrows show
the path of the screws from the medial cuneiform to the second and
third metatarsals, which cannot be seen because they are radiolucent. D: Oblique view. E: lateral view.![]() Figure 111.7. AP (A), oblique (B), and lateral (C)
Figure 111.7. AP (A), oblique (B), and lateral (C)
radiographs of bony Lisfranc’s injury, fracture of second and third
metatarsal necks, and displaced sesamoids due to a partly reduced first
MTP dislocation. AP (D) and lateral (E)
postoperative radiographs showing stainless steel screws to stabilize
Lisfranc injury. The first MTP joint was reduced and stabilized with a
K-wire. The second and third metatarsal neck fractures are well aligned.
examination because this injury may be missed, particularly in someone
complaining of an “ankle sprain.” A history that suggests forced
plantarflexion of the foot with axial loading needs to be examined very
carefully. If there is tenderness dorsally over the TMT joints and it
is not clear whether this is superficial or deep, then stress the
Lisfranc complex by grasping the appropriate metatarsal head and
applying plantarflexion and dorsiflexion forces to the metatarsal, with
the hindfoot stabilized. Pain indicates TMT joint pathology. Similarly,
rotational or mediolateral forces applied to the forefoot producing
pain in the midfoot suggests injury to the Lisfranc complex. Take AP,
lateral, and medial oblique radiographic views. In addition to the key
features listed earlier, other significant signs include
-
A small fracture from the base of the second metatarsal or intermediate cuneiform.
-
Compression fracture of the cuboid on the AP or oblique radiograph (17).
-
Any indication of overlap between the metatarsal bases and the adjacent tarsal bones, suggesting complete dislocation.
circumstance but can be obtained under either general anesthesia or
occasionally with an ankle block or local anesthetic directly
infiltrated into the TMT joints, depending on the clinical situation. A
CT scan is not usually necessary to make the diagnosis, but if there
are comminuted fractures, particularly of the cuboid, it may assist in
assessing the fracture pattern.
Lisfranc’s injuries can be associated with fractures of the shafts or
necks of the metatarsals or dislocation of the MTP joints. Longitudinal
forces can produce more proximal injuries, including navicular
fracture. It is always important to visualize the entire foot
radiographically in a patient with polytrauma with a swollen foot
because an obvious fracture such as a calcaneus or ankle fracture may
lead to missing a more subtle injury in the midfoot or forefoot (Fig. 111.8).
 |
|
Figure 111.8.
Patient referred with persistent lateral foot pain 18 months after a calcaneal fracture and subtalar arthrodesis. There was a missed dislocation of tarsometatarsals 4 and 5. A: Lateral view of the hindfoot; note that the cuboid is plantar flexed. B: Oblique view showing overlap of the bases of the fourth and fifth metatarsals and the cuboid. C,D: CT scan sections through the midfoot, demonstrating chronic dislocations. |
fractures in the literature. At present the most frequently quoted are
Hardcastle et al. (16) and Myerson et al. (24,25).
These classifications are primarily descriptive and do not alter
treatment decisions. Myerson’s work added to the understanding of the
injury and led to the concept of the Lisfranc joint complex.
is from the “midfoot sprain” to severe displaced fracture-dislocation,
occasionally with overlying soft-tissue injuries. In the polytrauma
patient, the more subtle forms may be missed; therefore, clinical
suspicion is important. See Figure 111.2 for an assessment algorithm.
there is significant plantar or dorsal displacement of the metatarsal
bases, neurovascular compromise is a possibility and urgent closed
reduction should be attempted. Compartment syndrome is also possible
with this injury, and fasciotomy is occasionally required. If
fasciotomy is required, the incisions for the fasciotomy should be
planned based on the incisions necessary for open reduction and
internal fixation of the underlying injury. Other aspects of immediate
treatment include assessing the rest of the foot for any associated
injuries, particularly the MTP joints. If the major displacement cannot
be reduced immediately, whether by direct manipulation or by
application of toe traps and ankle traction, then perform immediate
open reduction and internal fixation. This approach will decrease
pressure on the skin and tension on the neurovascular bundle.
Associated swelling is unlikely to resolve in the presence of
persistent displacement.
injuries who are not medically stable for immediate intervention,
splinting, ice, and elevation are appropriate in the interim. Once the
injury has been diagnosed and the patient otherwise stabilized, the
choices for a displaced Lisfranc’s fracture-dislocation are either
closed reduction and percutaneous fixation or open reduction and
internal fixation.
injury to the Lisfranc complex with no demonstrable displacement or
fracture on plain x-ray studies, further investigation is warranted
because a purely ligamentous injury may appear to be anatomic on plain
x-ray studies and yet be unstable. Stress views or examination under
anesthesia,
or both, may demonstrate instability. If that is not possible, then
splint the foot and do not allow the patient to bear weight for a few
days until the foot can be reassessed clinically and radiographically.
One method of obtaining a stress view in a patient who presents late
(i.e., 2 weeks or more after injury) is to perform a weight-bearing
x-ray and compare it with the opposite side, particularly looking at
the gap between the first and second metatarsals and the medial and
intermediate cuneiforms.
essential in Lisfranc’s injuries, even though the results are still
disappointing (3,4,9,11,13,15,16,24,25,28).
In the majority of cases in which significant displacement is visible
on initial radiographs or intraarticular fractures exist, closed
reduction is not sufficient. Closed reduction is feasible for subtle
injuries that are detected only on stress views. Commonly, this is seen
as a gap between the medial ray (first metatarsal and medial cuneiform)
and the second ray. Closed reduction and percutaneous, cannulated screw
fixation are an option.
-
Use a large bone tenaculum, such as a
pelvic reduction clamp placed through two small stab wounds to compress
the medial cuneiform to the base of the second metatarsal under
radiograph control.
and, therefore, generally are not suitable if they need to be left in
place for longer than 6 weeks. They are frequently used for the lateral
TMT joints in an effort to avoid stiffness.
the guide pins are of small diameter and prone to shear off, leaving a
portion in situ. Therefore, if you are
using cannulated screws, it is safer to stabilize the construct with a
parallel K-wire of at least 1.6 mm diameter so that when the screw hole
is drilled and tapped, there is no micromotion between the bones. Guide
pins can still break. An alternative when fluoroscopy is available is
to use the drill bit for initial fixation; having stabilized the
construct with a tenaculum, check the position under fluoroscopic
control, and then insert a 3.5 mm cortical screw.
therefore, provided adequate reduction has been achieved, com pression
is not necessary. A more recent option is that of bioabsorbable screws,
which can be inserted in a similar fashion (Fig. 111.6).
-
Position the image until it is
perpendicular to the plane of the intercuneiform and intermetatarsal
joint because that view is necessary to assess the reduction. Achieve
an anatomic reduction. -
Then insert a screw from the medial
cuneiform into the second metatarsal base, generally starting from
plantar medial going to dorsal lateral. If the third metatarsal is also
involved in the injury, then this screw can also fix the third
metatarsal shaft. If the fourth and fifth metatarsal joints are not
involved, then that single screw may be sufficient to stabilize the
medial column. If in doubt, insert a second screw from the first
metatarsal base into the second cuneiform to supplement the fixation.
There are multiple options for internal fixation, depending on the
pattern of injury (9,11,15).
in which significant displacement or articular fractures are evident on
initial films. The majority of authors support this approach, although
the choice of technique varies (3,4,9,11,13,15,16,24,25,28).
the surgical incisions. A C-arm fluoroscope is useful. Before prepping
the foot but after induction of anesthesia reassess the stability of
each column of the foot under fluoroscopy. If the fourth and fifth
tarsal metatarsal joints are stable to fluoroscopy, then an incision
over these joints may be avoided. Much less commonly, the injury is
isolated to the lateral TMT joints, sparing a medial incision. A
variety of surgical approaches have been used (3,4,9,11,15,24,25).
A frequent choice is a dorsal longitudinal incision just lateral to the
extensor hallucis longus, extending to the first metatarsal space. Many
authors supplement this incision with a second parallel incision
extending from the third web space proximalward between the lateral
cuneiform and the cuboid.
to use any combination of the following three incisions as the fracture
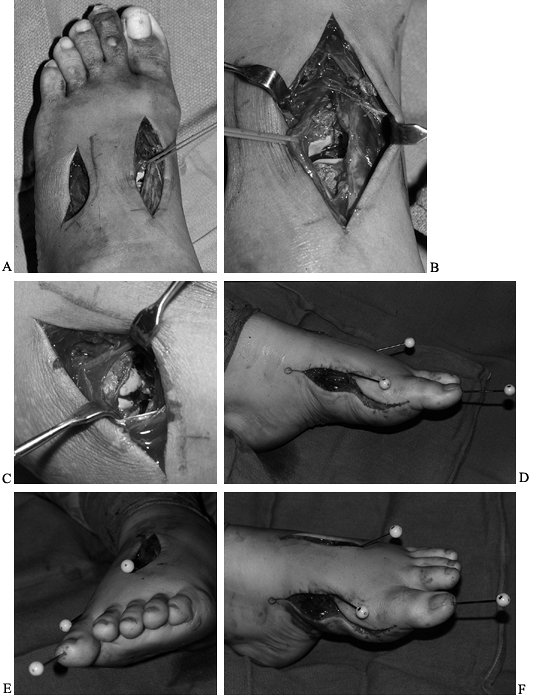
pattern dictates (12) (Fig. 111.9D, Fig. 111.9E and Fig. 111.9F).
 |
|
Figure 111.9. A: I prefer two dorsal incisions for Lisfranc complex injuries. Vessel loops are around the neurovascular bundle. B: The neurovascular bundle is retracted laterally to demonstrate the base of the second metatarsal and intermediate cuneiform. C: The bases of the fourth and fifth metatarsals are dislocated dorsally. D, E, F: Medial and dorsal surgical incisions with an extended medial exposure and provisional fixation with K-wires.
|
-
Make the first incision medially from the
navicular tuberosity centered along the midportion of the medial
cuneiform to the midpoint of the first metatarsal. Dissect down to
bone, lifting an osteoperiosteal flap and being careful not to detach
the tibialis anterior tendon insertion that wraps around the medial
aspect of the medial cuneiform and first metatarsal base, which can, on
occasion, be trapped in the fracture fragments. -
Make the second incision over the lateral
aspect of the second metatarsal shaft and second interspace. Also carry
this incision down to the bone, avoiding the medial branch of the
superficial peroneal nerve. -
Once these two incisions are down to
bone, then dissection allows elevation of a flap that contains the
doralis pedis neurovascular bundle. Take particular care to protect the
dorsalis pedis artery because it penetrates the first intermetatarsal
space. -
Between these two incisions, identify and
reduce the first and second TMT joints and, in particular, reduce the
base of the second metatarsal to the lateral aspect of the medial
cuneiform (Fig. 111.9D, Fig. 111.9E and Fig. 111.9F).
The rationale behind the medial incision is to check the rotational
reduction of the first metatarsal and to place screws from the medial
aspect of the foot into the metatarsal bases and cuneiform. -
If necessary, place a K-wire from the
dorsal incision to stabilize the fracture and then place a screw
medially. The key screw is from the plantar medial aspect of the medial
cuneiform to the base of the second metatarsal.
intra-articular fracture (e.g., the corner fracture of the medial
aspect of the second metatarsal), the purpose of the screw is not to
transfix that fracture but to stabilize the majority of the second
metatarsal in appropriate alignment. An alternative fracture pattern,
when there is a transverse fracture of the second metatarsal, leaves
the base intact. Obviously, there are a wide variety of fracture
patterns that can occur in the metatarsal, but these two are commonly
seen.
-
In the latter case, fix the screws into
the base of the second metatarsal and a longitudinal K-wire can
stabilize the shaft of the metatarsal to the base. -
When the second metatarsal shaft is extremely comminuted, a longitudinal K-wire to maintain the alignment is appropriate.
-
If the articular surface is comminuted,
remove any small fragments, particularly those without a blood supply.
If there remain any articular fragments too small for a screw, then use
a smooth or threaded K-wire for fixation. -
In some circumstances, it is possible to
stabilize the second ray by placing screws on either side (i.e., the
first and third rays). Occasionally, supplementary screws are needed
from the medial cuneiform into the intermediate or through into the
lateral cuneiform.
curve the third incision to match to the steep angle of the fourth and
fifth TMT joints (Fig. 111.9).
-
Start distally in the fourth interspace
and curve laterally and inferiorly proximalward to allow adequate
exposure of the fourth and fifth TMT joints. -
For fixation across this joint, make a
separate small stab wound over the base of the fifth metatarsal just
distal to the flare. Again, there is a choice of K-wire or screw
fixation in this area. More recently, there has been a move away from
using screws across the fourth and fifth TMT joint because stiffness of
these joints is more problematic. Therefore, insert a 0.062 in. (1.6
mm) threaded K-wire because it provides adequate stability with less
damage to the articular surface than a 3.5 mm screw. This can be cut
off to lie just under the skin. It generally is easily palpated and
removed in clinic through a stab incision under local anesthetic at 3
months’ follow-up. Document the fact that the K-wire is threaded so
that needle-nose pliers or heavy-duty needle holders used to unscrew it. -
Make the two or three incisions to expose the area adequately (Fig. 111.7 and Fig. 111.9). Reduce the fracture dislocations working through the multiple exposures, and obtain temporary fixation with K-wires.
-
Check the alignment with radiographs or
fluoroscopy before placing any permanent fixation. Often, it is not
possible to reduce each portion of the injury accurately until all of
the joints have been approximately aligned. -
If the MTP joints are dislocated, it may
be necessary to reduce the MTP joint before the metatarsal base can be
anatomically relocated (Fig. 111.7). When
metatarsal neck fractures have occurred they usually do not prevent
reduction of the metatarsal base, but it is possible to extend the
dorsal incisions distally to expose the metatarsal necks and transfix
these fractures with longitudinal K-wires. -
Once all the fractures or dislocations
are adequately reduced and stabilized, insert permanent fixation. My
preference is fully threaded cortical screws, preferably not
cannulated. Screws can be stainless steel, titanium, or bioresorbable.
When screws are not possible because of comminution, then use either
smooth or threaded K-wires (Fig. 111.6 and Fig. 111.7).
Smooth K-wires are often satisfactory when stabilizing fractures with
minimal ligamentous injury because generally by 6 weeks, fractures
consolidate sufficiently to remove the K-wire. -
The pattern of screw fixation varies
depending on the injury pattern. In particular, the injury may extend
proximally between the cuneiforms or into the navicular, in which case
transverse screws may be necessary to stabilize these injuries. The
lateral cuboid may impact on the articular surface, particularly the
dorsal lateral corner. If this is 25% or less of the articular surface,
it is generally possible to stabilize the fourth metatarsal base to the
medial half of the cuboid and insert a screw from the base of the fifth
into the fourth metatarsal to stabilize the construct further. In this
way, the articular surface of the cuboid can then be reduced, and
occasionally bone grafted and fixed with a pin, a bridging plate, or an
external fixator if the cuboid has a nutcracker-type injury that needs
to be held out to length (Fig. 111.5).
splinting for 7 to 10 days and then the application of a
non-weight-bearing cast. At approximately 6 weeks, remove any K-wires
that have been left out through the skin for either a metatarsal neck
or shaft fractures. Provided that the patient is reliable and will
remain non-weight bearing, it is reasonable to place the patient in a
removable cast to start range of movement to the ankle and subtalar
joints. At 3 months, if clinical and radiographic findings show
maintenance of the reduction and healing, the patient may commence
weight bearing in a cam-walker. Schedule surgery for removal of the
screws 3 to 4 weeks later. Whether removal of all of these screws is
necessary is under review, but certainly any screw or hardware across
the fourth and fifth TMT joints must be removed. I prefer to remove any
screws that cross a joint. Some authors advocate leaving the screws in
the medial three columns or even performing a primary arthrodesis (11,14,15,32). The use of bioresorbable implants eliminates the need for a second procedure.
significant displacement, then perform an open reduction and internal
fixation as in an acute fracture. If the injury is between 6 weeks to 6
months old, base your decision of which procedure to perform on the
patient’s age and general health, the severity of displacement,
activity level, and whether it is purely a soft-tissue or bony injury.
In some cases, repair as for an acute injury may be successful. After 6
months, acute repair is unlikely to be successful, and the choices are
nonoperative treatment or reduction and arthrodesis (11,12,15,32). Realignment and arthrodesis may lead to development of degenerative changes in adjacent joints (12).
The presence of diabetes and, particularly, diabetic neuropathy makes
success of any surgery less likely. Advise the patient that late
treatment of a Lisfranc injury likely will result in long-term problems
with persistent pain and possible progression of deformity.
-
Fractures of the tuberosity, often associated with inversion ankle injuries
-
Jones’ fracture, which is a transverse fracture of the diaphysealmetaphyseal junction
-
Spiral fractures of the shaft associated with rotational foot injuries
-
Oblique or transverse fractures of the metatarsal neck
site of the fracture in the metatarsal, especially whether the
metatarsal is one of the middle metatarsals, which behave differently
than the first and fifth. Similarly, multiple metatarsal fractures are
treated differently than an isolated metatarsal fracture. Apart from
Jones’ fracture, there has not been much scientific study of metatarsal
fractures, and authors have varied significantly in recommendations
about management. A variety of opinions exist on the indications for
reduction and internal fixation of these fractures (9,15,34,38).
does require special consideration. Any shortening of the first
metatarsal or plantar or dorsal displacement of the metatarsal head
will have an adverse affect on foot function as a whole. In addition,
any articular fracture causing loss of movement in the first MTP joint
will interfere with the normal progression of gait. Therefore, any
displaced fracture of the first metatarsal that allows shortening or
angular displacement or impacts the MTP joint requires reduction,
either closed or open, and fixation. The choice between closed
reduction and K-wire or external fixation versus open reduction and
internal fixation depends on the site and comminution of the fracture
and possibly related soft-tissue injuries.
metatarsal injuries), particularly those associated with inversion
injuries. Jones’ fracture, although less common, is of clinical and
academic interest because of its poor prognosis. The fifth metatarsal
is the most mobile of the five, so a small amount of shortening or
angular deformity may be less problematic because the fifth metatarsal
itself is more adaptable.
surgery are the fracture of the tuberosity of the fifth metatarsal,
which is commonly an avulsion fracture, and the spiral fracture of the
fifth metatarsal shaft. Nonoperative treatment of metatarsal fractures,
include using a stiff-soled shoe, strapping, or a short-leg
non-weight-bearing cast for 4 to 6 weeks.
metatarsal like an ankle sprain. Spiral fractures of the fifth
metatarsal shaft produce significant pain and swelling, and benefit by
a few days of rest, elevation, splinting, and crutches. Once the acute
pain and swelling have subsided in both of these injuries, a removable
cast device, preferably with some means to control swelling, will
enable the
patient
to walk relatively pain free. A hard-sole shoe does not give sufficient
support for the ankle and is moderately uncomfortable for walking.
In brief, such fractures of the fifth metatarsal have a propensity for
nonunion. For low-demand patients, if seen immediately after the
injury, treat non-weight bearing for 6 weeks in a short-leg cast.
Immobilization may be needed for 3 months or more with still no
guarantee that the fracture will unite. For those patients with an
established nonunion or those who are considered high demand,
particularly athletes, it is recommended to peform intramedullary
fixation of the fifth metatarsal shaft (9,15,34,38).
In the acute instance, internal fixation alone may be sufficient. In
established nonunions, opening the fracture site, debridement of the
sclerotic bone, and bone grafting combined with internal fixation are
warranted.
lower violence, and if the transverse metatarsal ligament is intact,
most often there is minimal displacement and closed management is
indicated. However, this is one area where authors differ widely.
Shereff (34) believes that any displacement of
more than 3 to 4 mm or more than 10° of angulation requires open
reduction and internal fixation.
level of energy has been dissipated in the foot. More than likely, the
ligaments are disrupted and significant shortening or displacement will
occur. These metatarsal fractures are often associated with other
injuries in the foot and, as previously noted, the amount of morbidity
associated with the metatarsal fractures has been underestimated.
Dorsal displacement of the metatarsal head or shortening produces
transfer metatarsalgia, which can lead to significant disability (Fig. 111.10).
It is less clear cut whether medial or lateral displacement will cause
interference with the adjacent metatarsal or interdigital nerve (34),
although anatomically it is certainly feasible. If palpation of the
forefoot demonstrates enough displacement of the affected metatarsal
head to alter the mechanics of weight bearing, then reduction and
fixation are indicated. Closed reduction of a metatarsal without some
form of fixation is unlikely to be stable (15,34).
 |
|
Figure 111.10. Patient with persistent metatarsalgia after a “neuroma” was excised. AP (A), oblique (B), and sesamoid (C)
views show healed metatarsal fractures. The fifth metatarsal is asymptomatic; pain is due to the overload of the third metatarsal from the dorsally angulated second metatarsal. |
and internal fixation. Fractures of the first metatarsal may require
fixation with screws or a plate and screws.
fractures rarely results in anatomical position therefore I favor open
reduction.
-
Expose a fracture of the metatarsal neck
through a 2 to 3 cm longitudinal dorsal incision. For multiple neck
fractures, a somewhat larger incision over the first and third or
second and fourth web spaces, depending on which metatarsals are
fractured, provides adequate exposure. Identify and protect the
extensor tendons and neurovascular structures. -
Expose the fracture and insert a 1.6 mm
or 2 mm K-wire into the medullary canal of the distal fragment and exit
on the plantar aspect of the foot. Keep the toe dorsiflexed to avoid
penetration of the proximal phalanx. -
Then attach the drill to the exposed
K-wire outside of the foot, reduce the fracture anatomically, and drill
the wire retrograde into the medullary canal of the proximal shaft
securing the fracture. Verify proper position radiographically. -
Cut the K-wire to leave 1 to 1.5 cm exposed and apply pin caps or bend the end of the wire to prevent migration.
a splint. K-wires can be removed at 4 to 6 weeks, and weight bearing is
then permitted. Sometimes, a cam-walker is useful for a couple of weeks.
hyperextension and is an extreme example of the “turf toe” type injury.
It can also occur with severe direct trauma, such as in motor-vehicle
accidents. Jahss (19) classifies the injury as
type I or II, depending on whether the intersesamoid ligaments are
intact or whether one of the sesamoids has a transverse fracture. In
the type I dislocation, the ligament and sesamoid are intact, and if
the lesion is irreducible by closed means, it will require an open
reduction and sometimes K-wire fixation. In the type II injury, there
is either disruption of the intersesamoid ligament or a transverse
fracture of one of the sesamoids. Closed reduction is usually
successful, but when the sesamoid is fractured, the distal fragment
usually requires excision. These are uncommon injuries. These can be
approached dorsally, medially, or through a plantar incision. My
preference is a direct medial approach, which allows access to both the
dorsal and plantar aspects of the joint which avoids the neurovascular
structures and a plantar scar (19).
Be sure to preserve the continuity of the flexor hallucis brevis tendon
if partial or complete excision of the sesamoid is indicated.
in children. The most common mechanism is a hyperextension injury. The
toe usually sits in a hyperextended position at the MTP joint with some
associated clawing, the metatarsal head having button holed through the
plantar plate. Closed reduction is often possible, but direct traction
on the toe may further trap the metatarsal head and be ineffective. If
closed reduction is ineffective, perform open reduction through a
dorsal incision adjacent to the extensor tendon. These dislocations are
usually stable after reduction. Chronic dislocations generally require
open reduction and K-wire fixation through a dorsal approach.
Sometimes, a metatarsal condylectomy is necessary to achieve reduction.
symptomatic. Although acute fractures of the sesamoids may occur with
either direct trauma or hyperextension, it is also possible to have
stress fractures of the sesamoids, symptomatic bipartite sesamoids, and
also avascular necrosis of the sesamoids (7,9,15,19,41). Clinical and radiographic
differentiation of these conditions may not be clear cut. A bone scan
is not likely to differentiate between a stress fracture, an acute
fracture, avascular necrosis, or even sesamoiditis. A bipartite
sesamoid generally does not appear hot on a bone scan.
includes no weight bearing and immobilization of the MTP joint for at
least 4 to 6 weeks. This is followed by a further period of at least 4
to 6 weeks with protected weight bearing by relief padding or a
removable cast-brace for a total of 3 months immobilization. Lack of
healing is generally treated by sesamoidectomy. Occasionally, if one
fragment is small, excision of a single pole is possible. The
application of a bone graft to an undisplaced fracture site may
encourage union.
phalanx of the great toe, generally treat phalangeal fractures by
strapping to the adjacent toe and using a stiff-soled shoe until pain
and swelling settles. Similarly, generally treat dislocations of the
interphalangeal joint, when closed, by closed reduction, strapping to
an adjacent stable toe, and stiff-soled shoes (Fig. 111.11).
 |
|
Figure 111.11.
Residual displacement after closed reduction of interphalangeal dislocation of the great toe. The patient declined further surgery. |
function and the size of the bones that makes them more suitable for
internal fixation, displaced intra-articular fractures are generally
treated with open reduction and internal fixation with miniscrews.
Treat shaft fractures of the proximal phalanx with a longitudinal
K-wire, screws, or a miniplate if closed reduction and a splint or cast
does not give adequate alignment and stability.
and irrigate the wound, stabilize the fracture with an intramedullary
K-wire running lengthwise down the toe to maintain length and medial
and lateral stability, and give antibiotics. Interphalangeal joint
dislocations are often open on the plantar aspect and, once they are
reduced, are usually stable.
viability of the toe must be assessed in terms of neurovascular damage
and the degloving component of the injury (26).
Salvage of the toe risks infection, and poor function must be compared
with the effects of loss of the toe through amputation on foot function.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
PH, Reschauer R, Kutscha-Lissberg E, Schoffmann W. Injuries to the
Tarsometatarsal Joint: Incidence, Classification and Treatment. J Bone Joint Surg 1982;64B:349.
MS, Fisher RT, Burgess AR, et al. Fracture Dislocations of the
Tarsometatarsal Joints: End Results Correlated with Pathology and
Treatment. Foot Ankle 1986;6:225.
M, Margulies JY, Barbarawi M, et al. Fractures of the Body of the
Tarsal Navicular Bone: Case Reports and Literature Review. J Trauma 1989;29:1448
JS, Balduini FC, Zelco RR, et al. Fractures of the Base of the Fifth
Metatarsal Distal to the Tuberosity: Classification and Guidelines for
Nonsurgical and Surgical Management. J Bone Joint Surg 1984;66A:209.
D, Schemitsch E, Waddell J. The Outcome of Foot Injuries in Multiple
Injured Patients. (Abstract.) American Orthopaedic Foot and Ankle
Society 1998 Annual Winter Meeting.


