Calcaneus Fractures
-
Calcaneus fractures account for approximately 2% of all fractures.
-
The calcaneus, or os calcis, is the most frequently fractured tarsal bone.
-
Displaced intraarticular fractures comprise 60% to 75% of calcaneus fractures.
-
Ninety percent of calcaneus fractures
occur in men between 21 and 45 years of age, with the majority being in
industrial workers. -
Between 7% and 15% of calcaneus fractures are open injuries.
-
The anterior half of the superior
articular surface contains three facets that articulate with the talus.
The posterior facet is the largest and constitutes the major
weight-bearing surface. The middle facet is located anteromedially on
the sustentaculum tali. The anterior facet is often confluent with the
middle facet. -
Between the middle and posterior facets
lies the interosseous sulcus (calcaneal groove), which, with the talar
sulcus, forms the sinus tarsi. -
The sustentaculum tali supports the neck
of the talus medially; it is attached to the talus by the interosseus
talocalcaneal and deltoid ligaments and contains the middle articular
facet on its superior aspect. The flexor hallucis longus tendon passes
beneath the sustentacular tali medially. -
The peroneal tendons pass between the calcaneus and the lateral malleolus laterally.
-
The Achilles tendon attaches to the posterior tuberosity.
-
Axial loading: Falls from a height are
responsible for most intraarticular fractures; they occur as the talus
is driven down into the calcaneus, which is composed of a thin cortical
shell surrounding cancellous bone. In motor vehicle accidents,
calcaneus fractures may occur when the accelerator or brake pedal
impacts the plantar aspect of the foot. -
Twisting forces may be associated with
extraarticular calcaneus fractures, in particular fractures of the
anterior and medial processes or the sustentaculum. In diabetic
patients, there is an increased incidence of tuberosity fractures from
avulsion by the Achilles tendon.
-
Patients typically present with moderate
to severe heel pain, associated with tenderness, swelling, heel
widening, and shortening. Ecchymosis around the heel extending to the
arch is highly suggestive of calcaneus fracture. Blistering may be
present and
P.425
results
from massive swelling usually within the first 36 hours after injury.
Open fractures are rare, but when present they occur medially.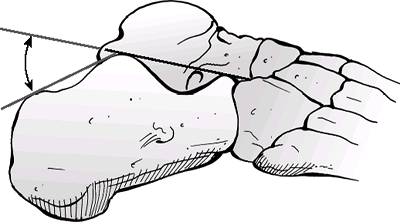 Figure 39.1. The Böhler angle.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 39.1. The Böhler angle.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Careful evaluation of soft tissues and
neurovascular status is essential. Compartment syndrome of the foot
must be ruled out, because this occurs in 10% of calcaneus fractures
and may result in clawing of the lesser toes.
-
Up to 50% of patients with calcaneus
fractures may have other associated injuries, including lumbar spine
fractures (10%) or other fractures of the lower extremities (25%);
intuitively, these injuries are more common in higher-energy injuries. -
Bilateral calcaneus fractures are present in 5% to 10% of cases.
-
The initial radiographic evaluation of
the patient with a suspected calcaneus fracture should include a
lateral view of the hindfoot, an anteroposterior (AP) view of the foot,
a Harris axial view, and an ankle series. -
Lateral radiograph
-
The Böhler tuber joint angle is composed
of a line drawn from the highest point of the anterior process of the
calcaneus to the highest point of the posterior facet and a line drawn
tangential from the posterior facet to the superior edge of the
tuberosity. The angle is normally between 20 and 40 degrees; a decrease
in this angle indicates that the weight-bearing posterior facet of the
calcaneus has collapsed, thereby shifting body weight anteriorly (Fig. 39.1). -
The Gissane (crucial) angle is formed by
two strong cortical struts extending laterally, one along the lateral
margin of the posterior facet and the other extending anterior to the
beak of the calcaneus. These cortical struts form an obtuse angle
usually between 95 and 105 degrees and are visualized directly beneath
the lateral process of the talus; an increase in this angle indicates
collapse of the posterior facet (Fig. 39.2).
-
-
AP radiograph of the foot: This may show extension of the fracture line into the calcaneocuboid joint.
-
Harris axial view
![]() Figure 39.2. Angle of Gissane.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 39.2. Angle of Gissane.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)-
This is taken with the foot in dorsiflexion and the beam angled at 45 degrees cephalad.
-
It allows visualization of the joint
surface as well as loss of height, increase in width, and angulation of
the tuberosity fragment (Fig. 39.3).
-
-
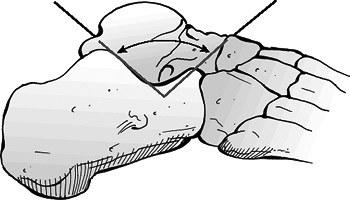
Broden views (Fig. 39.4)
-
These are obtained with the patient
supine and the x-ray cassette under the leg and the ankle. The foot is
in neutral flexion, and the leg is internally rotated 30 to 40 degrees.
The x-ray beam then is centered over the lateral malleolus, and four
radiographs are made with the tube angled 40, 30, 20, and 10 degrees
toward the head of the patient. -
These radiographs show the posterior
facet as it moves from posterior to anterior; the 10-degree view shows
the posterior portion of the facet, and the 40-degree view shows the
anterior portion. -
It is most useful intraoperatively to assess fracture reduction.
-
-
Computed tomography (CT)
-
CT images are obtained in the axial, 30-degree semicoronal, and sagittal planes.
-
Three- to 5-mm slices are necessary for adequate analysis.
-
The coronal views provide information
about the articular surface of the posterior facet, the sustentaculum,
the overall shape of the heel, and the position of the peroneal and
flexor hallucis tendons. -
The axial views reveal information about
the calcaneocuboid joint, the anteroinferior aspect of the posterior
facet, and the sustentaculum. -
Sagittal reconstruction views provide
additional information on the posterior facet, the calcaneal
tuberosity, and the anterior process.
-
-
Anterior process fractures: These may
result from strong plantar flexion and inversion, which tighten the
bifurcate and interosseous ligaments leading to avulsion fracture;
alternatively, they may occur with forefoot abduction with
calcaneocuboid compression. They are often confused with lateral ankle
sprain and are seen on lateral or lateral oblique views. Figure
Figure
39.3. Photograph of the radiographic technique for obtaining the Harris
or calcaneal radiographic view. Maximum dorsiflexion of the ankle was
attempted to obtain an optimal view.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.) -
Tuberosity fractures: These may result
from avulsion by the Achilles tendon, especially in diabetic patients
or osteoporotic women, or rarely by direct trauma; they are seen on
lateral radiographs. -
Medial process fractures: These vertical
shear fractures are due to loading of heel in valgus; they are seen on
axial radiographs. -
Sustentacular fractures: These occur with
heel loading accompanied by severe foot inversion. They are often
confused with medial ankle sprain and are seen on axial radiographs. -
Body fractures not involving the subtalar
articulation: These are caused by axial loading. Significant
comminution, widening, and loss of height may occur along with a
reduction in the Böhler angle without posterior facet involvement.
 |
|
Figure
39.4. Photograph of the technique to obtain the Broden view in an office setting. Technicians must angle the tube to allow for direct view of the posterior facet of the subtalar joint. (From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
|
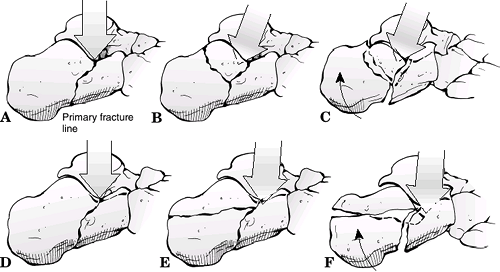
calcaneus obliquely through the posterior facet. The fracture line
exits anterolaterally at the crucial angle or as far distally as the
calcaneocuboid joint. Posteriorly, the fracture moves from plantar
medial to dorsal lateral, producing two main fragments: the
sustentacular (anteromedial) and tuberosity (posterolateral) fragments.
-
The anteromedial fragment is rarely
comminuted and remains attached to the talus by the deltoid and
interosseous talocalcaneal ligaments. -
The posterolateral fragment usually
displaces superolaterally with variable comminution, resulting in
incongruity of the posterior facet as well as heel shortening and
widening.
comminution, creating a free lateral piece of posterior facet separate
from the tuberosity fragment.
-
Tongue fracture: A secondary fracture line appears beneath the facet and exits posteriorly through the tuberosity.
-
Joint depression fracture: A secondary fracture line exits just behind the posterior facet.
-
Continued axial force causes the
sustentacular fragment to slide medially, causing heel shortening and
widening. As this occurs, the tuberosity fragment will rotate into
varus. The posterolateral aspect of the talus will force the free
lateral piece of the posterior facet down into the tuberosity fragment,
rotating it as much as 90 degrees. This causes lateral wall blowout,
which may extend as far anteriorly as the calcaneocuboid joint. As the
lateral edge of the talus collapses further, there will be additional
comminution of the articular surface.
 |
|
Figure 39.5. Mechanism of injury according to Essex Lopresti. A–C: Joint depression. D–F: Tongue.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Baltimore: Lippincott Williams & Wilkins, 2005.)
|
-
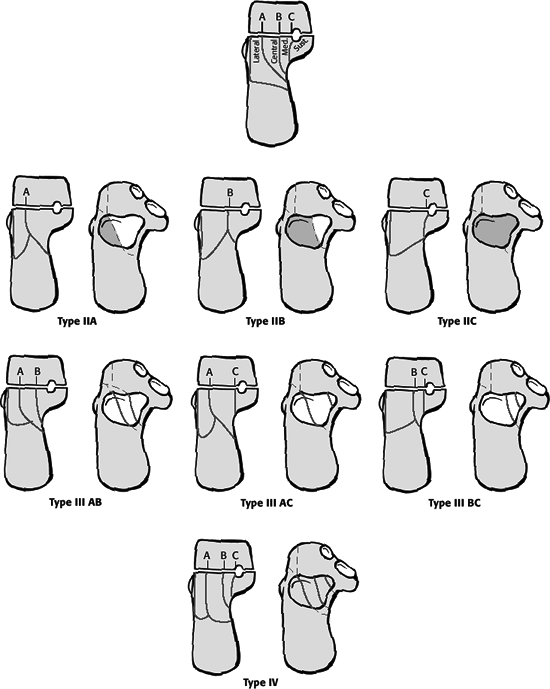
This is based on CT scans.
-
This classification is based on the
number and location of articular fragments; it is based on the coronal
image, which shows the widest surface of the inferior facet of the
talus. -
The posterior facet of the calcaneus is
divided into three fracture lines (A, B, and C, corresponding to
lateral, middle, and medial fracture lines on the coronal image). -
Thus, there can be a total of four potential pieces: lateral, central, medial, sustentaculum tali.
| Type I: | All nondisplaced fractures regardless of the number of fracture lines |
| Type II: | Two-part fractures of the posterior facet; subtypes IIA, IIB, IIC, based on the location of the primary fracture line |
| Type III: | Three-part fractures with a centrally depressed fragment; subtypes IIIAB, IIIAC, IIIBC |
| Type IV: | Four-part articular fractures; highly comminuted |
 |
|
Figure 39.6. The Sanders computed tomography scan classification of calcaneal fractures.
(From Sanders R. Current concepts review: displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am 2000;82:233.)
|
the os calcis may be severely disabling injuries, with variable
prognoses and degrees of functional debilitation with chronic pain
issues. Treatment remains controversial, with no clear indication for
operative versus nonoperative treatment.
-
Indications include:
-
Nondisplaced or minimally displaced extraarticular fractures.
-
Nondisplaced intraarticular fractures.
-
Anterior process fractures with less than 25% involvement of the calcaneal-cuboid articulation.
-
Fractures in patients with severe peripheral vascular disease or insulin-dependent diabetes.
-
Fractures in patients with other medical comorbidities prohibiting surgery.
-
Fractures associated with blistering and massive prolonged edema, large open wounds, or life-threatening injuries.
P.431 -
-
Initial treatment is placement of a bulky Jones dressing.
-
Nonoperative treatment consists of a
supportive splint to allow dissipation of the initial fracture
hematoma, followed by conversion to a prefabricated fracture boot
locked in neutral flexion to prevent an equinus contracture and an
elastic compression stocking to minimize dependent edema. -
Early subtalar and ankle joint
range-of-motion exercises are initiated, and non–weight-bearing
restrictions are maintained for approximately 10 to 12 weeks, until
radiographic union.
-
Indications
-
Displaced intraarticular fractures involving the posterior facet
-
Anterior process of the calcaneus fractures with >25% involvement of the calcaneal-cuboid articulation
-
Displaced fractures of the calcaneal tuberosity
-
Fracture-dislocations of the calcaneus
-
Selected open fractures of the calcaneus
-
-
Timing of surgery
-
Surgery should be performed within the initial 3 weeks of injury, before early fracture consolidation.
-
Surgery should not be attempted until
swelling in the foot and ankle has adequately dissipated, as indicated
by the reappearance of skin wrinkles.
-
-
Anterior process fractures (Fig. 39.7)
-
Surgical management of anterior process
fractures is performed for fractures involving >25% of the
calcaneal-cuboid articulation on CT scan evaluation. -
Definitive fixation involves small or minifragment screws.
-
The patient may ambulate in a wooden-soled shoe, but regular shoes are not permitted for 10 to 12 weeks postoperatively.
-
-
Tuberosity (avulsion) fractures
-
These result from a violent pull of the
gastrocnemius-soleus complex, such as with forced dorsiflexion
secondary to a low-energy stumble and fall, producing an avulsed
fragment of variable size. -
Indications for surgery: (1) the
posterior skin is at risk from pressure from the displaced tuberosity,
(2) the posterior portion of the bone is extremely prominent and will
affect shoe
P.432
wear,
(3) the gastrocnemius-soleus complex is incompetent, or (4) the
avulsion fragment involves the articular surface of the joint.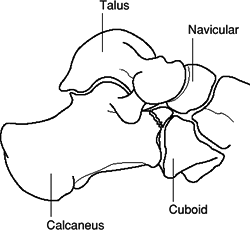 Figure 39.7. Anterior process fracture. Schematic lateral view.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
Figure 39.7. Anterior process fracture. Schematic lateral view.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.) -
Surgical treatment involves lag screw fixation with or without cerclage wire.
-
-
Calcaneus body fractures
-
True extraarticular fractures of the
calcaneus, not involving the subtalar joint, probably account for 20%
of all calcaneal fractures. -
Minimally displaced fractures (<1 cm) are treated with early motion and non–weight bearing for 10 to 12 weeks.
-
Those with significant displacement
resulting in varus/valgus deformity, lateral impingement, loss of heel
height, or translation of the posterior tuberosity require open
reduction and internal fixation.
-
-
Medial or lateral process fractures
-
Rare and usually nondisplaced.
-
The fracture is best seen on the axial radiographic view or on coronal CT scans.
-
Nondisplaced fractures can be treated with a short leg weight-bearing cast until the fracture heals at 8 to 10 weeks.
-
When fractures are displaced, closed manipulation may be considered.
-
operative to nonoperative treatment of displaced intraarticular
calcaneal fractures found the following:
-
Significantly better results occurred in certain fracture groups undergoing operative treatment
-
Those having nonoperative treatment of
their fracture were 5.5 times more likely to require a subtalar
arthrodesis for posttraumatic arthritis than those undergoing operation. -
Operative goals include:
-
Restoration of congruity of the subtalar articulation.
-
Restoration of the Böhler angle.
-
Restoration of the normal width and height of the calcaneus.
-
Maintenance of the normal calcaneocuboid articulation.
-
Neutralization of the varus deformity of the fracture.
-
-
Open reduction and internal fixation are
generally performed through a lateral L-shaped incision, with care
taken not to damage the sural nerve both proximally and distally. -
The posterior facet is reduced and
stabilized with lag screws into the sustentaculum tali. The
calcaneocuboid joint and the lateral wall are reduced. The length of
the heel is regained with neutralization of varus. A thin plate is
placed laterally and is used as a buttress with possible bone grafting
to restore bone stock. -
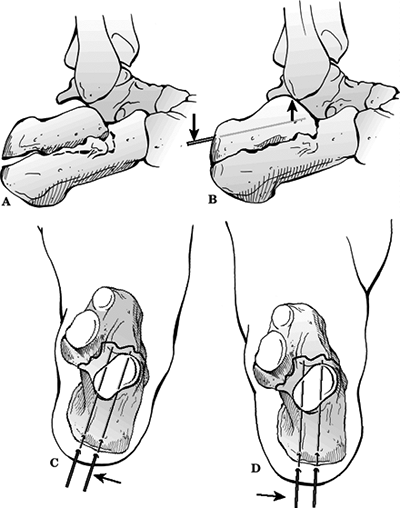
Good results have been reported for
tongue-type fractures using percutaneous reduction (Essex-Lopresti
maneuver) and lag screw fixation (Fig. 39.8). -
Primary subtalar or triple arthrodesis has had good reported results for select high-energy injuries.
-
Postoperative management includes:
-
Early supervised subtalar range-of-motion exercises.
-
Non–weight bearing for 8 to 12 weeks.
-
Full weight bearing by 3 months.
-
-
Wound dehiscence: Most common at the
angle of incision. Avoidance requires meticulous soft tissue technique
and minimization of skin trauma during closure. It may be treated with
wet to dry dressing changes, skin grafting, or muscle flap if necessary. -
Calcaneal osteomyelitis: The risk may be minimized by allowing soft tissue edema to resolve preoperatively.
-
Posttraumatic arthritis (subtalar or
calcaneocuboid): This reflects articular damage in addition to fracture
displacement and comminution; thus, it may occur even in the presence
of an anatomic reduction; it may be treated with injections or
orthoses, or it may ultimately require subtalar or triple arthrodesis. -
Increased heel width: Some degree of heel
widening is expected, even with open reduction and internal fixation.
It may result in lateral impingement on the peroneal tendons or the
fibula. It is aggravated by increased residual lateral width and may be
treated by wall resection or hardware removal. -
Loss of subtalar motion: This is common with both operative and nonoperative treatment of intraarticular fractures.
-
Peroneal tendonitis: This is generally seen following nonoperative treatment and results from lateral impingement.
-
Sural nerve injury: This may occur in up to 15% of operative cases using a lateral approach.
![]() Figure
Figure
39.8. (A–D) Essex-Lopresti technique as modified by Tornetta. Once
guide pins are correctly positioned, they are exchanged for 6.5- to
8.0-mm cannulated cancellous lag screws.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Chronic pain: Despite nonoperative or
operative treatment of calcaneal fractures, many patients have chronic
heel pain that may be debilitating; many individuals are unable to
return to gainful employment. -
Reflex sympathetic dystrophy: This may occur with operative or nonoperative management.