Fibrous, Fibrohistiocytic, and Giant Cell Tumor Malignancies
Editors: Tornetta, Paul; Einhorn, Thomas A.; Damron, Timothy A.
Title: Oncology and Basic Science, 7th Edition
Copyright ©2008 Lippincott Williams & Wilkins
> Table of Contents > Section
II – Specific Bone Neoplasms and Simulators > 6 – Bone Sarcomas >
6.4 – Fibrous, Fibrohistiocytic, and Giant Cell Tumor Malignancies
II – Specific Bone Neoplasms and Simulators > 6 – Bone Sarcomas >
6.4 – Fibrous, Fibrohistiocytic, and Giant Cell Tumor Malignancies
6.4
Fibrous, Fibrohistiocytic, and Giant Cell Tumor Malignancies
Hannah D. Morgan
Fibrosarcoma, malignant fibrous histiocytoma (MFH) of
bone, and malignancy in giant cell tumor (GCT) are three relatively
rare bone sarcomas that tend to be of high grade. All are found
primarily around the knee. MFH and malignancy in GCT of bone may be
primary or secondary malignancies. Malignancy in GCT is the current
World Health Organization (WHO) terminology for what has also been
referred to as malignant giant cell tumor or dedifferentiated giant
cell tumor. MFH is now referred to as pleomorphic sarcoma not otherwise
specified (NOS) as it is thought to
bone, and malignancy in giant cell tumor (GCT) are three relatively
rare bone sarcomas that tend to be of high grade. All are found
primarily around the knee. MFH and malignancy in GCT of bone may be
primary or secondary malignancies. Malignancy in GCT is the current
World Health Organization (WHO) terminology for what has also been
referred to as malignant giant cell tumor or dedifferentiated giant
cell tumor. MFH is now referred to as pleomorphic sarcoma not otherwise
specified (NOS) as it is thought to
P.202
represent a final common pathway toward dedifferentiation for many sarcomas.
Pathogenesis
Etiology
-
Fibrosarcoma
-
Malignant spindle cell tumor with fibroblastic differentiation and a collagenous intercellular background
-
-
MFH
-
Malignant mesenchymal neoplasm of histiocytic origin
-
72% primary; 28% secondary
-
Conditions associated with secondary
form: bone infarction, fibrous dysplasia, intraosseous lipoma, Paget’s
disease, prolonged steroid use, hematopoietic malignancy, history of
radiation therapy, and possibly presence of metallic orthopaedic
implant (controversial)
-
-
Malignancy in GCT
-
Primary malignancy in GCT: high-grade sarcoma arising beside or within a conventional GCT of bone
-
Secondary malignancy in GCT: high-grade
sarcoma arising at the site of a previously treated conventional GCT
(either with surgery alone or with radiation therapy); tumors often
multiply recurrent prior to diagnosis of malignancy
-
Epidemiology
-
Fibrosarcoma
-
<5% of malignant bone tumors; may be lower as more cases are diagnosed as fibroblastic osteosarcoma or MFH
-
Male:female 1:1
-
Most patients second through seventh decade
-
Arises in metaphysis, most commonly around the knee
-
-
MFH
-
<2% of malignant bone tumors
-
Male:female 3:2
-
All ages affected, but majority >40 years old
-
75% affect ends of long tubular bones; 50% about the knee
-
-
Malignant GCT
-
Very rare: 1% to 2% of all GCT of bone
-
Primary malignant GCT: male > female
-
Secondary malignant GCT: male:female 1:1
-
Average age: 45 to 50 years
-
Secondary malignant GCTs
-
Typically occur >3 years after treatment of original tumor
-
Average latent period: 9 years
-
-
Majority of tumors occur about knee, as for benign GCT of bone.
-
 |
|
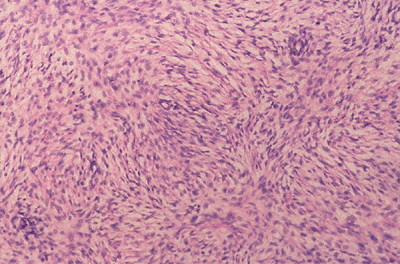
Figure 6.4-1 Fibrosarcoma of bone.
|
Pathophysiology
-
Fibrosarcoma
-
Uniform fibroblast-like spindle cells arranged in parallel bundles with intercellular collagen in herringbone pattern (Fig 6.4-1)
-
One study found 22q aberration leading to increased platelet-derived growth factor beta (PDGF-β).
-
-
MFH
-
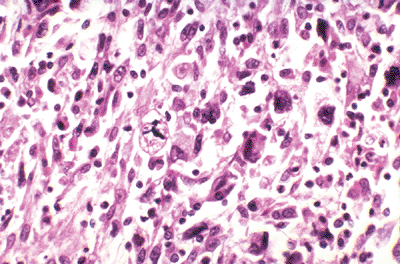
Plump malignant spindle-shaped cells in
sheets and storiform patterns with granular eosinophilic cytoplasm; may
have cytoplasmic vacuoles; marked nuclear atypia and numerous atypical
mitoses (Fig. 6.4-2)
-
-
Malignant GCT
-
High-grade lesions that usually exhibit a
continuum of microscopic change between areas of conventional benign
GCT of bone (multinucleated giant cells with benign spindle cell
stroma) and areas of high-grade sarcoma (usually pleomorphic sarcoma or
osteosarcoma) -
May have p53 or H-ras molecular abnormality
-
 |
|
Figure 6.4-2
Malignant fibrous histiocytoma. An anaplastic tumor exhibits spindle cells, plump lipid-laden histiocytes, tumor giant cells, an abnormal mitosis (center), and a mild chronic inflammatory infiltrate. (From Rubin E, Farber JL. Pathology, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 1999.) |
P.203
Classification
-
Fibrosarcoma
-
May be low- or high-grade malignancy
-
-
MFH
-
Aggressive high-grade tumor
-
Pleomorphic, histiocytic, giant cell, myxoid, and inflammatory variants described
-
-
Malignant GCT
-
High-grade lesions
-
Primary malignant GCT: occurs de novo
-
Secondary malignant GCT: occurs following latent period after treatment of benign GCT of bone with surgery and/or radiation
-
Diagnosis
Physical Examination and History
Clinical Features
Pain and swelling are most common; all may present with pathologic fracture.
-
Fibrosarcoma
-
Nothing unique
-
-
MFH
-
Palpable tender mass
-
Symptoms develop over months to years.
-
Pathologic fracture in 30% to 50% of patients
-
-
Malignant GCT
-
Primary malignant GCT: symptoms present for an average of 12 months
-
Secondary malignant GCT: symptoms present for an average of 7 months
-
Radiologic Features
-
Radiographs
-
Show destructive lytic lesion, often in
metaphyseal area; may have diaphyseal or epiphyseal extension; with or
without pathologic fracture
-
-
Computed tomography (CT) scan
-
Bone involvement
-
Assess intraosseous and extraosseous extent of tumor
-
Best test for demonstrating cortical involvement
-
-
Chest CT
-
Used to look for pulmonary metastases in high-grade lesions
-
-
-
Magnetic resonance imaging (MRI)
-
Best test for evaluating marrow involvement and associated soft tissue mass, which is frequently present with all of these
-
Can also demonstrate cortical involvement
-
Evaluate relationship of tumor to adjacent neurovascular structures
-
-
Bone scan
-
Look for osseous metastasis; determine extent of bony involvement of tumor
-
-
Positron emission tomography: investigational
Treatment
Surgical Indications and Contraindications
Surgical and Nonoperative Options
All high-grade fibrosarcomas, MFH, and malignant GCT of
bone should be treated surgically with the intent of achieving a wide
surgical resection, either by way of limb-sparing surgery or
amputation. Neoadjuvant and adjuvant chemotherapy (often doxorubicin
[Adriamycin]-based) and radiation therapy may enhance tumor control and
are supported by univariate analysis of retrospective
multi-institutional survey data.
bone should be treated surgically with the intent of achieving a wide
surgical resection, either by way of limb-sparing surgery or
amputation. Neoadjuvant and adjuvant chemotherapy (often doxorubicin
[Adriamycin]-based) and radiation therapy may enhance tumor control and
are supported by univariate analysis of retrospective
multi-institutional survey data.
Preoperative Planning (also see Chapter 4, Treatment Principles)
Appropriate imaging studies should be obtained to
determine the extent of resection that is necessary. Any allograft or
orthopaedic implants that will be used for reconstruction should be
ordered. The patient should have a preoperative medical work-up when
appropriate, and blood products should be ordered if significant
intraoperative blood loss is anticipated. Surgical goals and
approaches, techniques, and complications are covered in Chapter 4.
determine the extent of resection that is necessary. Any allograft or
orthopaedic implants that will be used for reconstruction should be
ordered. The patient should have a preoperative medical work-up when
appropriate, and blood products should be ordered if significant
intraoperative blood loss is anticipated. Surgical goals and
approaches, techniques, and complications are covered in Chapter 4.
Results and Outcome (Prognosis)
-
Fibrosarcoma
-
True prognosis difficult to determine, as many tumors once labeled fibrosarcoma are actually MFH of bone
-
Low grade: 10-year survival estimated to be 80%; metastasis in 5% to 20% of patients
-
High grade: 10-year survival 40% or less; metastasis in 55% to 65% of patients
-
-
MFH
-
Estimated 50% to 60% 5-year survival
-
Younger patients and those receiving chemotherapy have better prognosis.
-
-
Malignancy in GCT
-
Approximately 50% 5-year survival
-
Chemotherapy may offer increased survival in some patients, but no randomized prospective trials have been done.
-
Postradiation secondary malignant GCT has worse prognosis.
-
Postoperative Management
Same as for all bone sarcomas (see Chapter 4).
Suggested Reading
Bertoni F, Bacchini P, Staals EL. Malignancy in giant cell tumor of bone. Cancer 2003;97:2520–2529.
Bielack
SS, Schroeders A, Fuchs N, et al. Malignant fibrous histiocytoma of
bone: a retrospective EMSOS study of 125 cases. European
Musculo-Skeletal Oncology Society. Acta Orthop Scand 1999;70(4):353–360.
SS, Schroeders A, Fuchs N, et al. Malignant fibrous histiocytoma of
bone: a retrospective EMSOS study of 125 cases. European
Musculo-Skeletal Oncology Society. Acta Orthop Scand 1999;70(4):353–360.
P.204
Dorfman HD, Czerniak B. Bone Tumors. St. Louis: Mosby, 1998:530–555.
Hattinger
CM, Tarkkanen M, Benini S, et al. Genetic analysis of fibrosarcoma of
bone, a rare tumour entity closely related to osteosarcoma and
malignant fibrous histiocytoma of bone. Eur J Cell Biol 2004;83:483–491.
CM, Tarkkanen M, Benini S, et al. Genetic analysis of fibrosarcoma of
bone, a rare tumour entity closely related to osteosarcoma and
malignant fibrous histiocytoma of bone. Eur J Cell Biol 2004;83:483–491.
Papagelopoulos
PJ, Galanis EC, Sim FH, et al. Clinicopathologic features, diagnosis,
and treatment of malignant fibrous histiocytoma of bone. Orthopedics 2000;23:59–65.
PJ, Galanis EC, Sim FH, et al. Clinicopathologic features, diagnosis,
and treatment of malignant fibrous histiocytoma of bone. Orthopedics 2000;23:59–65.
Smith SE, IKransdorf MJ. Primary musculoskeletal tumors of fibrous origin. Semin Musculoskelet Radiol 2000;4:73–88.
