CHAPTER 74 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 74 – Distal Realignment for Patellofemoral Disease
Although the emphasis of this chapter is on tibial tuberosity surgery for patellofemoral disease, the multifactorial nature of patellofemoral dysfunction requires an acknowledgement that a patellofemoral problem is rarely addressed by a single surgical treatment. tibial tuberosity repositioning must be examined with a full appreciation of proximal soft tissue balance, limb rotation, and articular cartilage disease (grade, site, and extent). Although positive outcomes were initially reported for many distal realignment patellofemoral surgeries, early positive results often deteriorated markedly over time. In the case of the Hauser posterior medial tuberosity transfer, although stability was maintained, patellofemoral cartilage degeneration predictably occurred over time. Thus, in general, patellofemoral surgery not only must address the acute problem but do so without causing intermediate and long-term problems, such as chondrosis and arthrosis. Application of a more scientific approach to patellofemoral dysfunction has led to the identification of the importance of the medial patellofemoral ligament (MPFL) in restraint to lateral patellar instability, and it has refined and focused the limited role of lateral release to isolated, documented patellar tilt rather than global patellofemoral pain or instability. Likewise, the role of tibial tuberosity surgery for patellofemoral dysfunction continues to evolve both as an isolated procedure and in conjunction with proximal patellofemoral surgery.
Indications espoused for tuberosity surgery (often in combination with proximal soft tissue surgery) at one point included patellofemoral pain, instability, chondrosis, and arthrosis. Straight tibial tuberosity medialization (TTM) was initially associated with the names of specific surgeons, including Roux, Elmslie, and Trillat; anteriorization, with Maquet; and anteromedialization (AMZ), with Fulkerson. These tuberosity surgeries have, at times, been used to treat static patellar subluxation, recurrent lateral patellar instability, patellar pain, and patellofemoral chondrosis. Tuberosity surgery for treatment of recurrent or chronic patellofemoral dislocation or subluxation was based on the assumption that the primary pathologic process was an increased Q (quadriceps) angle; for pain and chondrosis, elevation was promoted as the preferred procedure to dramatically decrease patellofemoral stress. Whereas it is obvious that repositioning of the distal point of the Q angle (tibial tuberosity) surgically does modify the Q angle, today the MPFL is accepted as the main restraint to lateral patellar instability. In fact, the Q angle, which formed the rational basis for planning of a TTM, is being questioned as a benchmark in light of the poor intraobserver and interobserver reproducibility of the measurement as reviewed by Post. In addition, Fithian is questioning the role of TTM for lateral patellar instability. At the annual meeting of the American Orthopaedic Society for Sports Medicine in 2005, he presented a case series of recurrent lateral patellar instability treated by MPFL reconstruction with or without TTM. The results were the same in both groups. On the other hand, it must be acknowledged that Cox has reported excellent long-term results in prevention of recurrent patellar instability with TTM, although critics note that his report is a clinical outcome series without radiographs that might have demonstrated arthrosis (as predicted to occur with excessive medialization of the tuberosity in biomechanical studies by Andrish and Kuroda). Furthermore, as the extent of medialization with TTM has been variably defined, critics could imply that (1) some of the patients with instability successfully treated by TTM had spontaneous healing of the MPFL, (2) the MPFL lesion was marginally injured, or (3) the TTM “overmedialized” the tuberosity and constrained the patella into stability.
From a basic science approach, the initial tuberosity surgery focused on the action of the various force vectors on patellar position and motion and on the effect of tuberosity position on those vectors. However, the equation is more complicated, as Teitge, Powers, Heino, and others have emphasized the importance of the “other half” of the joint in motion: the trochlea and associated tibiofemoral torsion. Furthermore, Dejour has brought to attention the importance of trochlear morphologic features (dysplasia) in patients with lateral patellar instability. In an attempt to objectify tuberosity surgery, we must define normal and abnormal positions of the tuberosity. We must additionally consider the extent of femoral internal torsion and tibial external torsion as per Teitge and Heino.
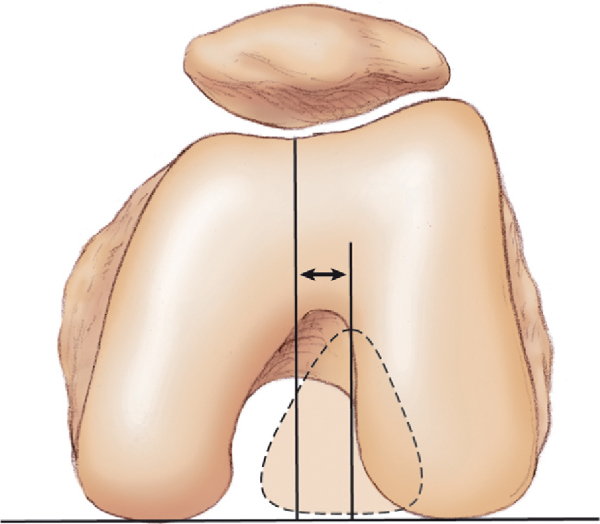
This objective approach to limb coronal and axial alignment from hip to ankle also measures (at the knee) an objective alternative to the Q angle, that is, the tibial tuberosity to trochlear groove (TT-TG) distance (
Fig. 74-1
). The TT-TG distance, as popularized by Dejour, quantitates the concept of tibial tuberosity malalignment locally at the knee. Studies suggest that a TT-TG distance of more than 15 to 20 mm is abnormal; most asymptomatic patients have distances that are less than 15 mm. Likewise, anteriorization was first shown mathematically to reduce patellofemoral stress, but direct measurements with pressure-sensitive film, real-time pressure transducer arrays, and finite element analysis modeling such as by Cohen and Ateshian show that although stresses are typically reduced with anteriorization, there is a unique response for each knee, and a global “50%” force reduction cannot be assumed. Thus, load transfer should play an important role in surgical planning, rather than assuming that there will be an absolute decrease in stress. By use of these and other objective parameters, future studies may objectively quantify the preoperative pathologic process to aid in planning of tuberosity surgery.
|
|
|
|
Figure 74-1 |
Subgroups considered for tuberosity surgery are those with static subluxation of the patella, those with patellofemoral chondrosis that requires load optimization, and those with recurrent lateral instability with or without static subluxation. The history will be highly variable for each subgroup, from insidious onset of patellofemoral pain to pain that began after a patellar instability episode. The standard patellofemoral history as outlined by Post should be elicited. Functional aspects need to be documented, including the amount of energy needed to cause instability and the degree of stress necessary to cause pain. Prior surgical operative notes are useful, as are intraoperative photographs.
Patellofemoral symptoms are ubiquitous but nonetheless must be documented as to functional impairments with respect to pain, crepitation, swelling, giving way, and frank patellar instability and loose body sensations. Clinical signs overlap with the physical examination findings and include documentation of crepitation during the specific arc of motion, effusion, and loose body appearance.
As for all patients with patellofemoral dysfunction, a standard examination is performed of the knee and the entire functional kinetic chain from the pelvis to the foot. A standard patellofemoral examination as detailed by Post pays particular attention to the following:
Magnetic resonance imaging with or without contrast enhancement will add information about the extent and position of articular cartilage disease. Magnetic resonance imaging or computed tomography delineates patellofemoral morphologic features (extent of dysplasia), evaluates congruity of the patella in the trochlea, and provides objective measurement of the TT-TG distance and patellar height—with the understanding that cartilage contour does not always match bone contour.
Technetium bone scan may indicate areas of overload and arthrosis or suggest complex regional pain syndrome (sympathetically mediated pain).
Indications and Contraindications
Indications for Tibial Tuberosity Medialization
Indications for Anteromedialization
Contraindications to Tibial Tuberosity Medialization
Contraindications to Anteromedialization (without cartilage restoration)
The goal of medialization is normalization of the tuberosity position rather than overmedialization, so preoperative radiographic or clinical assessment of TT-TG distance is useful in planning.
If lateral release and MPFL repair (or reconstruction) are performed in conjunction with TTM or AMZ, the procedure order is lateral release, then tuberosity surgery, and finally MPFL surgery. If cartilage restoration is planned, in addition to the TTM or AMZ, these procedures can be performed concomitantly to reduce total knee exposure to surgery and to ease the patient’s rehabilitation.
The less invasive TTM can be performed under local anesthetic with sedation. TTM as well as AMZ may be performed by use of regional blocks (femoral and sciatic), with postoperative femoral nerve block for prolonged pain control. Alternatively, epidural, spinal, or general anesthetics may be used according to the surgeon’s preference. Both AMZ and TTM are performed with the patient in the supine position, often with a roll under the ipsilateral pelvis to decrease external rotation. In light of bone surgery, they are often performed with the foot of the operating table elevated and a side post used for the arthroscopic portion of the procedure rather than with the foot in a dependent position.
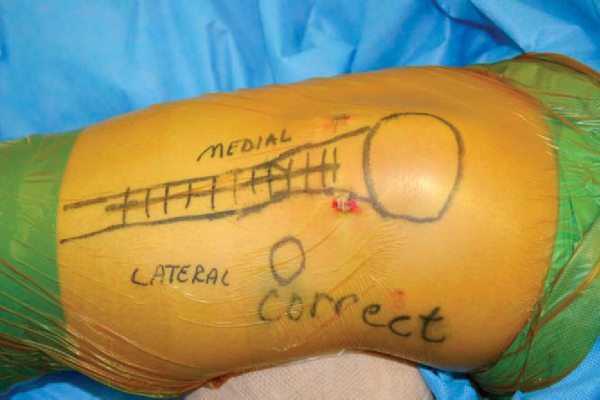
Surgical Landmarks, Incisions, and Portals (
Fig. 74-2
)
| • | Patella | |
| • | Trochlear margins | |
| • | Patellar tendon attachment to tibial tuberosity | |
| • | Gerdy tuberosity | |
| • | Crest of tibia |
|
|
|
|
Figure 74-2 |
| • | Anterior tibial artery | |
| • | Deep peroneal nerve | |
| • | Patellar tendon | |
| • | Sites of long-term overload (leading to chondrosis). |
Examination Under Anesthesia and Diagnostic Arthroscopy
Under anesthesia, range of motion (comparison of passive patellar tracking to known preoperative active) and the full extent of patellar displacement and tilt are documented. Diagnostic arthroscopy allows mapping and grading of all areas of chondrosis. These findings enter into final planning and in some instances suggest cancellation of the tuberosity surgery in light of discovery of a contraindication.
The arthroscopic examination documents the associated tibiofemoral and patellofemoral chondral (grade and region of lesions) and morphologic features of the pathologic process. This information allows fine-tuning of the tuberosity surgery for the indications listed before. Arthroscopic chondral treatment may be performed as indicated, followed by titration of the lateral release, if necessary. For those patients with reversible patellar tilt and significant medial patellar displacement (two trochlear quadrants), a lateral release will not be performed; for patients with patellar tilt and minimal medial patellar displacement (one trochlear quadrant or less), a limited lateral release or stepcut lateral lengthening will be titrated to allow reversal of tilt and to achieve two quadrants of medial patellar displacement.
Specific Steps (
Box 74-1
)
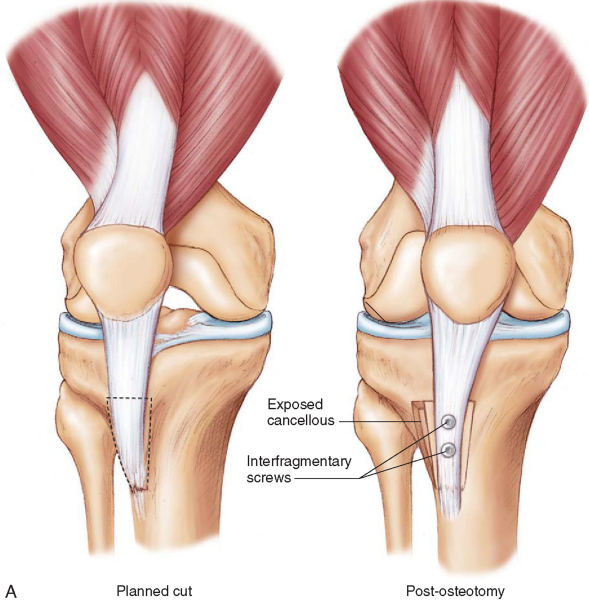
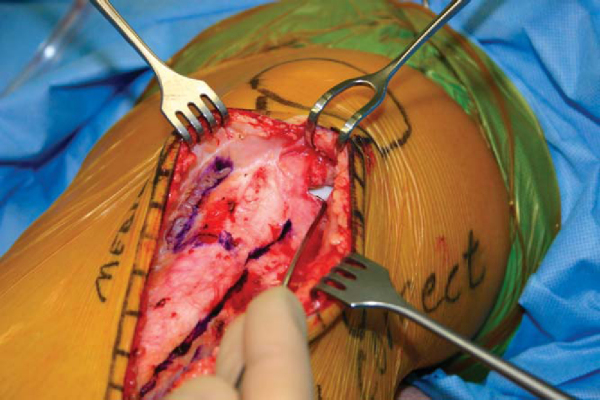
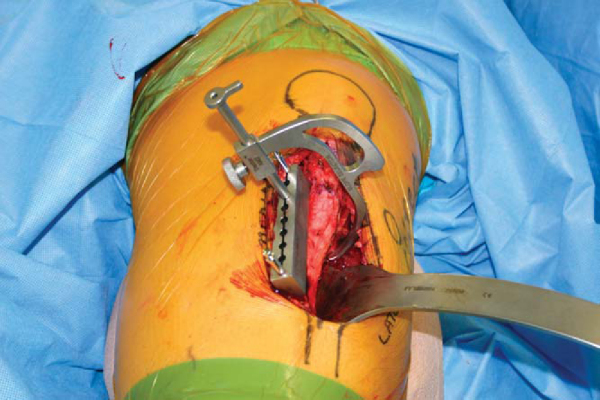
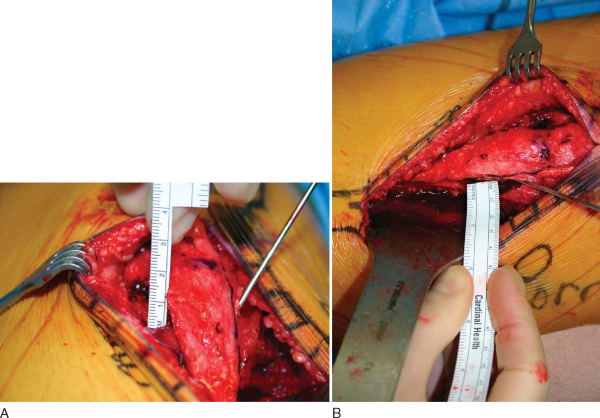
Tibial Tuberosity Medialization (
Fig. 74-3A and B
)
The skin incision is based on whether the TTM is an isolated or combined surgery. The standard longitudinal incision is made lateral to the tibial tuberosity, with approximately 2 cm of the incision above the tuberosity and 3 cm of the incision below the tuberosity. It may be modified to a more universal direct anterior longitudinal approach as dictated by concomitant surgery. The patellar tendon is identified, and the lateral release (if it is performed) is extended along the lateral border of the patellar tendon with emphasis on hemostasis. A 1.5-cm subperiosteal exposure of the lateral aspect of the tibial tuberosity is performed.
| Surgical Steps | ||||||||||||
|
|
|
|
|
Figure 74-3 |
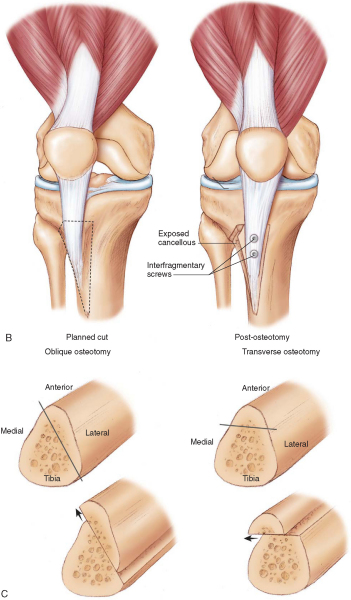
The coronal plane cut is referenced from the anterior joint lines to be flat in the coronal plane. If there is a desire to unload the distal lateral patella, the cut is made with a mild anteriorly directed slope (
Fig. 74-3C, right
).
3. Performance of the Osteotomy
A 1.5-cm-deep cut in the axial plane is performed just proximal to the protected patellar tendon proximal attachment to the tibial tuberosity. A second bone cut begins at the posterior aspect of this cut and extends distally for approximately 5 cm while remaining 1.5 cm posterior to the crest of the tibial tuberosity. With the distal anterior tibial crest kept intact, the tuberosity is rotated medially, making a greenstick fracture at the distal portion of the osteotomy. The tuberosity is medialized to the extent that the TT-TG distance is normalized, but not overmedialized.
The tuberosity is temporarily fixed with a Kirschner wire. Patellar tracking is viewed, and if it is acceptable, the tuberosity is fixed with interfragmentary screws (the screws are aimed medially, with care taken to avoid vascular injury).
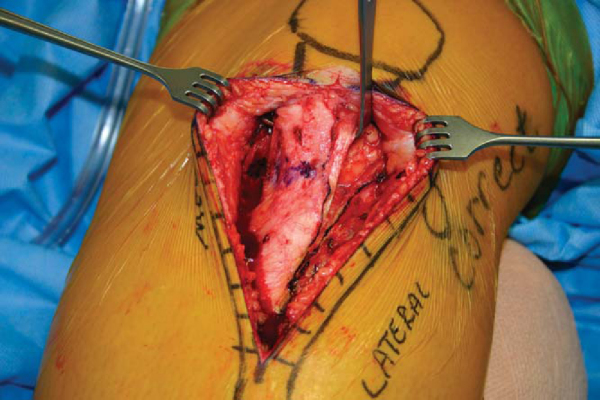
If the AMZ is an isolated procedure, begin the midline longitudinal incision midway between the patella and tuberosity and extend it distally 10 to 15 cm. Alternatively, the incision can course from the anterolateral portal to the same point on the tibial crest distally. Proximal extension may be performed to allow concomitant patellofemoral cartilage restoration. The patellar tendon is exposed subcutaneously. The lateral aspect of the patellar tendon is released, isolated, and protected. This lateral peripatellar tendon incision is extended proximally to the lateral release (noting the specific lateral release indications discussed earlier) and then distally along the anterior tibial crest to begin elevation of the anterior compartment musculature (
Fig. 74-4
). To allow anteriorization, a release is also performed immediately adjacent to the patellar tendon medially. The freed patellar tendon is protected with a retractor (
Fig. 74-5
). The anterior compartment musculature is subperiosteally dissected, and a retractor is positioned at the posterior extent of the lateral tibial wall to protect the posterior neurovascular structures (
Fig. 74-6
).
|
|
|
|
Figure 74-4 |
|
|
|
|
Figure 74-5 |
|
|
|
|
Figure 74-6 |
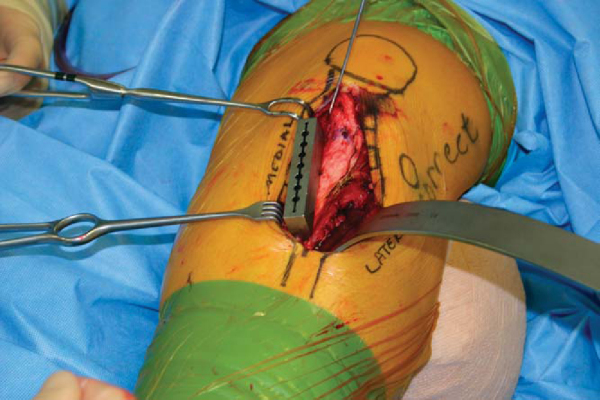
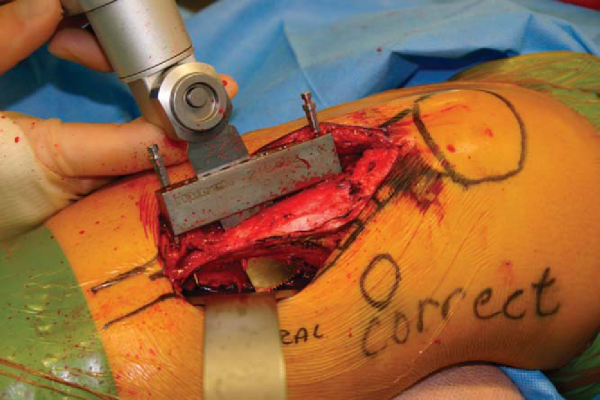
With use of a commercially available AMZ osteotomy system (Tracker by Mitek, Raynham, Mass), the osteotomy starting entrance position is planned by placing the cutting block jig medial to the patellar tendon attachment to the tibial tuberosity (
Fig. 74-7
). The planned osteotomy begins adjacent to the medial patellar tendon and courses laterally as it runs distally to allow the osteotomy to exit distally and laterally (a triangle shape). A drill guide–like arm is inserted into the cutting block. The tip of the slope selector arm predicts the lateral wall exit of the oblique osteotomy (
Fig. 74-8
). The tip (osteotomy exit) should be on the lateral wall of the tibia, always anterior to the posterior wall. With the cutting block immediately adjacent to the patellar tendon attachment medially and the slope selector tip just anterior to the posterior wall, the slope is approximately 60 degrees (
Fig. 74-3C, left
). By moving the cutting block medially and the slope selector anteriorly, the slope can be decreased, for example, to 45 degrees. A smaller angle provides increased medialization relative to anteriorization. That is, the suggested anteriorization of 1.2 to 1.5 cm is “constant,” and thus with a steep slope (60 degrees), the medial displacement would be 0.6 to 0.75 cm; for a 45-degree slope, the same elevation would allow 1.2 to 1.5 cm of medialization.
|
|
|
|
Figure 74-7 |
|
|
|
|
Figure 74-8 |
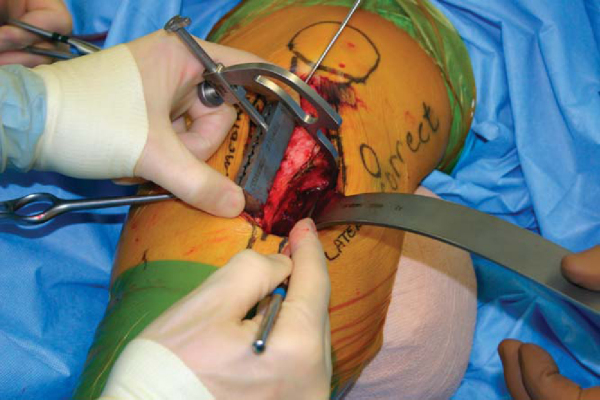
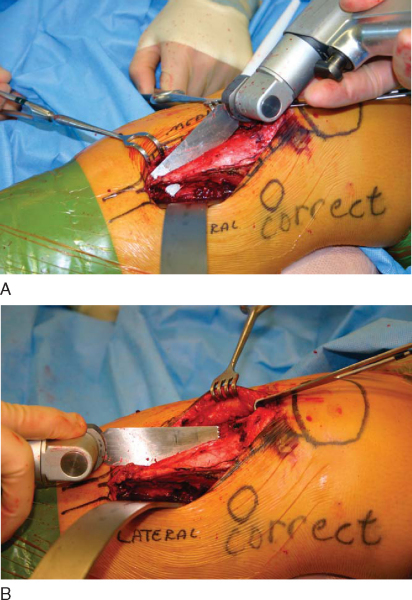
3. Performance of the Osteotomy
With the desired slope selected, the cutting block is temporarily fixed to the tibia with pins through drill holes (
Fig. 74-9
). The oblique cut is made with an oscillating saw cooled with saline. The saw is directly observed as it exits on the lateral wall of the tibia anterior to the retractor (
Fig. 74-10
). The cutting block is removed. The oblique cut is finished proximally and distally with use of the original bone cut as a captured saw guide (
Fig. 74-11
). To finish the proximal osteotomy, an osteotome connects the posterolateral wall saw exit site to the lateral aspect of the patellar tendon attachment to the tibial tuberosity (
Fig. 74-12
). Changing the angle of the osteotome, the last bone cut connects the previous cuts that have extended just proximal to the patellar tendon attachment to the tibial tuberosity medially and laterally. At this point, the tuberosity pedicle is free to rotate up the inclined slope.
|
|
|
|
Figure 74-9 |
|
|
|
|
Figure 74-10 |
|
|
|
|
Figure 74-11 |
|
|
|
|
Figure 74-12 |
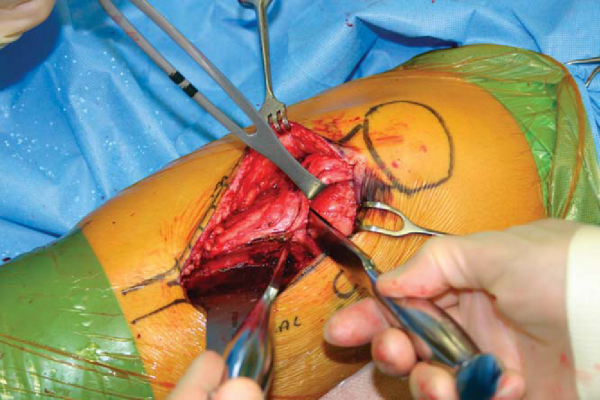
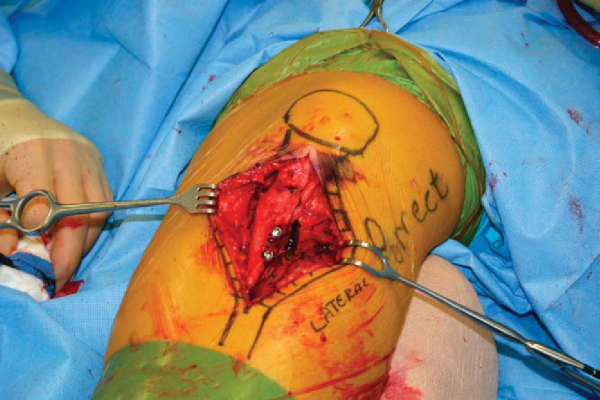
The completed oblique cut allows movement of the tuberosity pedicle up the inclined plane, affecting the desired anteromedialization. The tuberosity is temporarily fixed with a Kirschner wire, and the anteriorization and medialization are measured (
Fig. 74-13
). The tuberosity is fixed with interfragmentary technique, with avoidance of vascular structures as discussed by Miller (
Fig. 74-14
).
|
|
|
|
Figure 74-13 |
|
|
|
|
Figure 74-14 |
| • | Standard knee management includes a protective brace locked at or near extension initially, compression, cryotherapy, elevation, and possible continuation of the femoral nerve block ( Fig. 74-15 ). The limb is observed for compartment syndrome and any problems with skin healing. |
|
| • | Sutures and staples are removed at 7 to 10 days. | |
| • | Radiographs are typically obtained perioperatively and then at 6 weeks postoperatively. For comparison of preoperative and postoperative radiographs, see Figure 74-16 . |
|
|
|
|
Figure 74-15 |
|
|
|
|
Figure 74-16 |
Complications are similar to those of any open bone procedure of the knee. These include fracture, malunion, loss of fixation, nonunion, infection, thromboembolic phenomenon, compartment syndrome, sympathetically mediated pain, arthrofibrosis, patella infera, and long-term progression of patellofemoral chondrosis. Additionally, failure to address preoperative surgical indications may lead to postoperative complications.
Both short- and long-term case series for TTM and AMZ demonstrate high percentages of good and excellent results (
Table 74-1
). However, these are case series and need interpretation within the ranking of evidence-based medicine. In addition, these results need to be reviewed with biomechanical studies (i.e., Cohen and Kuroda) in mind.
| Investigator | Surgery Type | Followup (average) | Outcomes |
|---|---|---|---|
| Bellemans et al[2] (1997) | AMZ | 32 months | Lysholm scores: preoperative, 62; postoperative, 92 |
| Buuck and Fulkerson[3] (2000) | AMZ | 8.2 years | 86% good and excellent |
| Cameron et al[4] (1986) | AMZ | 2 years | 82% good and excellent |
| Carney et al[5] (2005) | TTM | 26 years | 54% good and excellent |
| Fulkerson[11] (1983) | AMZ | All patients received substantial relief of pain | |
| Fulkerson et al[12] (1990) | AMZ | 35 months | 89% good and excellent |
| Naranja et al[17] (1996) | TTM + Ant | 74.2 months | 53% good and excellent |
| Pidoriano et al[18] (1997) | AMZ | 46.8 months | 72% improvement |
| Sakai et al[20] (1996) | AMZ | 5 years | 20/21 satisfactory |
1.
Beck PR, Thomas AL, Farr J, et al: Trochlear contact pressures following anteromedialization of the tibial tubercle.
Am J Sports Med 2005; 33:1710-1715.
2.
Bellemans J, Cauwenberghs F, Witvrouw E, et al: Anteromedial tibial tubercle transfer in patients with chronic anterior knee pain and a subluxation-type patellar malalignment.
Am J Sports Med 1997; 25:375-381.
3.
Buuck D, Fulkerson J: Anteromedialization of the tibial tubercle: a 4- to 12-year followup.
Oper Tech Sports Med 2000; 8:131-137.
4.
Cameron HU, Huffer B, Cameron GM: Anteromedial displacement of the tibial tubercle for patellofemoral arthralgia.
Can J Surg 1986; 29:456-458.
5.
Carney JR, Mologne TS, Muldoon M, Cox JS: Long-term evaluation of the Roux-Elmslie-Trillat procedure for patellar instability.
Am J Sports Med 2005; 33:1220-1223.
6.
Cohen ZA, Henry JH, McCarthy DM: Computer simulations of patellofemoral joint surgery. Patient-specific models for tuberosity transfer.
Am J Sports Med 2003; 31:87-98.
7.
Cosgarea AJ, Schatzke MD, Seth A, Litsky AS: Biomechanical analysis of flat and oblique tibial tubercle osteotomy for recurrent patellar instability.
Am J Sports Med 1999; 27:507-512.
8.
Dejour H, Walch G, Nove-Josserand L, Guier C: Factors of patellar instability: an anatomic radiographic study.
Knee Surg Sports Traumatol Arthrosc 1994; 2:19-26.
9.
Farr J: Anteromedialization of the tibial tubercle for treatment of patellofemoral malpositioning and concomitant isolated patellofemoral arthrosis.
Tech Orthop 1997; 12:151-164.
10.
Ferrandez L, Usabiaga J, Yubero J, et al: An experimental study of the redistribution of patellofemoral pressures by the anterior displacement of the anterior tuberosity of the tibia.
Clin Orthop 1989; 238:183-189.
11.
Fulkerson JP: Anteromedialization of the tibial tuberosity for patellofemoral malalignment.
Clin Orthop 1983; 177:176-181.
12.
Fulkerson JP, Becker GJ, Meaney JA, et al: Anteromedial tibial tubercle transfer without bone graft.
Am J Sports Med 1990; 18:490-497.
13.
Heino Brechter J, Powers CM, Terk MR, et al: Quantification of patellofemoral joint contact area using magnetic resonance imaging.
Magn Reson Imaging 2003; 21:955-959.
14.
Kline AJ, Gonzales J, Beach WR, Miller MD: Vascular risk associated with bicortical tibial drilling during anteromedial tibial tubercle transfer.
Am J Orthop 2006; 34:30-32.
15.
Kuroda R, Kambic H, Valdevit A, Andrish JT: Articular cartilage contact pressure after tibial tuberosity transfer.
Am J Sports Med 2001; 29:403-409.
16.
Morshuis WJ, Pavlov PW, de Rooy KP: Anteromedialization of the tibial tuberosity in the treatment of patellofemoral pain and malalignment.
Clin Orthop 1990; 255:242-250.
17.
Naranja RJ, Reilly PJ, Kuhlman JR, et al: Long-term evaluation of the Elmslie-Trillat-Maquet procedure for patellofemoral dysfunction.
Am J Sports Med 1996; 24:779-784.
18.
Pidoriano AJ, Weinstein RN, Buuck DA, et al: Correlation of patellar articular lesions with results from anteromedial tibial tubercle transfer.
Am J Sports Med 1997; 25:533-537.
19.
Post WR: Clinical evaluation of patients with patellofemoral disorders.
Arthroscopy 1999; 15:841-851.
20.
Sakai N, Koshino T, Okamoto R: Pain reduction after anteromedial displacement of the tibial tuberosity: 5-year followup in 21 knees with patellofemoral arthrosis.
Acta Orthop Scand 1996; 67:13-15.