Tibial Plateau Fracture
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Tibial Plateau Fracture
Tibial Plateau Fracture
Peter R. Jay MD
Jason W. Hammond MD
Description
-
The tibial plateau is the proximal weightbearing surface of the tibia.
-
Articulates with the femoral condyles to form the knee joint
-
Can be divided into medial and lateral components
-
-
A tibial plateau fracture is any fracture involving the proximal articular surface of the tibia (Fig. 1).
-
Classification by Schatzker et al. (1):
-
Type I: Lateral split fracture
-
Type II: Lateral split/depression fracture
-
Type III: Central depression fracture
-
Type IV:
-
Medial plateau fracture (with or without intercondylar spine involvement)
-
Represents a fracture dislocation and has the highest concurrence of vascular or neurologic injury
-
-
Type V: Combined medial and lateral plateau fracture
-
Type VI:
-
Fracture of the metaphysis separating the articular portion of the fracture from the tibial shaft
-
Often the result of high-impact trauma,
so associated abdominal, thoracic, pelvic, spinal, skeletal, or cranial
injury may be present.
-
-
-
Neurovascular injury and compartment
syndrome may occur with any tibial plateau fracture, but they are more
common with high-energy injuries (type IV, V, and VI fractures).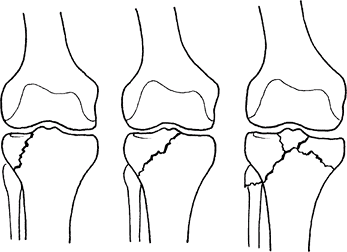 Fig. 1. Tibial plateau fracture may involve 1 or both sides of the joint.
Fig. 1. Tibial plateau fracture may involve 1 or both sides of the joint. -
Associated soft-tissue injuries to the knee are likely.
-
Involvement of these structures may be as
high as 77% for 1 or more cruciate or collateral ligaments, 91% for
lateral meniscus abnormality, 44% for medial meniscus tears, and 68%
for tears of 1 or more of the posterolateral corner structures of the
knee (2).
-
Epidemiology
Incidence
-
Tibial plateau fractures comprise 1% of all fractures and 8% of fractures in elderly persons (3).
-
Fractures in the elderly usually result from a low-energy fall (4).
-
-
Isolated medial plateau fractures comprise ~10–23% of these injuries (1,5).
-
Isolated lateral plateau fractures comprise ~55–70% of these injuries (1,5).
-
Combined medial and lateral plateau fractures comprise ~11–31% of these injuries (1).
Risk Factors
-
Those at risk for high-velocity trauma (e.g., young age, male gender, alcohol and drug abuse, urban environment)
-
The elderly with poor bone quality are at risk for fractures from falls.
Etiology
-
Isolated varus, valgus, or axial force, or a combination thereof
-
Most fractures are the result of motor vehicle accidents, pedestrian versus motor vehicle accidents, and falls from a height.
-
Less frequently, fractures are caused by a skiing or bicycle accident, or other sports injury.
Signs and Symptoms
-
Pain, swelling, and often deformity
-
Inability to bear any or full weight
-
Inability to move the knee partially or fully
Physical Exam
-
The patient requires a complete trauma evaluation.
-
Special care must be taken to evaluate the skin and subcutaneous tissue (open versus closed, and tissue quality).
-
Perform a careful neurologic examination for nerve injury (most often peroneal).
-
Perform a careful vascular examination.
-
If pulses are not equal, the arterial
brachial index should be measured and, if abnormalities are found, a
vascular surgeon should be consulted urgently. -
Arteriogram and revascularization may be required.
-
-
Patients must be examined for compartment syndrome.
-
Varus and valgus stability can be assessed gently, and pseudolaxity may be determined.
Tests
Imaging
-
Radiography:
-
High-quality AP and lateral radiographs are used to identify the fracture lines and estimate displacement.
-
Oblique radiographs may be helpful in assessing fracture lines.
-
-
CT:
-
This important adjunctive study to plain radiographs influences decision-making.
-
Obtain scout views to ensure the images are tangent to the articular surface; cuts of ≤5 mm are recommended.
-
Helps plan surgery and assess the articular surface of the joint
-
-
MRI:
-
Useful in identifying soft-tissue injury, including ligamentous and meniscal injury
-
Also useful for diagnosing nondisplaced fractures
-
Differential Diagnosis
-
Femur fracture
-
Supracondylar fracture
-
Femoral condylar fracture
-
Tibia metaphyseal injury
-
High tibial shaft injury
-
Soft-tissue injuries, such as of the ACL, OSD, LCL, MCL, meniscus, or any combination thereof
P.457
General Measures
-
Ice, elevation, and immobilization should be initiated as early as possible.
-
A large, bulky dressing with plaster and splints or a well-padded knee immobilizer is used to prevent excessive swelling.
-
Nondisplaced fractures may be treated
without surgery, but they should be immobilized initially and then
placed in a hinged knee brace.
Activity
Regardless of treatment, patients should not bear weight until the fracture is healed.
Special Therapy
Physical Therapy
ROM and quadriceps strengthening exercises are performed until full ROM is achieved.
Medication
First Line
Opioid analgesics usually are required for pain control.
Surgery
-
Indications:
-
Open fracture
-
Intra-articular step-off of >3–5 mm or tilt of a condyle of >5°
-
Varus or valgus angulation of the extended knee
-
Floating knee (fracture of the tibia and femur, the knee floats in between)
-
-
Types of fixation:
-
External fixation:
-
Bridging: The PINS are placed in the
distal femur and midtibia to immobilize the knee and stabilize the
fracture while the soft tissues heal (temporary fixation). -
Hybrid frame: The tensioned wires are
placed just below the tibial articular surface and standard 5-mm PINS
are placed in the tibial diaphysis, providing stabilization of the
fracture fragments (open definitive fixation).
-
-
Internal fixation:
-
Elevate depressed parts of the joint.
-
Use bone graft or bone substitutes to maintain elevation of articular surface.
-
-
Limited percutaneous fixation:
-
Use cannulated screws and fluoroscopy.
-
Can be combined with limited reduction and elevation of the joint surface
-
Can be combined with external fixation
-
Can be performed with arthroscopic assistance
-
-
Plating:
-
Buttress plating: Medial or lateral
plates, depending on the type of fracture; use of a raft of subchondral
screws to support the articular surface -
Contoured locking plates: Available to
fit the lateral side of the proximal tibia precisely; screws lock into
the plate to add support; may be used to support bicondylar fractures -
Double plating: Must be done carefully to prevent soft-tissue stripping, the “dead bone sandwich”
-
-
Combined external/internal fixation:
-
Initial bridging external fixation followed by delayed plating
-
Allows for rest and healing of the soft-tissue envelope
-
Favored in high-energy injuries
-
-
Arthroscopic-assisted fixation:
-
Allows for diagnosis of intra-articular abnormality
-
Direct visualization of joint step-off
-
Care must be taken to avoid fluid extravasation and compartment syndrome.
-
-
Weightbearing is delayed usually until fracture is healed clinically.
-
With adequate stabilization, surgically treated knees should start early ROM exercises.
-
Prognosis
-
These fractures can be devastating injuries.
-
The incidence of posttraumatic arthritis
is related to the age of the patient, amount and location of initial
displacement, and reduction of the fracture (6). -
In 1 series, high-energy fractures
treated with a staged approach with initial external fixation had only
a 5% incidence of wound problems (7). -
Patients with high-energy fractures of
the tibial plateau treated with external fixation have been shown to
have 5-year knee scores comparable to those of age-matched controls (8).
Complications
-
Skin compromise
-
Infection
-
Compartment syndrome may occur in as many as 10% of plateau fractures (9).
-
Loss of fixation
-
Malunion
-
Nonunion
-
Posttraumatic arthritis
-
Stiffness
-
Pain
Patient Monitoring
After fracture fixation, patients should be monitored with monthly radiographs until fracture healing.
References
1. Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience, 1968–1975. Clin Orthop Relat Res 1979;138:94–104.
2. Gardner
MJ, Yacoubian S, Geller D, et al. The incidence of soft tissue injury
in operative tibial plateau fractures: A magnetic resonance imaging
analysis of 103 patients. J Orthop Trauma 2005;19:79–84.
MJ, Yacoubian S, Geller D, et al. The incidence of soft tissue injury
in operative tibial plateau fractures: A magnetic resonance imaging
analysis of 103 patients. J Orthop Trauma 2005;19:79–84.
3. Singer BR, McLauchlan GJ, Robinson CM, et al. Epidemiology of fractures in 15,000 adults: The influence of age and gender. J Bone Joint Surg 1998;80B:243–248.
4. Keating JF. Tibial plateau fractures in the older patient. Bull Hosp Jt Dis 1999;58:19–23.
5. Berkson EM, Virkus WW. High-energy tibial plateau fractures. J Am Acad Orthop Surg 2006;14:20–31.
6. Gaston P, Will EM, Keating JF. Recovery of knee function following fracture of the tibial plateau. J Bone Joint Surg 2005;87B:1233–1236.
7. Egol
KA, Tejwani NC, Capla EL, et al. Staged management of high-energy
proximal tibia fractures (OTA types 41): The results of a prospective,
standardized protocol. J Orthop Trauma 2005;19:448–455.
KA, Tejwani NC, Capla EL, et al. Staged management of high-energy
proximal tibia fractures (OTA types 41): The results of a prospective,
standardized protocol. J Orthop Trauma 2005;19:448–455.
8. Weigel DP, Marsh JL. High-energy fractures of the tibial plateau. Knee function after longer follow-up. J Bone Joint Surg 2002;84A:1541–1551.
9. Chang
YH, Tu YK, Yeh WL, et al. Tibial plateau fracture with compartment
syndrome: a complication of higher incidence in Taiwan. Chang Gung Med J 2000;23:149–154.
YH, Tu YK, Yeh WL, et al. Tibial plateau fracture with compartment
syndrome: a complication of higher incidence in Taiwan. Chang Gung Med J 2000;23:149–154.
Codes
ICD9-CM
832.00 Tibial plateau fracture
Patient Teaching
Compliance with motion and weightbearing status is essential for a good outcome.
Activity
-
Patients should begin ROM exercises of the knee as soon as possible.
-
Weightbearing should be delayed until the fracture is healed.
FAQ
Q: Which patients are at risk of compartment syndrome after tibial plateau fracture?
A: All patients are at risk. Patients with high-energy fractures and those with coagulopathies are at highest risk.
Q: Which patients are at highest risk of vascular injury?
A: Patients with high-energy fractures and fractures of the medial condyle (type IV fractures) are at highest risk.
