Meniscus Tear
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Meniscus Tear
Meniscus Tear
Carl Wierks MD
Bill Hobbs MD
Description
-
A meniscus tear is an acute or degenerative injury to the meniscal fibrocartilage of the knee (Fig. 1).
-
Classification:
-
Acute tear:
-
Longitudinal (50–90%)
-
Radial (6%)
-
Flap (4%)
-
-
Degenerative tear:
-
Mostly horizontal cleavage or complex tears
-
-
Epidemiology
-
Acute tears occur mainly in adolescents and young adults, and degenerative tears predominate in the 40–60-year-old population.
-
Degenerative medial tears occur more frequently than do degenerative lateral meniscal tears (1).
-
Acute lateral meniscus tears occur more frequently than do acute medial tears (2).
Incidence
-
In 1 study of asymptomatic individuals,
MRI showed that 13% of those <45 years old and 36% of those >45
years old had a meniscus tear (3). -
Another study showed that 60% of cadavers aged 65 years at time of death had degenerative tears (4).
-
Concomitant ACL tear occurs in ~30% of patients with acute meniscus tears (1).
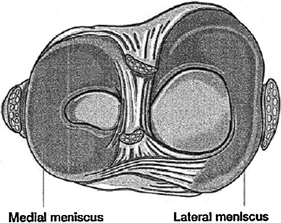 Fig.
Fig.
1. Artist’s sketch of a meniscal tear in the right knee. (From: Sports
Tips: “Meniscal tears in athletes.” Used with permission of the
American Orthopaedic Society for Sports Medicine, Rosemont, IL.)
Risk Factors
-
Twisting, hyperflexion injury
-
Age >40 years
-
Chronic ACL deficiency
-
Tibial plateau fracture
-
Arthritis affecting the knee
Genetics
No Mendelian inheritance is known.
Etiology
-
Acute:
-
Often occurs during athletic activities, most commonly football, basketball, and wrestling
-
A common mechanism is a severe twisting at the knee, often during change of direction.
-
Can be associated with ACL injury
-
-
Degenerative:
-
Age-related breakdown of collagen fibers
-
Associated Conditions
Ligamentous injury (ACL, collateral ligament) in acute tears
Signs and Symptoms
-
Acute pain and swelling
-
Tenderness localized to the joint line or popliteal region with the knee flexed
-
Popping, locking, catching, or buckling with large, unstable the tears
-
Inability of the patient to extend the knee fully in the presence of a displaced bucket-handle tear
-
May have chronic mild swelling and joint-line pain in the presence of a degenerative tear
History
-
Acute twisting of the knee while weightbearing
-
Chronic knee pain
Physical Exam
-
Assess knee stability.
-
Joint-line tenderness is the best clinical sign (74% sensitivity, 50% positive predictive value) (5).
-
McMurray test:
-
Hyperflex the knee and gently rotate it internally and externally, applying valgus and varus stress while extending the knee.
-
May feel click, pop, or crepitance
-
Reproduces patient symptoms
-
-
Apley grind test:
-
Position the patient prone.
-
Internally and externally rotate the leg with traction and compression.
-
Pain or mechanical symptoms indicate likely meniscal pathology.
-
Tests
Imaging
-
Plain radiographs: 30° flexed posteroanterior view is best for observing weightbearing surfaces.
-
MRI is 90–98% accurate, although it can give false-positive results (6).
Diagnostic Procedures/Surgery
Arthroscopy is the gold standard for diagnosis.
Pathological Findings
-
Collagen fibers:
-
Oriented circumferentially
-
Resistant to compressive forces
-
May tear under shear stress
-
-
Tears in inner 2/3 heal poorly because of the lack of blood supply.
-
Degeneration from repeated microtrauma occurs, with gradual loss of collagen and integrity that leads to tears.
Differential Diagnosis
-
Chondral lesion
-
ACL or collateral ligament tear
-
Fibrotic plica
-
Fat-pad impingement
-
Osteoarthritis
-
Patellofemoral chondrosis
-
Spontaneous osteonecrosis
P.253
General Measures
-
Begin with a trial of rest, protected weightbearing, and modified activity.
-
If the patient remains symptomatic, offer MRI or arthroscopic evaluation.
Activity
-
Weightbearing as tolerated
-
Often return to full activities 2–3 weeks after injury
Medication
Drugs of choice are analgesics or NSAIDs.
Surgery
-
Indications for arthroscopy:
-
Symptoms that affect activities of daily living or work, mechanical symptoms
-
Positive physical findings (joint tenderness, effusion)
-
Failure of nonsurgical treatment
-
-
The following lesions should be repaired:
-
Complete vertical tear >10 mm long
-
Tear within the peripheral 10–30% of the meniscus or 3–4 mm of the meniscocapsular junction
-
-
Better healing of meniscal repairs with concurrent ACL reconstruction
-
Complex tears and those in the avascular inner 2/3 are resected.
-
Total meniscectomy is not recommended because of the increased risk of degenerative arthritis.
-
Initiate gradual strengthening and ROM program.
-
Return to full activities 6–8 weeks after partial meniscectomy
Complications
-
Complications are uncommon but include:
-
Injury to neurovascular structures (infrapatellar branch of saphenous nerve, causing pain, dysesthesias at the portal site)
-
Infection
-
DVT
-
Arthritis
-
References
1. Poehling GG, Ruch DS, Chabon SJ. The landscape of meniscal injuries. Clin Sports Med 1990;9: 539–549.
2. Baker BE, Peckham AC, Pupparo F, et al. Review of meniscal injury and associated sports. Am J Sports Med 1985;13:1–4.
3. LaPrade
RF, Burnett QM, II, Veenstra MA, et al. The prevalence of abnormal
magnetic resonance imaging findings in asymptomatic knees. With
correlation of magnetic resonance imaging to arthroscopic findings in
symptomatic knees. Am J Sports Med 1994;22:739–745.
RF, Burnett QM, II, Veenstra MA, et al. The prevalence of abnormal
magnetic resonance imaging findings in asymptomatic knees. With
correlation of magnetic resonance imaging to arthroscopic findings in
symptomatic knees. Am J Sports Med 1994;22:739–745.
4. Noble J, Hamblen DL. The pathology of the degenerate meniscus lesion. J Bone Joint Surg 1975;57B:180–186.
5. Anderson AF, Lipscomb AB. Clinical diagnosis of meniscal tears. Description of a new manipulative test. Am J Sports Med 1986;14:291–293.
6. De
Smet AA, Norris MA, Yandow DR, et al. MR diagnosis of meniscal tears of
the knee: importance of high signal in the meniscus that extends to the
surface. AJR Am J Roentgenol 1993;161:101–107.
Smet AA, Norris MA, Yandow DR, et al. MR diagnosis of meniscal tears of
the knee: importance of high signal in the meniscus that extends to the
surface. AJR Am J Roentgenol 1993;161:101–107.
Additional Reading
Andrish JT. Meniscal injuries in children and adolescents: diagnosis and management. J Am Acad Orthop Surg 1996;4:231–237.
Greis PE, Holmstrom MC, Bardana DD, et al. Meniscal injury: II. Management. J Am Acad Orthop Surg 2002;10:177–187.
Greis PE, Bardana DD, Holmstrom MC, et al. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg 2002;10:168–176.
Hardin GT, Farr J, Bach BR, Jr. Meniscal tears: diagnosis, evaluation, and treatment. Orthop Rev 1992;21:1311–1317.
Phillips BB. Arthroscopy of lower extremity. In: Canale ST, ed. Campbell’s Operative Orthopaedics, 10th ed. St. Louis: Mosby, 2003:2515–2612.
Urquhart
MW, O’Leary JA, Giffin JR, et al. Knee. Section D. Meniscal injuries.
1. Meniscal injuries in the adult. In: DeLee JC, Drez D, Jr, Miller MD,
eds. DeLee & Drez’s Orthopaedic Sports Medicine: Principles and Practice, 2nd ed. Philadelphia: WB Saunders, 2003:1668–1686.
MW, O’Leary JA, Giffin JR, et al. Knee. Section D. Meniscal injuries.
1. Meniscal injuries in the adult. In: DeLee JC, Drez D, Jr, Miller MD,
eds. DeLee & Drez’s Orthopaedic Sports Medicine: Principles and Practice, 2nd ed. Philadelphia: WB Saunders, 2003:1668–1686.
Weiss CB, Lundberg M, Hamberg P, et al. Non-operative treatment of meniscal tears. J Bone Joint Surg 1989;71A:811–822.
Codes
ICD9-CM
836.2 Meniscus tear
FAQ
Q: When can I walk after an arthroscopic meniscectomy?
A: For an isolated arthroscopic partial meniscectomy, weightbearing as tolerated can begin almost immediately.
Q: What decides if a meniscus tear is repaired?
A:
The decision is based on the capacity to heal, i.e., the presence of a
blood supply. Acute tears, near the periphery, usually are repaired.
Less peripheral and degenerative tears are resected.
The decision is based on the capacity to heal, i.e., the presence of a
blood supply. Acute tears, near the periphery, usually are repaired.
Less peripheral and degenerative tears are resected.
