Lumbar Plexus Blocks
II – Single-Injection Peripheral Blocks > B – Lower Extremity >
13 – Lumbar Plexus Blocks
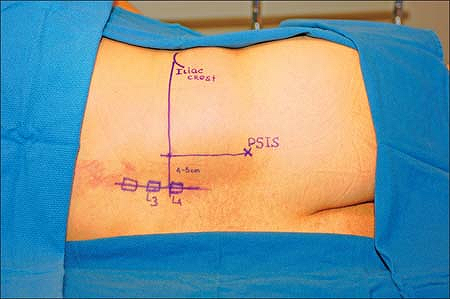
The spinous processes of L4, L5 is identified. A parallel line to the
spinous process line is then drawn, originating from the postsuperior
iliac spine (parasagittal line usually 4.5 to 5 cm lateral to midline).
Next, a vertical line is drawn at the level of the highest point on the
iliac crest (intercrestal line). The intersection of the intercrestal
line with the parasagittal line determines the site of introduction of
the needle (Fig. 13-1).
The insulated needle, connected to a nerve stimulator (1.5 mA, 2 Hz,
0.1 ms) is introduced perpendicularly to the skin and advanced slowly
in search of the transverse process of L4. The introduction of the
needle is first associated with a direct stimulation of paravertebral
muscles. When the transverse process is contacted, the needle is
withdrawn and redirected either caudal or cephalad in search of the
femoral nerve. The stimulation of the femoral nerve produces a
quadriceps contraction and a patella snap. After appropriate
positioning of the needle maintaining the motor response with a current
of less than 0.5 mA and negative aspiration for blood, 2 mL of
ropivacaine is slowly injected. The patient is asked to move both feet
to verify that the injection is not intrathecal. Then 5 ml of local
anesthetic is injected slowly alternating with repeated aspiration for
blood (Fig. 13-2).
 |
|
Figure 13-1.
The intersection of the intercrestal line with the parasagittal line determines the site of introduction of the needle. Iliac Spine (IS). Postsuperior iliac spine (PSIS). |
-
The lumbar spine may be flexed as in the
positioning for a lumbar epidural or spinal technique to help identify
surface anatomy landmarks. -
More cephalad approaches to the lumbar
plexus should be avoided. With a more cephalad approach there is an
increased risk of renal puncture and renal hematoma. Figure 13-2. X-ray indicating appropriate positioning.P.135
Figure 13-2. X-ray indicating appropriate positioning.P.135![]() Figure 13-3. Evaluation of lumbar plexus blocks. Sensory innervation with ice. A: Femoral nerve. B: Lateral femoral cutaneous nerve. C: Obturator nerve.
Figure 13-3. Evaluation of lumbar plexus blocks. Sensory innervation with ice. A: Femoral nerve. B: Lateral femoral cutaneous nerve. C: Obturator nerve. -
One may elicit quadriceps muscle contraction, without hitting the transverse process.
-
If the stimulation of the femoral nerve
in the lumbar plexus does not occur within 2 cm of the transverse
process, the needle is withdrawn from the skin and reintroduced after
increasing the needle angulations by 10° laterally. -
If the transverse process is not
contacted at a depth of 9 cm or deeper, and quadriceps contraction is
not elicited, the needle should be withdrawn and redirected medially. -
Hamstring contraction indicates
stimulation of the L4 component of the sacral trunk at the level of the
nerve root. The needle needs to be withdrawn from the skin and
redirected laterally. -
A scrotum/labial paresthesia indicates
stimulation of genitofemoral nerve (L1 branch of lumbar plexus), which
lies anteriomedial in the psoas compartment. The needle needs to be
withdrawn from the skin and redirected more laterally and less caudally. -
Stimulation of iliohypogastric nerve causes abdominal wall contraction. In this case, redirect the needle more medially.
-
Because of the risk of epidural spread,
it is important to monitor blood pressure during the injection of local
anesthetic to limit the epidural spread. A decrease in arterial blood
pressure is the first symptom suggesting such diffusion. -
Exercise caution with the needle depth to
avoid intraperitoneal injection. Non-obese patients require a needle of
no more than 100 mm in length, inserted to a depth of 70 to 90 mm.
However, with morbidly obese patients the femoral nerve may be reached
P.137P.138
at
a depth of 150 mm. Even in these patients it is recommended to first
start with a 100-mm needle, because there is no correlation between
weight and the depth of the lumbar plexus.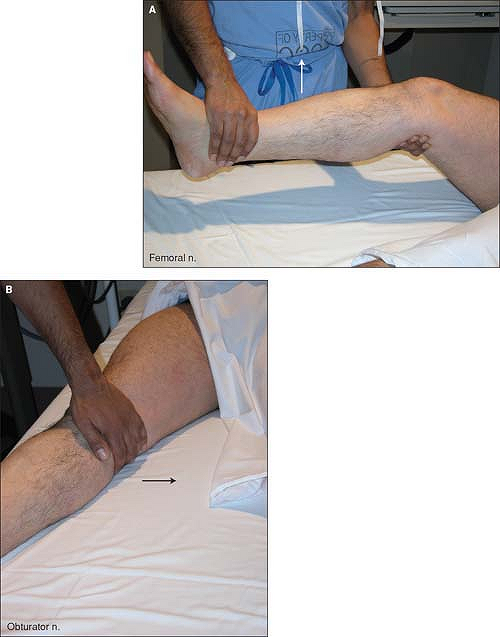 Figure 13-4. Evaluation of motor function against resistance. A: Femoral nerve. B: Obturator nerve.
Figure 13-4. Evaluation of motor function against resistance. A: Femoral nerve. B: Obturator nerve. -
The operator should ensure that a direct
stimulation of the psoas muscle is not mistaken for a contraction of
the quadriceps muscle by having an assistant place a hand on the
quadriceps. -
It is possible to identify the psoas
compartment (a region containing the lumbar plexus) by using a
loss-of-resistance approach. In fact, to reduce the number of
punctures, it is possible to combine the use of the nerve stimulator
and the loss-of-resistance approach by using an insulated needle
connected to both a nerve stimulator (1.5 mA, 2Hz, 0.1 ms) and a
loss-of-resistance syringe filled with 5 mL of air. As the needle goes
through the posterior part of the psoas muscle a direct stimulation of
the muscle is elicited. This muscle contraction disappears and a loss
of resistance is felt when the needle enters the psoas compartment.
After negative aspiration for blood, the local anesthetic solution can
be injected slowly. -
The aspiration of blood suggests the
puncture of a paravertebral vein and indicates that the needle needs to
be redirected laterally. -
Local anesthesia is required to minimize patient discomfort using a 25-gauge, 38-mm needle and 5 mL of 1% lidocaine.
-
Moderate sedation should be provided in most cases with 1 to 2 mg of midazolam and 50 to 100 µg of fentanyl.
-
Evaluation of lumbar plexus blocks:
sensory innervation with ice (femoral [A], lateral femoral cutaneous
nerve [B], and obturator [C]; Fig. 13-3) and motor function against resistance (femoral [A] and obturator [B]; Fig. 13-4).
NY, Bennetts FE. An observational study of combined continuous lumbar
plexus and single-shot sciatic nerve blocks for post-knee surgery
analgesia. Reg Anesthes 1996;21:287–291.
JM, Hanks GA, Rung GW, et al. A comparison of patient-controlled
analgesia and continuous lumbar plexus block after anterior cruciate
ligament reconstruction. Arthroscopy 1993;9:87–90.
R, Van Gessel E, Flory N, et al. Lumbar plexus block reduces pain and
blood loss associated with total hip arthroplasty. Anesthesiology 2000;93:115–121.
Anesthesia and immediate postoperative analgesia for surgery performed
at the level of the anterior aspect of the thigh, femur, and knee, and
the medial aspect of the leg.
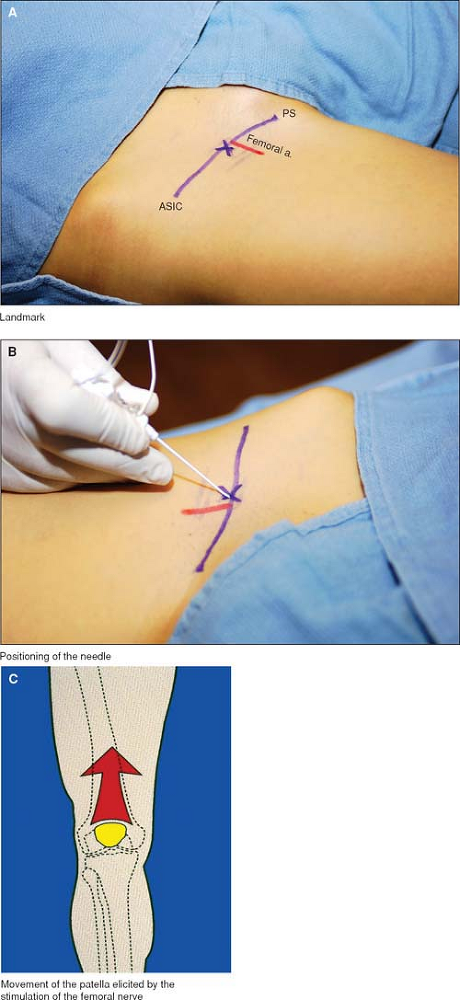
A 22-gauge insulated stimulating needle is connected to a nerve
stimulator (1.5 mA, 2 Hz, 0.1 ms) and is inserted approximately 1 cm
lateral to the femoral artery at the level of the inguinal crease (Fig. 13-8A, 13-8B).
The needle is directed cephalad and advanced at a 45° angle while
maintaining needle orientation in a parasagittal plane without medial
direction. Femoral nerve stimulation results in quadriceps contraction
and proximal patellar movement (Fig. 13-8C).
The needle is positioned to optimize the muscle contraction with a
current of 0.2 to 0.5 mA. The local anesthetic solution is injected
slowly with aspiration for blood every 5 mL to avoid intravascular
injection.
 |
|
Figure 13-5. Anatomic landmarks.
|
 |
|
Figure 13-6. Anatomic landmarks.
|
 |
|
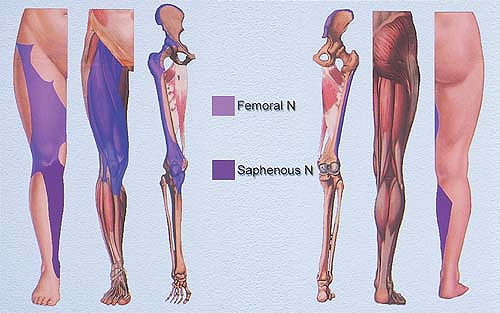
Figure 13-7. Femoral and saphenous nerve distributions.
|
 |
|
Figure 13-8. A:
An insulated stimulating needle connected to a nerve stimulator is inserted approximately 1 cm lateral to the femoral artery at the level of the inguinal crease. |
-
The skin overlying the middle third of
the medial thigh and the middle third of the medial leg are reliable
sensory distributions for testing successful femoral and saphenous
nerve blocks respectively. Successful saphenous nerve block may fail to
include medial malleolus sensory loss at the ankle in about 40% of all
patients. Quadriceps paralysis is the most reliable indicator of a
successful femoral nerve block. -
This approach positions the needle below
the fascia lata at the level of the inguinal ligament. Although it is
possible to obtain an incidental block of the lateral femoral cutaneous
nerve, it is unreliable and concurrently blocked less than 40% of the
time using this approach. -
The lateral femoral cutaneous nerve may
be blocked separately, which may have some value if a thigh tourniquet
is to be used. In adults, the lateral femoral cutaneous nerve is
variable in its anatomy and crosses the inguinal ligament between 1 and
7 cm medial to the anterior superior iliac spine (ASIS). The classic
approach to this nerve is a needle insertion point 2 cm lateral and 2
cm caudal to the ASIS. The needle is inserted to contact bone, and as
the needle is withdrawn, 10 mL of local anesthetic is injected.
Alternatively, a nerve stimulator technique may be used, with a
22-gauge, 5-cm insulated stimulating needle (5 mA, 2Hz, 1.0 ms). The
needle is inserted at the level of the inguinal crease at the
intersection of the lateral one-third and medial two-thirds, with a
paresthesia in the lateral thigh. -
If a quadriceps twitch is not obtained,
the femoral artery should be repalpated to confirm the needle insertion
site. The relevant anatomy may be easily distorted during positioning
especially in obese patients and it is helpful to use tape for pannus
retraction prior to marking the femoral artery. Patients may tend to
rotate their legs laterally while lying supine, which causes the
femoral nerve to lie relatively posterior to the artery in a
parasagittal plane. The patient should rotate feet to anatomical
position prior to defining landmarks and the insertion site. -
Insertion at a point more distal to the
inguinal crease may increase the likelihood of a vascular puncture.
This is due to the lateral femoral artery, which may be present at this
level as a branch of the femoral artery, the profunda femoris, or both. -
The contraction of the sartorius
indicates that the needle needs to be redirected slightly more
laterally and advanced 2 to 3 mm. -
The obturator nerve lies deep and medial
to the femoral nerve and is not reliably blocked with a femoral nerve
block, although it may be blocked using a separate approach.
A, Vloka JD, Saff GN, et al. The “three-in-one block” for treatment of
pain in a patient with acute herpes zoster infection. Reg Anesth 1997;22:575–578.
D, O’ Neill T, Jabbour H, et al. Evaluation of femoral nerve blockade
following inguinal paravascular block of Winnie: Are there still
lessons to be learnt? Anaesthesia 2005;60:974–977.
JD, Hadzic A, Mulcare R, et al. Femoral nerve block versus spinal
anesthesia for outpatients undergoing long saphenous vein stripping
surgery. Anesth Analg 1997;84:749–752.
JD, Hadzic A, Reiss W, et al. Femoral nerve block: needle insertion at
the inguinal crease results in more consistent nerve localization. Reg Anesth 1998;23:53.
Anesthesia and immediate postoperative analgesia following major knee
surgery, hip arthroplasty pain, and femoral neck fracture surgery.
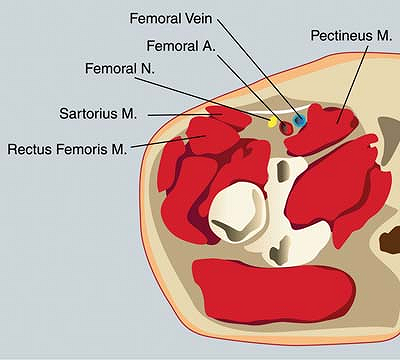
The psoas muscle is surrounded by the fascia iliaca and its extensions.
The target nerves (femoral, lateral cutaneous, and obturator) all run
immediately under the fascia iliaca. When injected under the fascia,
the local anesthetic diffuses around the psoas muscle and theoretically
can reach at least two nerves (femoral and lateral cutaneous nerve).
The lateral part of the fascia iliac is a very thick aponeurosis
closing the muscular compartment while the medial part is a thin,
perforated aponeurosis. Therefore, a lateral approach provides a better
sensation of the fascia penetration.
A line between the anterosuperior iliac spine and symphysis pubis is
drawn, denoting the course of the inguinal ligament. The femoral pulse
is palpated, and another line is drawn to mark the femoral artery. A
third line is drawn to mark the medial border of the sartorius muscle.
The puncture point is situated 2 to 3 cm below the inguinal ligament,
just distal to the inguinal crease, and 2 to 3 cm lateral to the
femoral artery that runs just medial to the sartorius muscle. An
18-gauge, 90-mm noninsulated Tuohy needle is introduced through the
skin at a 30° angle (Fig. 13-9).
A two-pop loss of resistance perception is essential. The first pop
represents the fascia lata penetration, and the second pop places the
needle beneath the fascia iliaca. After negative aspiration for blood,
a local anesthetic solution is slowly injected.
femoral cutaneous nerve is evaluated on the lateral aspect of the
thigh. The intensity of the sensory block of the femoral nerve is
tested on the anterior aspect of the thigh and the medial aspect of the
leg (saphenous nerve). The extension of the leg is impossible with
motor block of the femoral nerve. Testing the obturator nerve block is
particularly difficult because adduction of the lower limb is only 60%
dependent on this nerve. Sensory territory of the obturator nerve is
mainly variable and frequently absent.
-
The use of a large-gauge Tuohy needle allows the clinician to better feel the penetration of the fascia.
-
This block can also be performed with an
18-gauge, 50-mm plastic catheter introducer with a 30° beveled stylet.
Once the skin is pierced, the needle is rotated and redirected cephalad
at an angle of 30° to the thigh. This slope means the bevel is parallel
to the fascia, thus making penetration more difficult but easier to
recognize. -
Complete diffusion of the local anesthetic solution takes time, particularly toward the obturator nerve.
-
The success rate for the iliofascial block is greatly dependent on operator experience.P.145
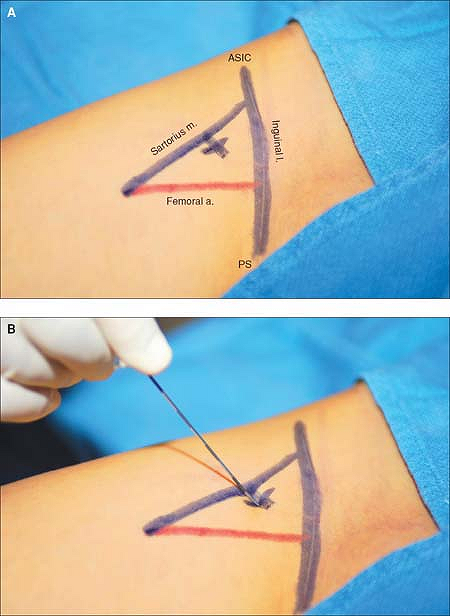 Figure 13-9. A noninsulated Tuohy needle is introduced through the skin at a 30° angle.
Figure 13-9. A noninsulated Tuohy needle is introduced through the skin at a 30° angle. -
With obese patients, it is sometimes
necessary for an assistant to hold back the abdominal skin to
facilitate the recognition of the crossing of the fascia. -
Intravascular injection is possible in
the small-caliber circumflex veins that run under the fascia lateral to
the femoral artery. Therefore, careful aspiration is necessary before
injection. -
Postoperative falling by the patient is a
major risk with the technique, due to absence of knee locking. An
extension splint is indispensable if the patient is allowed to get up
before recovery from the block.
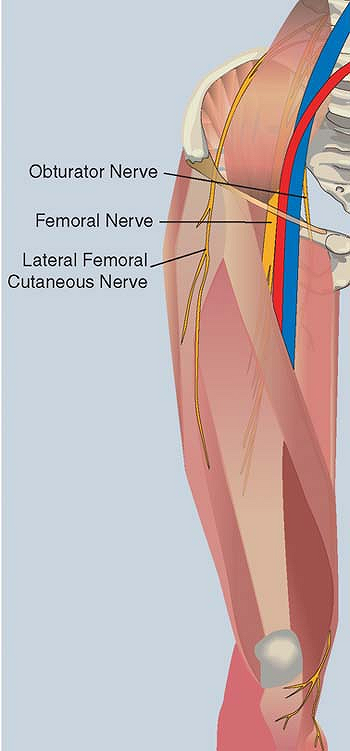
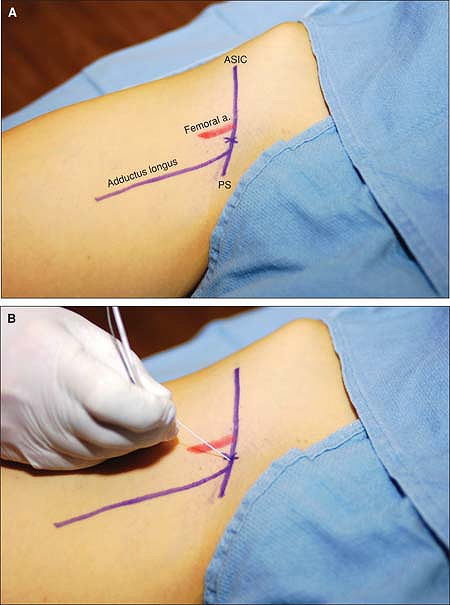
The obturator nerve, originating from the anterior divisions of L2-4,
emerges from the upper anterior aspect of the obturator foramen, runs
medial to the femoral vein and inferior to the pectineus muscle. It
divides into anterior and posterior branches, which straddle the
adductor brevis muscle. The anatomic landmarks are the femoral artery
and medial border of the adductor longus.
The 50-mm insulated needle connected to a nerve stimulator (1.5 mA, 2
Hz, 0.1 ms) is introduced at 45° in the middle between the femoral
artery and the medial border of the adductor longus at the level of the
inguinal crease (Fig. 13-10B). Local anesthetic (5 mL) is injected
when a contraction of the adductor brevis (anterior branch) and a
contraction of the adductor longus (posterior branch of the obturator
nerve) are elicited.
 |
|
Figure 13-10. A:
The femoral artery and the medial border of the adductor longus are palpated and marked at the level of the inguinal crease. The site of the introduction of the needle is the middle between the femoral artery and the adductor longus at the level of the inguinal crease. B: The needle is introduced at a 45° angle. |
-
The intensity of the motor block is
estimated by seeking adductor muscle weakness. The intensity of the
sensory block, however, is difficult to assess because there is
considerable individual variation regarding the sensory obturator
innervation. -
A double-stimulation technique is
necessary because at this level the obturator nerve is divided into an
anterior and posterior branch. -
Obturator nerve block is used to
complement a femoral block and a sciatic block for knee surgery for
anterior cruciate ligament repair or total knee replacement. It may be
considered each time a femoral nerve block is performed for knee or
above-the-knee surgery, especially when a tourniquet is indicated.
SH, Amaya B, Okoniewski M, et al. CT-guided obturator nerve block for
diagnosis and treatment of painful conditions of the hip. Eur Radiol 2001;11:1047–1053.
DA, Parks L, Milligan KR. Post-operative analgesia following total knee
replacement: an evaluation of the addition of an obturator nerve block
to combined femoral and sciatic nerve block. Acta Anesthesiol Scand 2002;46:95–99.

