Continuous Sciatic Blocks
Anesthesia and postoperative analgesia for total knee arthroplasty;
above and below the knee amputation; popliteal fossa surgery (e.g.,
tumors, cysts); cancer surgery of the lower limb; and major leg, ankle,
and foot surgery with a thigh tourniquet.
A 15 to 20 mL ropivacaine 0.75% bolus followed by an infusion of 7
mL/hour or a patient-controlled analgesia (PCA) ropivacaine 0.2% with a
basal rate of 5 mL/hour, bolus 5 mL, lockout time 45 minutes.
An 18-gauge, 100-mm plastic introducing cannula with a stimulating
short beveled stylet or insulated Tuohy needle and a 20- or 21-gauge
catheter.
The posterior superior iliac spine (PSIS) and the ischial tuberosity
(IT). With this approach, the sciatic nerve is approached at the level
of the greater sciatic foramen, where it leaves the pelvis with the
pelvic fascia medial, piriformis muscle posterior, and obturator
internus muscle lateral.
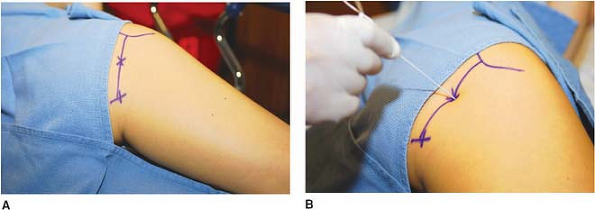
A line is drawn between the PSIS and the lowest point of the IT. The
site of needle insertion is three fingerbreadths caudal to the PSIS on
the PSIS–IT line. The insulated Tuohy needle with the bevel oriented
laterally, connected to a nerve stimulator (2.0 mA, 2 Hz, 0.1 ms) is
introduced perpendicularly at a 10° caudal and lateral angle (Fig. 29-1).
The position of the needle is adjusted to produce a motor response
corresponding to a stimulation of the sciatic nerve, either the common
peroneal nerve (inversion of the foot or dorsiflexion of the foot and
toes) or the tibial nerve (eversion of the foot or plantar flexion of
the foot and toes) with a current less than 0.5 mA. After negative
aspiration for blood, local anesthetic is slowly injected with repeated
aspiration for
blood.
The catheter is introduced 3 to 5 cm beyond the needle tip. The
introducer needle is removed, and the catheter is secured in place with
Steri-Strip (3M, St. Paul, MN) and covered with a transparent dressing.
 |
|
Figure 29-1. The insulated Tuohy needle connected to a nerve stimulator is introduced perpendicularly.
|
-
The site of the introduction of the needle is just below the PSIS.
-
A motor response at the level of the hip
or thigh should not be considered sufficient because it can be produced
by direct muscle stimulation or can correspond to a nerve stimulation
of the piriformis or the obturator internus muscle (needle too
lateral). Conversely, a stimulation of the obturator nerve (adduction
of the thigh) indicates that the needle is too anterior and medial.
Finally, a gluteal muscle contraction indicates that the position of
the needle is too superficial. -
In case of bony contact (sacral or iliac
bone, near the sacroiliac joint, at the top of the greater sciatic
notch), the needle needs to be withdrawn and reintroduced more caudally
on the PSIS–IT line. The depth at which the bone was contacted is an
important indicator. Since the nerve is approached on the top of the
greater sciatic foramen, where the sciatic nerve leaves the pelvis, the
needle tip should be introduced no more than an additional 20 mm. -
This block is often associated with a
block of the obturator nerve (>90%) because of the anatomic
proximity of the sacral plexus and the obturator nerve. An extension of
the block to the pudendal plexus is also possible, especially to the
pudendal nerve (up to 80%). This explains the associated unilateral
anesthesia of the perineum. Finally, the proximity of the pelvic
splanchnic nerves and the terminal branches of the sympathetic trunks
and the inferior hypogastric plexus may explain associated urinary
retention. -
Although no specific serious
complications have been reported with this technique, caution should be
exercised to avoid damaging the pelvic vessels and organs because of
the proximity of the sacral plexus and the pelvic vessels and organs. -
In the recovery room, a radiograph may be
performed after injection of a contrast agent to verify the position of
the parasacral catheter. -
This is the only approach to the sciatic
nerve that allows consistent blocking of the tibial, common peroneal,
and posterior cutaneous nerves of the thigh and also the superior and
inferior gluteal nerves and the quadratus femoris nerve. -
Compared with a single parasacral block,
the Tuohy needle is oriented caudally and laterally to facilitate the
placement of the catheter.
P, Ripart J, Jeannes P, et al. Comparison of the parasacral approach
and the posterior approach, with single- and double-injection
techniques, to block the sciatic nerve. Anesthesiology 2003;98(6):1436–1441.
NY, Bennetts FE. An observational study of combined continuous lumbar
plexus and single shot sciatic nerve blocks for post-knee surgery
analgesia. Reg Anesth 1996;21:287–291.
15 to 20 mL of 0.5% ropivacaine followed by either a continuous
infusion of 6 to 10 mL/hour or a PCA with a basal infusion rate of 5
mL/hour, bolus of 5 mL, and a 30-minute lockout time 0.2% ropivacaine.
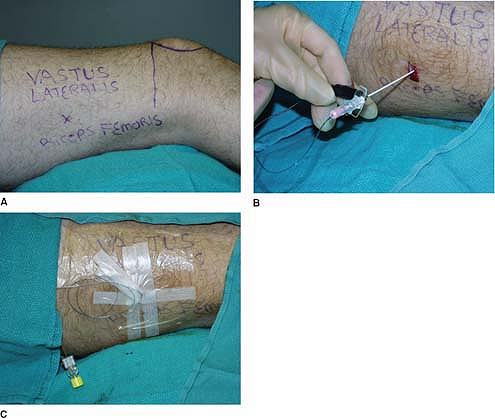
The greater trochanter and the ischial tuberosity (IT). At the level of
the thigh, the sciatic nerve runs toward the popliteal fossa (sciatic
line), lying on the posterior surface of the adductor magnus, within
the posterior medial compartment of the thigh. The septum
intermusculare femoralis mediale and a reinforcement of the posterior
fascia of the adductor magnus muscle limit this compartment.
The greater trochanter and the IT are identified and marked, and a line
is drawn between these two points. The site of introduction of the
needle is the midpoint (Fig. 29-2A).
At this level, a skin depression can be palpated, representing the
groove between the biceps femoris and semi-tendinous muscles. After
proper local skin infiltration, the Tuohy needle with the tip oriented
cephalad and connected to a nerve stimulator (1.5 mA, 2 Hz, 0.1 ms) is
introduced through the skin at a 90° angle (Fig. 29-2B).
The Tuohy needle is advanced until the sciatic nerve is stimulated with
either an eversion of the foot or dorsiflexion of the foot and
extension of the toes
(common
peroneal nerve) or an inversion or plantar flexion of the foot and toes
(tibial nerve). The needle position is adjusted to maintain the same
motor response with a current 0.5 mA. After negative aspiration for
blood, 15 to 20 mL of local anesthetic solution is slowly injected with
repeat aspiration for blood every 5 mL. A 20-gauge catheter is
introduced through the Tuohy needle no more than 3 to 4 cm beyond the
needle tip. Finally, the needle is removed, and the catheter is secured
with Steri-Strip and covered with a transparent dressing.
 |
|
Figure 29-2. A: Landmark; B: Placement of the needle.
|
-
The gluteal approaches, as compared with
other sciatic approaches (classic posterior approach of Labat, high
lateral, mediofemoral), reduces the risk for vascular puncture and
reduces the risk for misplacement or dislocation of the catheter after
surgery. -
This block is usually performed in
combination with a single lumbar, femoral, or saphenous block to
satisfy the surgical and tourniquet requirements. Less frequently, a
combination of a gluteal continuous block and a continuous lumbar
plexus or femoral block is indicated (anterior cruciate ligament [ACL]
involving the use of hamstring graft) for postoperative analgesia. -
This approach is also particularly helpful in obese patients.
-
Furthermore, compared with the classic
posterior approach of Labat, this approach is mostly painless because
the needle is introduced into the groove between the biceps femoris and
semi-tendinous muscles. -
With this approach, the catheter can be easily maintained in place with minimal risk for dislocations.
-
If the femur is contacted, the needle needs to be withdrawn and redirected medially.
Benedetto P, Casati A, Bertini L. Continuous subgluteus sciatic nerve
block after orthopedic foot and ankle surgery: comparison of two
infusion techniques. Reg Anesth Pain Med 2002;27:168–172.
Benedetto P, Casati A, Bertini L, et al. Postoperative analgesia with
continuous sciatic nerve block after foot surgery: a prospective,
randomized comparison between the popliteal and subgluteal approaches. Anesth Analg 2002;94:996–1000.
 |
|
Figure 29-3. A: Landmark; B: Placement of the needle and catheter; C: Dressing.
|
The leg is rotated slightly medially. Next, the groove between the
biceps femoris and the vastus lateralis muscles is identified and
marked (groove line). A vertical line is drawn from the top of the
patella (patella line). The site of needle insertion is located 10 cm
cephalad from the intersection of the groove and the patella lines. The
insulated Tuohy needle connected to a nerve stimulator (1.5 mA, 2 Hz,
0.1 ms) is introduced 30° posteriorly (Fig. 29-3B).
With the bevel oriented cephalad, a local contraction of either the
femoris biceps or the vastus lateralis is observed. Within 4 to 8 cm,
the local contractions disappear as the needle enters the popliteal
fossa. Within an additional 0.5 to 1.0 cm, the sciatic nerve is
stimulated and produces either an eversion of the foot or a
dorsiflexion of the foot and extension of the toes (common peroneal
nerve) or an inversion of the foot or a plantar flexion and flexion of
the toes (tibial nerve). The position of the introducer needle is
adjusted to maintain the same motor response with a current of 0.5 mA.
Then, after negative aspiration for blood, the local anesthetic
solution is slowly injected with negative aspiration for blood every 5
mL (Fig. 29-4).
The catheter is advanced 2 to 3 cm beyond the needle tip. The
introducer needle is removed, and the catheter is secured with
Steri-Strip and covered with a transparent dressing (Fig. 29-3C).
-
If the procedure fails to identify the
sciatic nerve, the needle is withdrawn to the level of the skin and
reinserted 45° posteriorly. -
If the needle contacts the femur, it is necessary to withdraw the needle to the skin and reorient the needle 30° posteriorly.
-
This high lateral approach minimizes the
risk for vascular puncture, since the popliteal vessels originate from
the deep femoral vessels usually below the site of introduction of the
needle. Figure 29-4. Diffusion of local anesthetic solution after a lateral approach to the sciatic move.
Figure 29-4. Diffusion of local anesthetic solution after a lateral approach to the sciatic move. -
This approach allows the sciatic nerve to
be reached before its division into the common peroneal and the tibial
nerves, as indicated by the ability to stimulate either branch of the
sciatic nerve with minimum displacement of the needle. -
In most cases, a block of the saphenous
or femoral nerve is also required to complete the anesthesia of the
medial aspect of the leg and ankle and to allow the patient to tolerate
a tourniquet placed at the thigh (femoral nerve block) or the calf
(saphenous nerve).
JE, Greger J, Casati A, et al. Continuous lateral sciatic blocks for
acute postoperative pain management after major ankle and foot surgery.
Foot Ankle Int 2002;23:749–752.
An 18-gauge, 100-mm plastic introducing cannula with a stimulating
short beveled stylet or insulated Tuohy needle and a 20- or 21-gauge
catheter.
20 to 25 mL 0.5% ropivacaine followed postoperatively by a basal
infusion rate of 3 to 5 mL/hour with patient-controlled boluses of 2.5
mL and a lockout period of 30 minutes 0.2% ropivacaine.
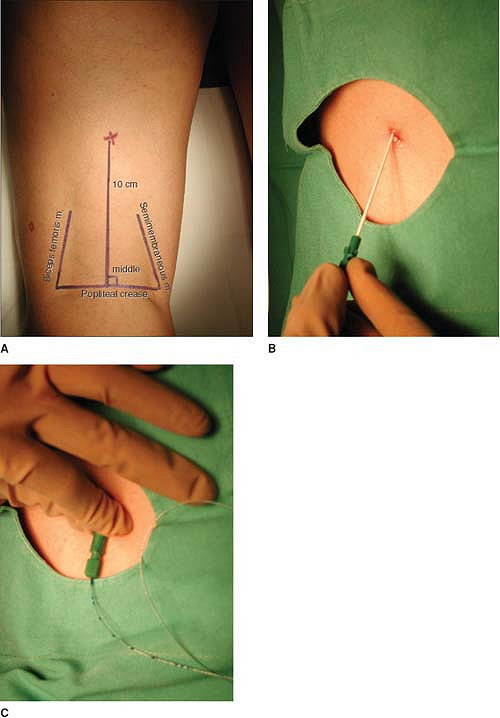
The sciatic nerve divides into the tibial (medial) and common peroneal
nerves (lateral) high in the popliteal fossa (6.1 cm ± 2.7 cm from the
popliteal crease) (Fig. 29-5A).
The patient is asked to lift the leg so that the muscular borders
(biceps femoris laterally, semi-tendinous and semi-membranous tendons
medially) of the popliteal fossa become easily palpable. The site of
puncture is located between the muscles, on the midline, at least 10 cm
above the popliteal crease (Fig. 29-5B).
The introducer catheter, connected to a nerve stimulator (2.5 mA, 2 Hz,
0.1 ms), is introduced at a 45° angle to the skin and advanced in an
anterior and cephalad direction until foot movements (plantar or
dorsiflexion) are elicited. Its position is judged adequate when the
same motor response can be maintained with a current less than 0.5 mA.
The initial bolus dose of local anesthetic is injected after negative
aspiration for blood. The stimulating needle is then removed and the
catheter is introduced into the cannula, with caution being taken to
place it at the same depth as the cannula (Fig. 29-5C). The cannula is removed, and the catheter is secured with Steri-Strip and covered with a transparent dressing.
-
To block both branches of the sciatic
nerves with a continuous infusion, it is essential to place the
catheter before the tibial and common peroneal nerves separate (i.e.,
at least 10 cm above the femoral crease). -
To shorten the onset time, an additional 10 mL of local anesthetic can be injected through the catheter.
-
The highest degree of success with this technique is obtained when an inversion of the foot is obtained initially.
-
Popliteal continuous blocks have been shown to be safe and effective for ambulatory postoperative analgesia.
 |
|
Figure 29-5. A: Landmark; B: Placement of the needle; C: Catheter placement.
|
F, Aye F, Gouverneur JM. Continuous popliteal sciatic nerve block: an
original technique to provide postoperative analgesia after foot
surgery. Anesth Analg 1997;84:383–386.
J, Hadzic A, April E, et al. The division of the sciatic nerve in the
popliteal fossa: anatomical implications for popliteal nerve blockade. Anesth Analg 2001;92:215–217.
