Charcot-Marie-Tooth Disease
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Charcot-Marie-Tooth Disease
Charcot-Marie-Tooth Disease
Dhruv B. Pateder MD
Description
-
Charcot-Marie-Tooth disease is the most common hereditary motor and sensory neuropathy.
-
Involvement progresses from distal to proximal: Lower extremity wasting, weakness, and cavovarus feet develop (Fig. 1), followed in some cases by upper extremity weakness.
-
5 recognized types (1):
-
Type I (hypertrophic form):
-
The most common form (50% of patients)
-
Thickened nerves have abnormal myelin that breaks down, leading to slowed nerve conduction.
-
-
Type II (axonal form) is characterized by
generally severe disease, with intact reflexes and a mild decrease in
nerve conduction velocities secondary to axonal degeneration. -
Type III (Dejerine-Sottas disease) shows marked segmental demyelination.
-
Type IV is autosomal recessive.
-
Charcot-Marie-Tooth-X is X-linked inheritance (~10% of cases) (2).
-
Risk Factors
Genetics
-
Charcot-Marie-Tooth disease is caused by a mutation in the gene for the peripheral myelin protein 22-kDa.
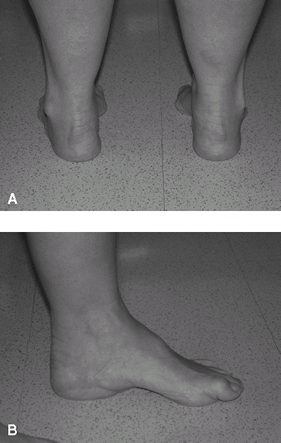 Fig. 1. Clinical photographs of foot deformity in Charcot-Marie-Tooth disease. Posterior view shows hindfoot varus (A). Medial view shows high arch and hallux clawing (B).
Fig. 1. Clinical photographs of foot deformity in Charcot-Marie-Tooth disease. Posterior view shows hindfoot varus (A). Medial view shows high arch and hallux clawing (B). -
Inheritance patterns include:
-
Autosomal dominant with variable penetrance: Types I, II, and III
-
Autosomal recessive: Type IV
-
X-linked: Type CMT-X
-
Pathophysiology
-
Characterized by progressive weakness of
the intrinsic muscles of the foot, peroneal muscles, and dorsiflexors
of the foot and toes -
Intrinsic weakness leads to characteristic clawing of the toes.
-
Relative weakness of the anterior
tibialis and peroneus brevis leads to plantarflexion of the 1st
metatarsal, which causes dynamic hindfoot inversion with gait. -
Chronic deformity leads to relative stiffness of the foot, impaired shock absorption, and arthritis.
-
Long-standing hindfoot varus can lead to lateral ankle ligament attenuation and symptoms of instability.
Associated Conditions
-
Scoliosis develops in 10% of patients (3).
-
Hip dysplasia develops in 6–10% of patients and presents at a later age than does the idiopathic form (4).
Signs and Symptoms
-
Patients usually present at 10–20 years of age with a high arch, loss of endurance or coordination, or a “steppage” gait.
-
Their shoes wear out rapidly and unevenly because of progressive cavovarus foot alignment.
-
-
On examination:
-
Weakness is present in the ankle evertors and dorsiflexors before the plantarflexors and invertors.
-
Sensation and proprioception are diminished.
-
There may be increased circumduction of
the extremity or steppage pattern during the swing phase of gait to
allow clearance of dropfoot.
-
History
-
Identify family members with similar foot deformities.
-
Note progression of deformity, weakness, and giving-way of the ankle.
-
Identify site(s) of pain about the ankle and foot.
Physical Exam
-
The calf usually is atrophied.
-
Record and monitor foot and ankle muscle strength.
-
Test sensation.
-
Examine the position of the foot at rest for the presence of hindfoot varus.
-
This aspect is most strongly related to functional problems.
-
If present, assess for rigidity by
placing a lift under the lateral side of the forefoot and seeing
whether the hindfoot varus corrects (Coleman block test). -
Assess passive correction of the hindfoot varus.
-
-
Assess the lateral ankle ligaments for laxity and instability.
-
Note the relative plantarflexion of the 1st metatarsals compared with that of the others.
-
Record the presence or absence of toe clawing.
-
Observe the patient’s gait, including the presence or absence of steppage or circumduction gait.
-
Examine the hips for abduction.
-
Check for scoliosis with a forward bend test.
-
Check the upper extremities for wasting of the ulnar-innervated hand muscles, including the abductors and interossei.
Tests
-
Electromyography and nerve conduction velocities usually are performed for diagnosis.
-
The electromyogram shows increased duration and decreased amplitude of the motor action potentials.
-
Nerve conduction velocity testing shows decrease in motor and sensory conduction velocity.
-
-
Biopsy:
-
Muscle biopsy shows atrophy.
-
Nerve biopsy shows loss of myelinated fibers.
-
These biopsies are not indicated routinely if the history and electrodiagnostic tests are characteristic.
-
-
DNA testing is available through blood testing for early diagnosis or family analysis.
Imaging
-
Radiography:
-
Obtain standing radiographs of the foot and ankle to assess alignment and identify arthritis.
-
Obtain spinal films in the index patient without a family history, to rule out spinal disorders.
-
Once a diagnosis is made, the physician
should have a low threshold for ordering pelvic films to rule out
dysplasia if limitation of abduction is present.
-
-
Depending on the index of suspicion, MRI
of the spine may be indicated because it can visualize corticospinal
tract abnormalities.
Pathological Findings
-
Muscle biopsy displays diffuse atrophy and replacement of muscle fibers with fibrous and adipose tissue.
-
Nerve biopsy shows loss of myelinated fibers and increased fibrous tissue in the endoneurium and perineurium.
-
The pathogenesis of the cavovarus foot:
-
Progressive weakness of the lumbricals,
interossei, peroneals, and extensors that leaves the long toe flexors
and ankle invertors unopposed. -
Claw toes develop, and the plantar fascia and intrinsic muscles contract.
-
Differential Diagnosis
-
Tethered spinal cord
-
Myelomeningocele, lipomeningocele
-
Peroneal nerve palsy
-
Early stages of Duchenne muscular dystrophy
-
Other hereditary motor and sensory neuropathies
P.69
General Measures
-
Patients should be seen on a routine basis to monitor for worsening deformity.
-
Stretching of the Achilles tendon and the plantar fascia may be helpful.
-
Custom orthotic insoles with lateral heel
build-up may improve hindfoot alignment, whereas forefoot accommodative
padding may relieve metatarsalgia secondary to claw-toe deformities. -
Ankle bracing may assist in patients with instability symptoms.
-
A custom ankle–foot orthosis may be necessary for patients with severe drop foot secondary to extensor weakness.
-
Comfortable shoe wear with adequate toe boxes and cushioned heels is recommended.
Special Therapy
Physical Therapy
Therapy involves stretching of the Achilles tendon and
plantar fascia, strengthening exercises, and proprioceptive training to
assist with ankle instability.
plantar fascia, strengthening exercises, and proprioceptive training to
assist with ankle instability.
Surgery
-
Treatment consists of addressing individual components of deformity:
-
Claw-toe correction
-
Flexor-to-extensor transfer, MTP joint release, and PIP fusion
-
Hallux IP arthrodesis and extensor hallucis longus transfer to 1st metatarsal (Jones procedure)
-
-
Plantar release (plantar fascia, abductor
hallucis, toe flexors) or plantar–medial release (includes posterior
tibialis and long toe flexor lengthening and talonavicular capsulotomy) -
Tendon transfer: Split or whole transfer of the posterior tibialis to assist with dorsiflexion and eversion
-
Peroneus longus tenodesis to peroneus brevis
-
Calcaneal lateral closing wedge osteotomy for rigid hindfoot varus
-
Midtarsal or metatarsal closing wedge osteotomies
-
Triple arthrodesis for rigid deformity or hindfoot arthritis
-
Ankle ligament reconstruction for instability
-
Disposition
Issues for Referral
Consultation by a neurologist is warranted for
electromyographic testing and peripheral blood tests for diagnosis and
genetic counseling.
electromyographic testing and peripheral blood tests for diagnosis and
genetic counseling.
Prognosis
-
Usually, the foot cannot be made fully normal even after surgery, and the muscle weakness progresses.
-
Life expectancy is not shortened.
Complications
-
Missed hip dysplasia means more difficult or less successful treatment.
-
May recur after surgery if soft-tissue procedures are performed in patients with a fixed bony deformity.
-
Transfer of stress with degeneration of the ankle or midfoot may occur, especially after triple arthrodesis.
Patient Monitoring
Patients are checked yearly for ambulatory function.
References
1. Kirchner
JS. Charcot-Marie-Tooth disease and the cavovarus foot. In: Richardson
EG, ed. Orthopaedic Knowledge Update: Foot and Ankle 3. Rosemont, IL:
American Academy of Orthopaedic Surgeons, 2004:135–143.
JS. Charcot-Marie-Tooth disease and the cavovarus foot. In: Richardson
EG, ed. Orthopaedic Knowledge Update: Foot and Ankle 3. Rosemont, IL:
American Academy of Orthopaedic Surgeons, 2004:135–143.
2. Guyton GP, Mann RA. The pathogenesis and surgical management of foot deformity in Charcot-Marie-Tooth disease. Foot Ankle Clin 2000;5:317–326.
3. Hensinger
RN, MacEwen GD. Spinal deformity associated with heritable neurological
conditions: spinal muscular atrophy, Friedreich’s ataxia, familial
dysautonomia, and Charcot-Marie-Tooth disease. J Bone Joint Surg 1976;58A:13–24.
RN, MacEwen GD. Spinal deformity associated with heritable neurological
conditions: spinal muscular atrophy, Friedreich’s ataxia, familial
dysautonomia, and Charcot-Marie-Tooth disease. J Bone Joint Surg 1976;58A:13–24.
4. Pailthorpe CA, Benson MKD. Hip dysplasia in hereditary motor and sensory neuropathies. J Bone Joint Surg 1992;74B:538–540.
Additional Reading
Kassubek J, Bretschneider V, Sperfeld AD. Corticospinal tract MRI hyperintensity in X-linked Charcot-Marie-Tooth disease. J Clin Neurosci 2005;12:588–589.
Kobsar
I, Hasenpusch-Theil K, Wessig C, et al. Evidence for
macrophage-mediated myelin disruption in an animal model for
Charcot-Marie-Tooth neuropathy type 1A. J Neurosci Res 2005;81:857–864.
I, Hasenpusch-Theil K, Wessig C, et al. Evidence for
macrophage-mediated myelin disruption in an animal model for
Charcot-Marie-Tooth neuropathy type 1A. J Neurosci Res 2005;81:857–864.
McCluskey WP, Lovell WW, Cummings RJ. The cavovarus foot deformity. Etiology and management [see comments]. Clin Orthop Relat Res 1989;247:27–37.
Miller MJ, Williams LL, Slack SL, et al. The hand in Charcot-Marie-Tooth disease. J Hand Surg 1991;16B:191–196.
Roper BA, Tibrewal SB. Soft tissue surgery in Charcot-Marie-Tooth disease. J Bone Joint Surg 1989;71B:17–20.
Wetmore RS, Drennan JC. Long-term results of triple arthrodesis in Charcot-Marie-Tooth disease. J Bone Joint Surg 1989;71A:417–422.
Codes
ICD9-CM
-
356.1 Charcot-Marie-Tooth disease
-
735.5 Claw toe
-
736.75 Cavovarus foot
Patient Teaching
-
Stress the importance of stretching and routine follow-up.
-
DNA testing may be helpful to provide for genetic counseling.
-
Discuss the risks of scoliosis and hip dysplasia.
FAQ
Q: What is the basic pathophysiology of Charcot-Marie-Tooth disease?
A:
Inherited motor–sensory neuropathy with resultant preferential weakness
of the intrinsic muscles of the hands and feet along with ankle
extensors and evertors.
Inherited motor–sensory neuropathy with resultant preferential weakness
of the intrinsic muscles of the hands and feet along with ankle
extensors and evertors.
Q: What is the typical foot deformity seen in Charcot-Marie-Tooth disease?
A: Cavovarus deformity and claw toes.
