Femoral Neck Fractures: Open Reduction Internal Fixation
fixation (ORIF) of a femoral neck fracture is a displaced fracture that
is not satisfactorily reduced using closed means. It can be done in a
patient of any age who has adequate bone density. Garden’s radiographic
index for acceptable reduction is useful in determining the need for
ORIF (1). On the anteroposterior (AP) view, the
angle between the central axis of the medial trabeculae of the head and
the medial cortex of the proximal femoral shaft should be maintained.
It should measure between 180 degrees and 160 degrees. Values more than
180 degrees and less than 160 degrees indicate unacceptable valgus and
varus alignment, respectively. On the lateral view, the alignment index
should be within 20 degrees of the normal 180-degree value. According
to this index, fractures that are not satisfactorily reduced by closed
means have been shown to be at greater risk for avascular necrosis and
osteoarthrosis and are therefore best treated with ORIF.
limited anterior capsulotomy results in evacuation of the fracture
hematoma, thus decreasing intracapsular pressure. This will improve
circulation to the femoral head, thereby decreasing the possibility of
osteonecrosis (2). Because no significant blood
supply is carried to the femoral head from the anterior capsule, an
anterior approach to the femoral neck causes no additional harm to the
circulation of the femoral head (3). Second,
open reduction allows direct visualization of the fracture site,
thereby facilitating optimal fracture reduction prior to fixation. The
accuracy of reduction and the density of the femoral head and neck have
been shown to be the two most important factors in achieving stability
after internal fixation of a femoral neck fracture. Even fractures that
appear reasonably well reduced under fluoroscopy can be markedly
displaced upon direct visualization, particularly in rotation.
ischemic, internal fixation should be considered a relative orthopedic
emergency (2). Attempts to perform the surgery
within 8 hours in the highest risk groups (patients younger than 50 years, including children) have improved outcomes (2,4).
fracture include advanced rheumatoid arthritis or moderate
osteoarthritis of the adjacent hip joint, poor bone density, limited
life expectancy, pathologic fractures related to metastatic disease,
and the presence of severe psychiatric disease. These patients are
better treated by arthroplasty.
pre-injury functional assessment, are vital in preoperative evaluation.
It should be determined whether a high-energy or low-energy force
caused the injury. Femoral neck fractures are typically the result of a
low-energy mechanism in elderly patients, whereas high-energy forces
are often the cause in younger individuals. Multiply injured patients
must be rapidly evaluated and cleared in terms of abdominal, chest, or
head injury.
function, or both directs the surgeon towards arthroplasty. Patients
with major medical co-morbidities benefit from treatment of their
associated medical condition up to 48 hours before surgery (5).
Elderly and sick patients often benefit from arthroplasty. It is also
important to determine the preoperative level of function. A previous
history of significant hip pain, which may point to a possible
preexisting arthrosis in the hip joint, should make the surgeon lean
toward arthroplasty.
femoral neck fracture should be prioritized over most other closed
injuries. Approximately 3% to 5% of patients with diaphyseal fractures
of the femoral shaft will have a concomitant femoral-neck fracture (2). High-quality hip and knee radiographs should be taken in all patients with diaphyseal fractures of the femur.
amount of deformity and presence or absence of any neurovascular
deficits. Range of motion is typically painful and should not be
performed. Associated injuries should be ruled out. It is usually
sufficient to immobilize the limb using pillows under the knees, as
traction has not been shown to provide any significant benefit. In
fact, traction tightens the anterior capsule, resulting in an increase
in intracapsular pressures that may further compromise the femoral head
circulation (6).
patients who are deemed candidates for surgery. Specifically,
assessment of bone density using Singh’s index is useful for purposes
of patient selection (7). Standard radiographic
examination of femoral neck fractures should consist of an AP and
cross-table lateral radiograph. An additional pelvis AP view aids in
evaluation of bone density, defines the neck shaft angle, and provides
a comparison to the uninjured hip. This is particularly useful in cases
where there is extensive comminution of the femoral neck.
useful in further delineating the amount of comminution of the fracture
and the degree of displacement of the fragments. Furthermore, in
multiply injured patients, CTs have often been obtained for purposes of
evaluation of the abdomen and pelvis and should be reviewed in advance
of stabilization of the fracture. Bone scans and magnetic resonance
imaging (MRI) have not been reliable in determining viability of the
femoral head and in identifying those who will develop posttraumatic
osteonecrosis, and are therefore not useful, in the short-term, in
selecting patients for either ORIF or arthroplasty (8,9).
Spinal and epidural anesthesia are the best choices for older patients
with medical problems. Patients may be positioned with the extremity
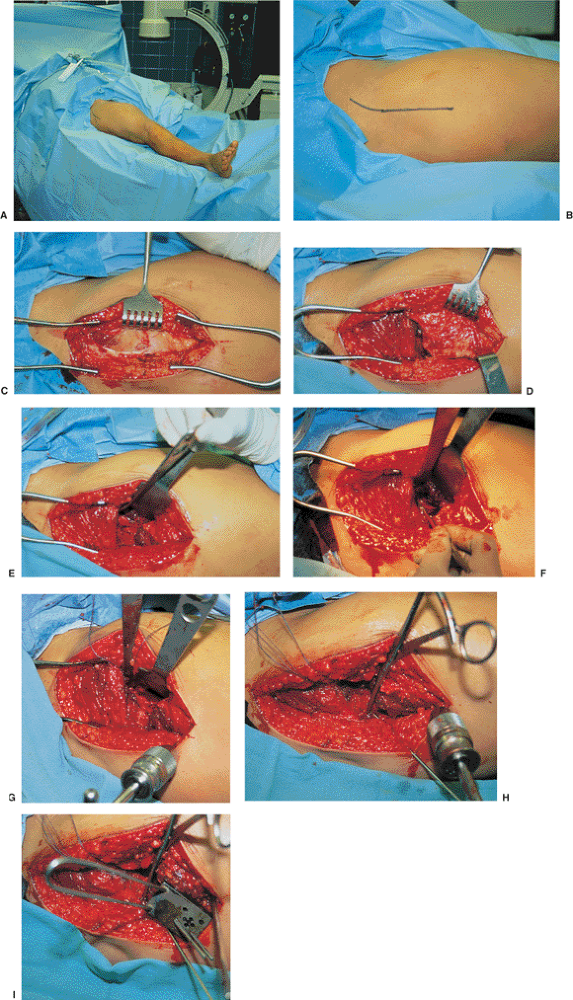
draped freely on a radiolucent table (Fig. 14.1A)
or on a fracture table in the supine position. If the latter is chosen
(which is the best method for obtaining high-quality lateral
radiographs), only light traction should be applied. This allows some
ability to manipulate the leg during surgery. If the former is chosen,
the lateral image is obtained by externally rotating the limb after
achieving temporary fixation. Before prepping and draping, the surgeon
must ensure that accurate AP and lateral fluoroscopic images are easily
obtainable.
preoperatively. The surgical approach is then done through a straight
lateral skin incision centered over the greater trochanter. In obese or
muscular patients, the proximal end of the incision must be curved
anteriorly toward the gluteal pillar of the iliac crest. This allows
easier dissection of the distal interval between the tensor fascia lata
and gluteus maximus muscles (see Fig. 14.1B).
incision, after which the interval between the tensor fascia and
gluteus medius muscles is developed (Watson-Jones approach) (see Fig. 14.1C,D).
The hip capsule is then identified by sweeping the pericapsular fat
medially and inserting a Hohmann retractor along the anterior
acetabular rim (see Fig. 14.1E). The capsule is then opened along the axis of the femoral neck (see Fig. 14.1F).
This can be done with minimal soft-tissue stripping, allowing the
surgeon to assess the reduction of the femoral fracture directly and
under fluoroscopic guidance. A small blade on a long handle can be used
under fluoroscopic control to limit the deep dissection.
encountered in approximately 15% of patients regardless of the amount
of fracture displacement or age of the patient (10).
The surgeon must be convinced that the fracture is anatomically reduced
before using the limited open technique. When an open reduction is
necessary, the capsule is dissected from the intertrochanteric ridge,
and its edges tagged with a no. 1 nonabsorbable suture for retraction.
A head lamp is very helpful to provide illumination. Another useful
technique to aid reduction is placement of a 5-mm Schanz pin in the
lateral aspect of the proximal femur distal to the planned insertion of
the cannulated screws (see Fig. 14.1G). The
fracture is manually distracted by lateral and distal traction on the
pin, and the proximal fragment is lifted anteriorly with a blunt curved
instrument or a Steinmann pin used as a joystick in the femoral head.
The fracture reduction is completed by internal rotation of the distal
fragment and by lifting the upward on the Schanz pin and applying a
compressive force perpendicular to the plane of the fracture.
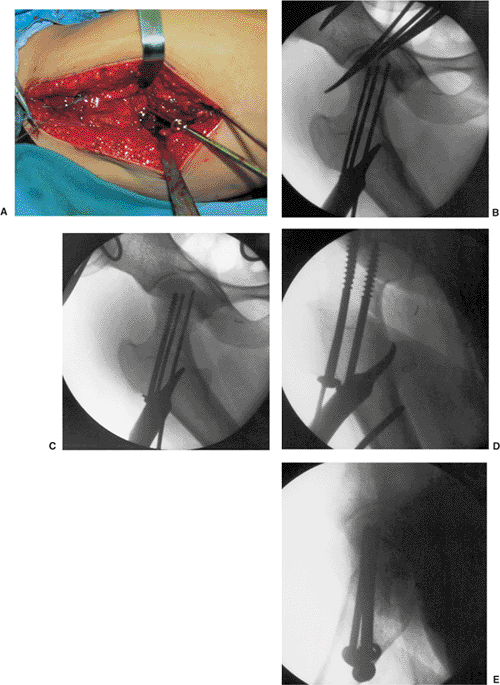
Provisional fixation is achieved using three K wires or cannulated
3.2-mm guide wires placed with the aid of biplanar image
intensification (see Fig. 14.1H). Definitive fixation is achieved with cannulated or noncannulated screws (see Figs. 14.1I and 14.2). Several biomechanical studies (11,12)
have shown no benefit from using more than three screws when an
anatomic reduction is achieved. Furthermore, there is no advantage in
postreduction stability among similar implants. A sliding hip screw has
not been shown to increase mechanical stability when anatomic reduction
has been achieved. However, this device may be of some benefit when the
reduction is not anatomic because it relies on the side-plate fixation
to the femoral shaft to resist angular displacement of the fracture
rather than the cancellous bone of the femoral head and neck.
can often be obtained by aligning the anterior cortices of the femoral
neck. In these cases, it is helpful to insert the anterosuperior screw
first because it helps to minimize fracture angulation when more
posterior screws are inserted and tightened. A sliding hip screw may
also be used when comminution is present to avoid angulation when the
fracture is compressed.
with a limited number of nonabsorbable sutures. The vastus lateralis is
allowed to fall back into place, and the fascia is reapproximated over
a drain with interrupted absorbable sutures. The subcutaneous fat is
reapproximated with a limited number of absorbable sutures and the skin
is reapproximated with a nylon 3-0 suture or staples. Intravenous
first-generation cephalosporins are continued for 24 hours
postoperatively.
 |
|
Figure 14.1. A.
The technique of open reduction is illustrated in this markedly displaced femoral-neck fracture. Positioning of the patient supine on a radiolucent table; as an alternative, a fracture table can be used. B. The skin incision is 8 to 10 cm long and centered over the Precter trochanter. This patient’s foot is to the reader’s right. C. After incising the fascia lata, the surgeon develops the interval between the tensor and gluteus medius muscles. This is visible in the proximal (left side) portion of the wound. D,E. The final exposure of the anterior aspect of the hip fracture is accomplished, first by elevating the vastus lateralis off the intertrochanteric ridge (D) and then by sweeping the pericapsular fat medially and inserting a Hohmann retractor along the anterior aspect of the acetabulum (E). F. The hip capsule is incised in line with the neck of the femur, and any collected intracapsular hematoma is evacuated. G. The reduction maneuver is performed with traction via a Schanz pin in the proximal femur with posterior translation of the shaft relative to the neck with a spiked pusher. The final reduction of the displaced neck fracture is accomplished by internal rotation of the leg by using the Schanz pin. H. The first guide wire is inserted after an anatomic reduction is documented with biplanar fluoroscopy and confirmed under direct vision. I. A second guide wire is placed parallel with the first by using a drill guide. |
is expected, and there is a 20% to 30% chance of osteonecrosis. Only
70% of patients older than 65 years reach their prefracture functional
level. A 12% risk of death related to the fracture (excess of mortality
over age-matched controls) should be expected.
protected weight-bearing with crutches or a walker, allowing progress
in weight-bearing as comfort dictates. Koval et al (13)
have shown that elderly patients will increase their weight bearing on
the injured hip as comfort allows. Patients who are able to maintain
limited weight bearing (up to 50% of body weight) on the injured limb
should continue to do so for 12 weeks. In patients older than 60 years,
this is generally accomplished with a walker, whereas younger patients
generally use crutches. In patients with upper-extremity injuries or
those who do not have enough upper-extremity strength and balance to
use crutches or a walker, postoperative care must be individualized.
Early, excessive, weight bearing has been shown to increase the risk of
redisplacement of the fracture, and in these cases the patient may need
a wheelchair for a short period. Physical therapy consultation for gait
retraining is appropriate. Range-of-motion exercises are generally
unnecessary.
 |
|
Figure 14.2. A. The screws are inserted one at a time starting with the anterior-superior screw. B,C.
The first screw is placed anteriorly and superiorly to generate compression and initial stability opposite the posterior cortex, which may be comminuted and unstable. D,E. The final position of the implants and quality of the reduction is confirmed on final fluoroscopic images. |
venous thrombosis (DVT) screening and prophylaxis until the patient is
mobile. A Doppler duplex scan is obtained within the first 36
postoperative hours and then weekly thereafter until the patient is
fully mobilized. Enoxaparin (Lovenox) and low-dose warfarin (Coumadin)
are equally efficacious for prophylaxis. Follow-up radiographs should
be obtained monthly until the fracture is healed. Patients are seen
annually for at least 3 years to rule out the presence of posttraumatic
osteonecrosis.
In a meta-analysis on the outcome after displaced femoral-neck
fractures, the risk of avascular necrosis in older patients was 16 %,
and the risk of nonunion was 30% (14). The rate
of nonunion in younger patients ranged from 0% to 86%, and avascular
necrosis was 20% to 59%. These complications are related to the degree
of initial displacement, the accuracy of reduction, and timing of the
surgical intervention. In a more recent meta-analysis utilizing only
controlled trials, weighted-mean revision rates after internal fixation
were 18.5% and 9.5 % for nonunion and avascular necrosis, respectively (15).
functionally. In one series, nearly all patients younger than 50 years
had symptoms severe enough to require additional surgery, whereas older
patients required reoperation in only 30% to 50% of cases (16). Therefore, symptoms are related to functional demand and can be successfully treated with arthroplasty.
with corrective osteotomy or joint arthroplasty. In physiologically
younger patients, nonunion can be treated with a closing wedge valgus
osteotomy and fixation with a 120-degree blade plate. Marti et al (16)
reported on 50 patients who underwent osteotomy, 37 of whom were
followed up for a minimum of 7 years and achieved an average Harris hip
score of 90. In an interesting result, 22 of these patients had
radiographic evidence of avascular necrosis, illustrating that this
complication is not always functionally devastating. Less common
complications include infection, DVT, pulmonary embolism, loss of
reduction, and subtrochanteric fracture through the lateral screw holes
in the lateral cortex of the proximal femur. Loss of reduction is
almost always related to poor bone quality or poor reduction, and it
should be treated with repeat reduction and internal fixation (usually
by switching to a sliding hip screw) if the patient’s bone density is
good, and with a cemented prosthesis if bone density is poor. Deep
infection is managed with early aggressive surgical debridement,
culture-specific antibiotics, and closure over a drain. Hip motion
should be limited until the wound is sealed.
J, Cserhati P, Bosch U, et al. Intracapsular femoral neck fractures:
the importance of early reduction and stable osteosynthesis. Injury 2002;33:41–46.
JE, McCarthy RE, Lowell JD, et al. Hip fracture mortality: relation to
age, treatment, preoperative illness, time of surgery, and
complications. Clin Orthop 1984;186:45–56.
GH, Harper WM, Connolly CD, et al. Preoperative skin traction for
fractures of the proximal femur: a randomised prospective trial. J Bone Joint Surg Br 1993;75(5):794–796.
B. Femoral head vitality after intracapsular hip fracture: 490 cases
studied by intravital tetracycline labeling and Tc-MDP radionuclide
imaging. Acta Orthop Scand 1983;200: 1–71.
KP, Spritzer CE, Harrelson JM, et al. Magnetic resonance imaging of the
femoral head after acute intracapsular fracture of the femoral neck. J Bone Joint Surg Am 1990;72(1):98–103.
ER, Lachiewicz PF, Gilbert JA. Internal fixation of femoral neck
fractures: a comparative biomechanical study of Knowles pins and 6.5-mm
cancellous screws. Clin Orthop 1991;267:85–92.
MF, Harrington RM, Keller TS, et al. Torsion and bending analysis of
internal fixation techniques for femoral neck fractures: the role of
implant design and bone density. J Orthop Res 1987;5(3):433–444.
KJ, Sala DA, Kummer FJ, et al. Postoperative weight-bearing after a
fracture of the femoral neck or an intertrochanteric fracture. J Bone Joint Surg Am 1998;80(3):352–356.
GL, Keller RB, Littenberg B, et al. Outcomes after displaced fractures
of the femoral neck: a meta-analysis of one hundred and six published
reports. J Bone Joint Surg Am 1994;76(1):15–25.
M, Devereaux PJ, Swiontkowski MF, et al. Internal fixation compared
with arthroplasty for displaced fractures of the femoral neck: a
meta-analysis. J Bone Joint Surg Am 2003;85:1673–1681.
