Medial Collateral Ligament Injury
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Medial Collateral Ligament Injury
Medial Collateral Ligament Injury
John H. Wilckens MD
Marc Urquhart MD
Description
-
An MCL injury is a sprain of the MCL, which is the primary restraint to valgus stress on the knee.
-
It occurs mainly in athletic teenagers and young adults, and equally among males and females.
-
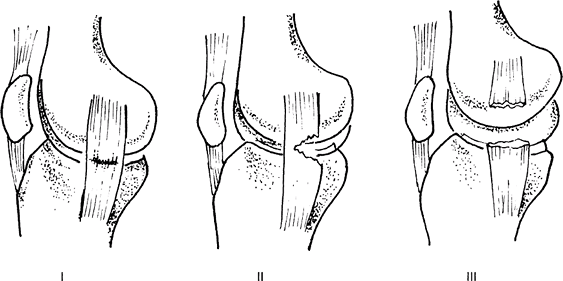
Classification (Fig. 1) (1):
-
Grade I (mild): Microscopic sprain with intact fibers
-
Grade II (moderate): Partial tear
-
Grade III (severe): Complete tear
-
General Prevention
Prevention is best accomplished through conditioning before sport activities.
Risk Factors
-
Contact sports
-
Falls
Etiology
-
Direct blow to the lateral knee
-
Valgus load to the knee
Associated Conditions
ACL injuries via a noncontact mechanism
 |
|
Fig. 1. MCL injuries may be graded as follows: I, microscopic strain; II, partial tear; or III, complete tear.
|
Signs and Symptoms
-
Pain along the medial aspect of the knee, typically extending proximally and distally along the course of the MCL
-
Possible knee effusion
-
Can be associated with an ACL tear and/or a meniscus tear
-
Increased pain with valgus loading
-
Occasionally, recollection by patient of a “pop” or “snap” at the time of the injury
History
-
Occurs most commonly with a direct blow to the lateral knee, causing the knee to gap open
-
If MCL injury occurs with a noncontact mechanism, a high association with ACL injury exists.
Physical Exam
-
MCL ruptures can be associated with other injuries; physical examination and diagnostic workup should reflect a high suspicion.
-
Test the stability of the MCL:
-
Flex the patient’s knee 30° and apply a valgus force
-
Estimate degree of opening and character of the end point (soft, solid).
-
Valgus laxity of the knee in 0° of flexion suggests an MCL injury in addition to a cruciate ligament injury.
-
-
Perform a complete neurovascular examination distal to the knee.
-
Perform the Lachman and posterior drawer tests to rule out associated ACL or PCL injury.
-
Compare with the contralateral knee.
Tests
Imaging
-
AP and lateral plain radiographs should be obtained initially to rule out fractures.
-
MRI is an appropriate study because of its sensitivity to other ligamentous or meniscal disease.
Differential Diagnosis
-
ACL rupture
-
Medial meniscal tears
-
OSD rupture
-
Tibial plateau fractures
-
Tibial spine avulsions
-
Patella dislocation
P.251
General Measures
-
Initially, a patient with an MCL injury
is treated with ice, elevation, analgesics, a hinged knee brace, and
protected weightbearing as tolerated. -
The patient should be referred to physical therapy.
-
If the patient has a suspicion for an
associated cruciate ligament injury, early referral to an orthopaedic
surgeon is indicated.
Special Therapy
Physical Therapy
-
Gentle ROM exercises
-
Muscle-strengthening program with emphasis on medial hamstrings (MCL agonists) and core muscles
-
Progressive weightbearing in hinged knee brace as tolerated
-
Ice, electrical stimulation (2)
-
Once pain free, progressive agility and proprioception training
Surgery
Chronic MCL tears unresponsive to nonoperative treatment may require surgical repair.
Prognosis
-
Most patients with MCL injuries respond to nonoperative treatment (bracing and early ROM).
-
Bracing should be considered for patients returning to contact sports.
Patient Monitoring (3,4)
-
Patients are followed at 2–6 weeks to check ROM, muscle strength, and joint laxity.
-
MRI if examination suggests associated cruciate ligament and/or meniscal injuries.
References
1. O’Donoghue DH. Treatment of acute ligamentous injuries of the knee. Orthop Clin North Am 1973;4:617–645.
2. Wilk KE, Andrews Jr, Clancy WG. Nonoperative and postoperative rehabilitation of the collateral ligaments of the knee. Oper Tech Sports Med 1996;4:192–201.
3. Bergfeld
J. Symposium: functional rehabilitation of isolated medial collateral
ligament sprains. First-, second-, and third-degree sprains. Am J Sports Med 1979;7:207–209.
J. Symposium: functional rehabilitation of isolated medial collateral
ligament sprains. First-, second-, and third-degree sprains. Am J Sports Med 1979;7:207–209.
4. Inoue
M, McGurk-Burleson E, Hollis JM, et al. Treatment of the medial
collateral ligament injury. I: The importance of anterior cruciate
ligament on the varus-valgus knee laxity. Am J Sports Med 1987;15:15–21.
M, McGurk-Burleson E, Hollis JM, et al. Treatment of the medial
collateral ligament injury. I: The importance of anterior cruciate
ligament on the varus-valgus knee laxity. Am J Sports Med 1987;15:15–21.
Additional Reading
Indelicato
PA, Hermansdorfer J, Huegel M. Nonoperative management of complete
tears of the MCL of the knee in intercollegiate football players. Clin Orthop Relat Res 1990;256:174–177.
PA, Hermansdorfer J, Huegel M. Nonoperative management of complete
tears of the MCL of the knee in intercollegiate football players. Clin Orthop Relat Res 1990;256:174–177.
Shelbourne KD, Nitz PA. The O’Donoghue triad revisited. Combined knee injuries involving anterior cruciate and MCL tears. Am J Sports Med 1991;19:474–477.
Codes
ICD9-CM
844.1 Medial collateral ligament
Patient Teaching
-
Most MCL injuries heal without surgery.
-
Patients are instructed in ROM and muscle-strengthening exercises.
FAQ
Q: How can you tell if someone has had an associated injury with the MCL sprain?
A:
An MCL injury sustained via a noncontact incident, with a large
effusion, or with valgus laxity in full extension suggests that another
structure (commonly the ACL) has been injured.
An MCL injury sustained via a noncontact incident, with a large
effusion, or with valgus laxity in full extension suggests that another
structure (commonly the ACL) has been injured.
