Continuous Lumbar Plexus Blocks
Anesthesia and immediate postoperative analgesia for major knee
surgery, hip arthroplasty, femoral neck fracture surgery, and any
surgery performed in the territory of the femoral and lateral cutaneous
nerves.
30 mL 0.5% ropivacaine (anesthesia), 15 to 20 mL ropivacaine 0.2%
followed by an infusion of 6 to 8 mL/hour 0.2% ropivacaine
(postoperative analgesia).
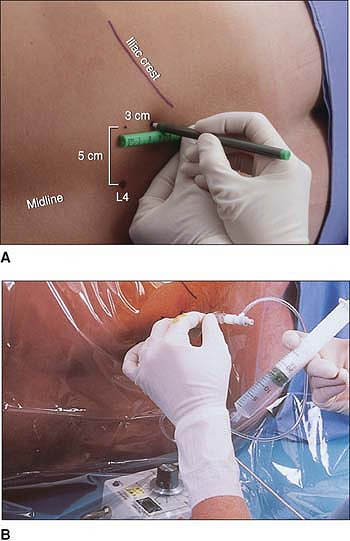
A vertical line is drawn at the level of the superior border of the
posterior iliac crest. Next a horizontal line is drawn at the level of
the spinous process of L5-L4. The site of introduction of the needle is
5 cm above the spinous processes on the bisiliac line. The needle, with
the bevel oriented cephalad, is introduced perpendicular to the skin in
the direction of the transverse process. The needle is then walked
cephalad off the transverse process until a stimulation of the femoral
nerve is elicited. The position of the needle is adjusted to produce a
motor response with a current less than 0.5 mA (Fig. 28-1).
After negative blood aspiration, local anesthetic solution is slowly
injected. The injection is followed by the placement of a catheter
introduced 3 to 5 cm beyond the needle tip. The catheter is secured and
covered with a transparent dressing.
 |
|
Figure 28-1. The lumbar plexus is identified and the needle is advanced.
|
-
When combined with a sciatic nerve block, this block may provide surgical anesthesia to the lower extremity.
-
Epidural spread and/or injections may result in a bilateral block.
-
A loss-of-resistance technique can be used, especially when the block is performed for postoperative analgesia.
-
A more medial approach has been described (3.5 cm from the spinous process).
-
Continuous lumbar plexus blocks should
not be performed in anticoagulated patients, because of the risk of
retroperitoneal hematoma.
X, Macaire P, Dadure C, et al. Continuous psoas compartment block for
postoperative analgesia after total hip arthroplasty: new landmarks,
technical guidelines, and clinical evaluation. Anesth Analg 2002;94:1606–1613.
A, Berkenstadt H, Salai M, et al. Continuous psoas compartment block
for anesthesia and perioperative analgesia in patients with hip
fractures. Reg Anesth Pain Med 1999;4:563–568.
S, D’Ecole F, Greengrass R, et al. Enoxaparin associated with psoas
hematoma and lumbar plexopathy after lumbar plexus block. Anesthesiology 1997;87:1576–1579.
NY, Bennetts FE. An observational study of combined continuous lumbar
plexus and single-shot sciatic nerve blocks for post-knee surgery
analgesia. Reg Anesth 1996;21:287–291.
P, Anker-Moller E, Dahl JB, et al. Postoperative pain treatment after
open knee surgery: continuous lumbar plexus block with bupivacaine
versus epidural morphine. Reg Anesth 1991;16:34–37.
Continuous femoral nerve block works well for postoperative analgesia
in patients undergoing thigh and knee surgery. It does not completely
cover an incision extending onto the tibia, but provides significant
analgesia.
The same as for the single-injection technique (1 cm lateral from the
femoral artery); however, the needle entry point is 2.5 cm below the
inguinal ligament to allow a flatter needle trajectory.
The femoral artery is identified. The needle entry site is 2.5 cm below
the inguinal ligament and 1 to 2 cm lateral to the femoral pulse. The
needle is advanced cephalad at a 60° angle to the skin (Fig. 28-2).
In almost all cases, two distinct pops are felt as the needle passes
through thick fascial planes. The needle is correctly placed when
patellar ascension is noted. The local anesthetic solution is slowly
injected after negative blood aspiration. The catheter is then threaded
3 to 5 cm beyond the needle tip. The Tuohy needle is removed, and the
catheter is secured with Steri-Strip and covered with a transparent
dressing.
-
If the medial thigh is twitching, direct the needle more laterally and at a shallower angle.
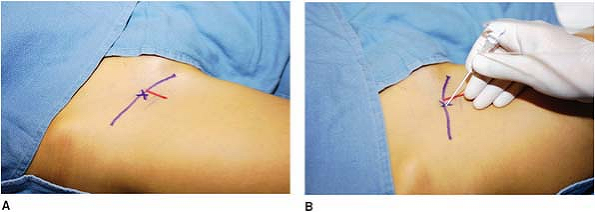 Figure 28-2. The femoral artery is identified and the needle is advanced.
Figure 28-2. The femoral artery is identified and the needle is advanced. -
If the catheter does not thread easily, drop the angle of the needle so it is at a less acute angle.
-
Placing the stimulator under a clear drape allows one person to run the stimulator and drive the needle at the same time.
X, Barthelet Y, Biboulet P, et al. Effects of perioperative analgesic
technique on the surgical outcome and duration of rehabilitation after
minor knee surgery. Anesthesiology 1999;91:8–15.
JE, Gebhard R, Coupe K, et al. Local anesthetic PCA via a femoral
catheter for the postoperative pain control of an ACL performed as an
outpatient procedure. Am J Anesthesiology 2001;28:192–194.
JE, Greger J, Gebhard R, et al. Continuous femoral blocks improve
recovery and outcome of patients undergoing total knee replacement. J Arthroplasty 2001;16:436–446.
S, Wasserman RA, Watson JT, et al. Modified continuous femoral
three-in-one block for postoperative pain after total knee
arthroplasty. Anesth Analg 1999;89:1197–1202.
FJ, Deyaert M, Joris D, et al. Effects of intravenous
patient-controlled analgesia with morphine, continuous epidural
analgesia, and continuous three-in-one block on postoperative pain and
knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg 1998;87:88–92.
FJ, Gouverneur JM. Extended “three-in-one” block after total knee
arthroplasty: continuous versus patient-controlled techniques. Anesth Analg 2000;91:176–180.
Anesthesia and immediate postoperative analgesia for major knee
surgery, hip arthroplasty, femoral neck fracture surgery, and any
surgery performed in the territory of the femoral and lateral cutaneous
nerves.
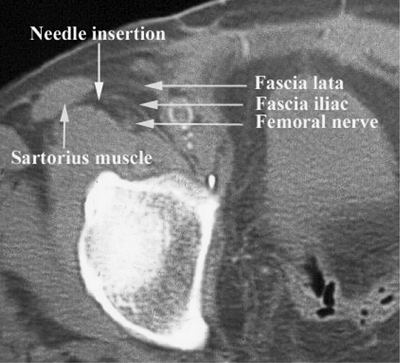
The psoas muscle surrounded by the fascia iliaca and its extensions,
the femoral, lateral cutaneous, and obturator nerves, which run
immediately under the fascia iliaca. When the local anesthetic is
injected under the fascia, the diffusion can theoretically reach the
three nerves (Fig. 28-3).
The anterosuperior iliac spine and the pubic symphysis (inguinal
ligament), the femoral artery, and the sartorius muscle are also
landmarks.
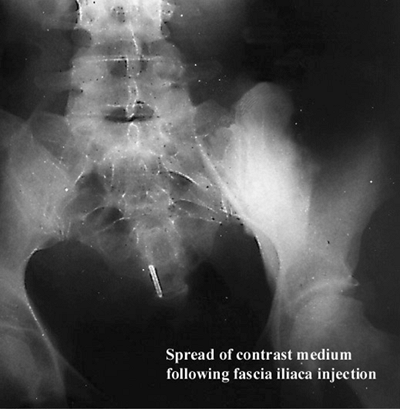
A line between the anterosuperior iliac spine and pubic symphysis is
drawn, demarcating the inguinal ligament. Femoral pulse and the medial
border of the sartorius muscle are palpated, and the femoral artery is
marked. The puncture point is situated 2 to 3 cm below the inguinal
ligament, just distal to the inguinal crease, and 2 to 3 cm lateral to
the femoral artery. The 18-gauge Tuohy needle is introduced through the
skin at a 30° angle. A two-pop loss of resistance perception is felt,
corresponding
to
the crossing of the fascia lata and the fascia iliaca, respectively.
After negative aspiration for blood, 20 mL of local anesthetic is
slowly injected (Fig. 28-4).
This is followed by the introduction of a 20-gauge catheter 3 to 5 cm
beyond the needle tip (8 to 12 cm at the skin). The Tuohy needle is
removed, and the catheter is secured with Steri-Strip and covered with
a transparent dressing.
 |
|
Figure 28-3. Three nerves are identified.
|
 |
|
Figure 28-4. Local anesthetic is slowly injected.
|
femoral cutaneous nerve is evaluated on the lateral aspect of the
thigh. The intensity of the sensory block of the femoral nerve is
tested on the anterior aspect of the thigh and the medial aspect of the
leg (saphenous nerve). The intensity of the femoral motor block is
evaluated through the extension of the leg. Testing the obturator nerve
block is particularly difficult because the sensory territory of the
obturator nerve at the knee is inconsistent and frequently absent, and
because the adduction of the lower limb is only 60% dependent on the
obturator nerve.
-
The lateral part of the fascia iliaca is
a very thick aponeurosis closing the muscular compartment, while the
medial part is a thin perforated aponeurosis. Therefore, a lateral
approach provides a better sensation of the crossing of the fascia.
This is also facilitated by the use of a large-gauge needle with a dull
tip or with a short bevel. -
This block can also be performed with an
18-gauge, 50-mm plastic introducer cannula with a stylet with a 30°
bevel. Once the skin is pierced, the needle is rotated and redirected
cephalad at a 30° angle to the thigh. This slope means the bevel is
parallel to the fascia, thus making penetration more difficult but
easier to recognize. -
A complete block of the femoral and
lateral femoral cutaneous nerves requires time. This approach often
produces an incomplete obturator block. -
The success rate for the iliofascial block is greatly dependent on operator experience.
-
With obese patients, it is sometimes
necessary to have an assistant hold back the abdominal skin to
facilitate recognition of the crossing of the fascia. -
Intravascular injection is possible in
the small caliber circumflex veins that run under the fascia lateral to
the femoral artery. Careful aspiration is necessary before injection. -
Postoperative falls by the patient are
the major risk with this technique, due to the absence of knee locking.
An extension splint is required if the patient is allowed to get up
before recovery from the block.
