PATELLOFEMORAL JOINT DISORDERS
Department of Orthopedic Surgery, Stanford University School of
Medicine and El Camino Hospital, Mountain View, California 94040.
relatively little attention until well into the latter half of the 20th
century. Yet today anterior knee pain and dysfunction are among the
major reasons patients seek help. Why was this joint overlooked for so
long? Perhaps the perspective of history will help to answer this
question. During the embryonic stage of orthopaedic surgery, those
general surgeons whom we would now call orthopaedists wrote infrequent
yet classic articles about the patellofemoral joint. These surgeons
were much more concerned, however, with life-threatening and crippling
conditions such as compound fractures, osteomyelitis, pyogenic
arthritis, tuberculosis, poliomyelitis, and birth defects. World Wars I
and II kept the orthopaedic surgeons focused on trauma and infection.
Furthermore, the general population in the United States had little
time for sports involvement during two world wars and the Great
Depression.
vaccines in the 1950s changed the practice of orthopaedic surgery
forever. At the same time, the prosperity of the 1950s and 1960s
allowed increased participation in recreational, scholastic, and
professional sports. Orthopaedists were ill prepared to treat the
increasing numbers of patellofemoral complaints. It remains unknown how
many normal menisci were removed for
“giving way” and “internal derangement” symptoms that were actually
caused by patellofemoral dysfunction. And patellectomy was all too
frequently the final answer to a perplexing and unresolved clinical
problem. Even during the development of “total” knee arthroplasties,
the early designs completely ignored the patellofemoral compartment.
medicine, the development of accurate and reproducible axial
radiographs, and the explosion of arthroscopy all combined to focus
attention on this puzzling joint. Yet
why
are patellofemoral problems so frequent? I believe the answer is
related to the fact that about 20% of an asymptomatic general
population demonstrate objective radiographic abnormalities of the
patellofemoral joint, presumably on a genetic basis (30).
the largest muscles (quadriceps and hamstrings) through the largest
lever arms (femur and tibia), one can now understand why these
relatively minor variations, which become symptomatic as a result of
the added physical demands of sports, are so frequent. This genetic
theory also explains why patellofemoral dysplasia has such a strong
familial predisposition.
this enigmatic and unique joint have been semantic and diagnostic
confusion. Years ago a popular diagnosis in the literature was
“traumatic dislocation.” But aren’t all dislocations of the patella
“traumatic”? Just ask the patient. What that term really implies is
that trauma is the sole cause of the dislocation. After the advent of
accurate axial knee radiographs in the 1970s, it was quickly recognized
that the normal knee rarely suffers a patellar dislocation. Thus, it
remains our duty to search for the abnormality or deficiency that
causes the pain or instability, and we must remember that there are
frequently multiple causes.
originated the term in 1928 to describe the gross appearance at surgery
of previously traumatized articular cartilage. For accuracy and
precision, this term should be used only within this meaning, never as
a solitary diagnosis, and never equated with anterior knee pain.
“Anterior knee pain syndrome” is a deception; it is a symptom
masquerading as a diagnosis. Our medical colleagues treat a stomachache
with a bland diet and antacids without resorting to the use of
“stomachache syndrome.” Why then can’t we treat anterior knee pain with
rest, proper exercises, and antiinflammatories without calling it a
syndrome? If one makes the diagnosis of anterior knee pain syndrome or
chondromalacia patellae, there is the tendency to stop there and not
continue searching for the primary anatomic cause (or causes, for they
are frequently multiple). If a thorough search fails to discover a
cause, there is nothing wrong with the diagnosis of “idiopathic
chondromalacia” or “idiopathic anterior knee pain.”
scientific approach to the patellofemoral joint so that the formulation
of treatment protocols is based on an accurate understanding of the
complex pathophysiology of this fascinating joint.
This classification is designed for clinical use and based on etiology.
Almost always the clinician can establish a diagnosis, or differential
diagnosis, using only a detailed history, a thorough physical
examination, and properly selected routine radiographs. Because many
different patellofemoral disorders respond very well to the same
nonoperative treatment protocols, the clinician can frequently provide
definitive relief working only from a differential diagnostic list.
Only about 10% of patellofemoral patients will fail to respond to these
nonoperative measures (8). If surgery is the
next option, and the diagnosis is still in doubt, then more
sophisticated diagnostic studies such as bone scans, computed
tomography (CT) scans, or diagnostic arthroscopy may be entertained.
Furthermore, by focusing on etiologies rather than symptoms such as
anterior knee pain or secondary changes such as chondromalacia
(chondrosis), a rational treatment program naturally follows.
 |
|
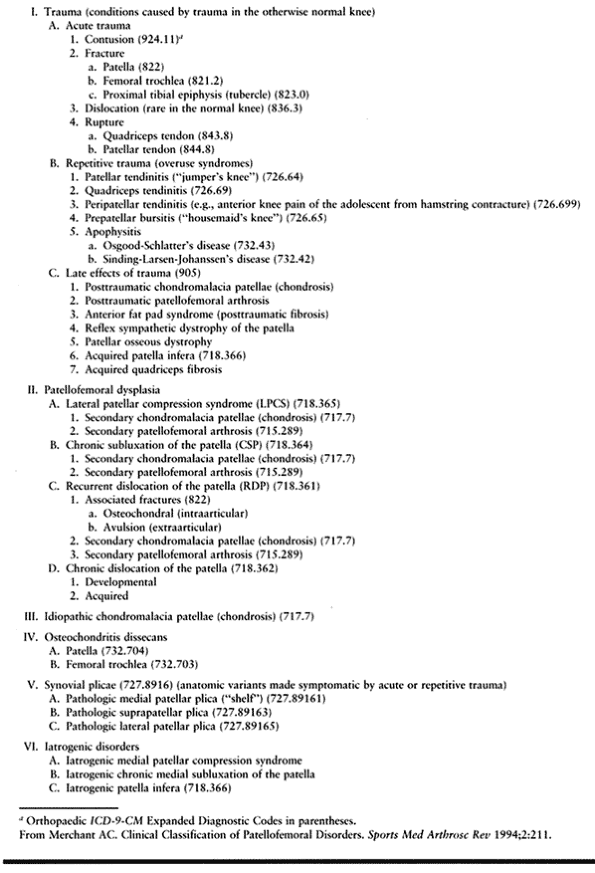
Table 87.1. Classification of Patellofemoral Disorders
|
lists conditions caused by trauma, whether acute, repetitive, or
delayed. These are self-explanatory for the most part and require
little comment. Group II (patellofemoral dysplasia) deals with patients
who have patellar pain and/or instability produced by the activities of
daily living or the normal stress of sports. Patellofemoral dysplasia
is discussed in more detail later in this chapter. Group III allows
inclusion of that ever-shrinking group of patients with proven
chondromalacia patellae for which no cause can be found. Groups IV and
V contain the less common patellofemoral disorders, with no attempt to
include rare entities such as tumors, infections, or metabolic
disorders. Group VI has been added to the original classification (29) to include those patellofemoral disorders of iatrogenicorigin.
that made it so successful in stopping recurrent dislocation of the
patella contained the seeds of its own failure. Medial transfer of the
tibial tubercle down onto the sloping side of the anteromedial face of
the tibia decreased the lever arm through which the extensor mechanism
worked, thereby increasing the patellofemoral joint reaction force. Too
frequently, this produced secondary patellofemoral arthrosis. The
short-term success rate of the Hauser procedure was improved by adding
distal transfer as well. This may have been appropriate for those with
a significant patella alta. However, the folly of treating all patients
who had recurrent dislocations of the patella with one single
operation, no matter what factors were causing their dislocations,
became apparent in longer-term studies. The distal transfer in many
patients produced a severe patella infera, which added to the secondary
patellofemoral osteoarthrosis. Performing a lateral release on a
patient who does not have a tight lateral retinaculum is always a
mistake and easily leads to an iatrogenic medial patellar compression
syndrome or iatrogenic chronic medial subluxation of the patella.
Another cause for these iatrogenic
complications is an excessive, or overzealous, release of the retinaculum and the vastus lateralis muscle as well (21,24).
pain and instability will have objective abnormalities of the extensor
mechanism and patellofemoral joint. These abnormalities are preexisting
and developmental. Major examples include a shallow trochlea, an
increased quadriceps angle (Q-angle), a vastus medialis obliquus (VMO)
deficiency, and a patella alta or infera. These multiple abnormalities
or factors all affect the proper function of the patellofemoral joint.
Each abnormality is not just present or absent in any given patient but
can vary from mild to severe anatomically, thus having a mild to severe
effect on patellofemoral pathomechanics and symptoms.
shallow intercondylar sulcus, deficient vastus medialis obliquus,
patella alta, chronic patellar subluxation, and so on, suggests an
underlying genetic, developmental, or familial abnormality. The
expression of these abnormalities can vary from mild to severe, but it
is helpful to apply the overall and unifying term “patellofemoral
dysplasia.” This term is a better diagnostic category than “maltracking
syndrome” because it indicates a cause, developmental dysplasia, rather
than a common physical characteristic, abnormal tracking.
Patellofemoral dysplasia can be thought of as analogous to
developmental dysplasia of the hip. Embryologically, the femoral
trochlea develops early in utero (8 weeks), complete with its adult predominance of the lateral condyle (16).
At this stage the knee is acutely flexed, and the patella is not even
articulating with the trochlea. Therefore, pressure inhibition from a
laterally subluxed patella cannot influence the trochlear depth. This
is confirmed clinically by the many patients who have a shallow sulcus
and no associated lateral patellar subluxation.
patellofemoral dysplasia and why it is so common in the general
population can be found in studies of comparative anatomy and
phylogeny. Dye (11) has demonstrated that the
bicondylar, cam-shaped design of the distal femur is of ancient origin,
existing in early tetrapods about 360 million years ago. The patella
did not appear until about 70 million years ago. The final human
adaptations of the knee that allowed erect bipedal gait evolved from
quadruped primates and did not occur until 3.5 million years ago. A
valgus femorotibial angle allowed the supporting limb to approach the
midline for efficient bipedal gait, but this change imparted a lateral
thrust on the patella acting through an increased Q angle. The
adaptation of a deeper patellofemoral trochlea with a prominent lateral
femoral condyle and lateral patellar facet plus the development of the
lower oblique fibers of vastus medialis, which is peculiar to humans (4),
allowed the extensor mechanism to function without lateral dislocation
of the patella. It could be possible that these relatively recent human
adaptations of the extensor mechanism are less well “fixed” genetically
and therefore show greater variability, thus explaining the frequency
of patellofemoral dysplasia.
disorders as a developmental dysplasia characterized by a continuum of
anatomic deficiencies. This will tend to focus our attention on the
search for sometimes subtle abnormalities to explain each patient’s
symptoms and help individualize our treatment to correct these
deficiencies.
large category of patellofemoral dysplasia, we must also subdivide this
classification. This will allow those patients with symptoms, signs,
and severity in common to be assessed as a group. Different treatment
protocols can be developed and compared. To do this, we must evaluate
each of the factors associated with patellofemoral disorders known to
influence patellar instability and pain. The normal lateral vector
imparted to the patella by the normal quadriceps angle is resisted by
(a) the depth of the femoral trochlea with its larger lateral condyle
and (b) the vastus medialis obliquus, whose fibers insert more distally
and horizontally on the patella than those of the vastus lateralis. A
deficiency of either the intercondylar sulcus or the VMO or both
predisposes to patellar subluxation and dislocation. Any increase in
the Q angle itself from any cause (e.g., internal femoral torsion,
external tibial torsion, genu valgum) increases the lateral vector on
the patella. There is also a dynamic increase in the Q angle when the
foot is planted and the femur internally rotates during the common
maneuver of cutting and pushing off; this predisposes to dislocation.
The lateral tethering of a tight lateral retinaculum can also increase
the lateral force on the patella, producing the tilt frequently seen
radiographically. A high-riding patella (patella alta) will also
increase patellar instability because it articulates in the more
shallow superior portion of the sulcus for any given degree of knee
flexion compared to the normal. That is, the knee must be flexed more
to bring a high-riding patella safely within the deeper portion of the
trochlea.
clinical evaluation is to establish a differential diagnosis, a
diagnosis, and a logical treatment plan. Because patellofemoral
instabilities and pain almost never arise from a single cause, and in
any given patient each of these multiple factors or abnormalities can
present within a range from mild to severe, the clinician’s job is to
document each and its severity to discover the pathomechanics, the
pathophysiology, and the correct diagnosis and to establish a logical
treatment plan. It is foolhardy to search for
one
physical sign, such as the apprehension response, or one radiographic
finding, such as patellar subluxation, to establish a diagnosis and a
treatment protocol. Each element of this evaluation—the history, the
physical examination, and the routine radiographs—plays an important
and interlocking role. However, the physical examination is paramount
in finding the physical abnormalities causing the patient’s symptoms
and suggesting corrective treatment, both nonoperative and surgical.
Simple checklists can be very helpful in speeding up record keeping and
keeping track of data. Both knees should be evaluated—as a control and
because patellofemoral disorders are so frequently bilateral.
patellofemoral joint, with the understanding that it is only part of a
complete knee evaluation that must also include examination of the
ligaments, the menisci, and the femorotibial articulations. Common
things do occur commonly, so be mindful that any given patient may have
two or more conditions, and they may or may not be symptomatic at any
given time or during certain activities.
after minor trauma indicates a preexisting condition. It is typically
aggravated by flexed-knee activities such as going up and down stairs
and hills (down often worse than up), squatting, kneeling, jumping, and
prolonged sitting (“theater ache”). Constant and unremitting pain
suggests reflex sympathetic dystrophy of neuritic origin.
(combined with a shallow trochlea and/or subluxation on x-ray) of true
patellar instability from the sudden pain and inhibition release
frequently aggravated by quadriceps weakness (with normal axial-view
x-rays). Recurrent patellar dislocation and subluxation almost never
occur with normal findings on axial-view radiographs.
The final common pathway is an excess lateralizing force on the
extensor mechanism, resulting in a lateral patellar compression
syndrome. Check also for foot alignment, because excess pronation can be a cause for anterior knee pain.
 |
|
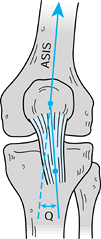
Figure 87.1. Tubercle–sulcus angle. Normal ~0°.
|
the trochlea in active extension and flexion. Does it translate, tilt,
and rotate laterally at terminal extension? This is a J sign because its track follows the pattern of an inverted J.
Look for x-ray confirmation later as patellar subluxation, tilt, or
both on the axial view. A good assessment of the patellar position and
attitude from 30° to 0° obviates the need for the more costly imaging
of CT scans and magnetic resonance imaging (MRIs).
by asking the patient to extend the knee against a fixed resistance at
about 30°. The resultant quadriceps contraction will make the defect
more apparent. Normally the VMO should reach and insert into the upper
third of the patella.
load by palpation during extension and flexion with manual resistance
at the ankle. Manual patellar compression at different degrees of knee
flexion helps to localize segmental chondral lesions.
patellar or quadriceps tendinitis, lateral or medial patellofemoral
joint line synovitis, and any neuromas in the lateral retinaculum or in
prior scars.
extremely important. They not only offer clues for the underlying
pathomechanics leading to a correct diagnosis but also point to
abnormalities to be corrected by exercise, bracing, or surgery. Moving
the patella medially and laterally with the knee relaxed and flexed 30°
demonstrates retinacular contracture or laxity. (Tip: Palpate the
patellar tendon to determine if the patient has relaxed the quadriceps
or not. If not, try performing this test with the patient supine and
the knee relaxed over a pillow or bolster.) The patella should move
about one fingerbreadth in each direction. Excessive lateral glide
means medial laxity, even rupture of the medial patellofemoral
ligament, and may evoke the “apprehension response” as the patient
feels the familiar sensation of dislocation. Restricted medial glide
means a tight lateral retinacular tether. (Tip: Performance of an
isolated lateral retinacular release in spite of an already lax or
normal
lateral
retinaculum represents unnecessary and possibly dangerous surgery.)
Increased medial glide is found in hyperlax individuals (e.g.,
Ehlers-Danlos) and after a lateral release.
for iatrogenic medial subluxation (after either severance of the vastus
lateralis tendon or excessive medial tibial tubercle transfer) is a
variation of the glide tests. With the knee in extension, push the
patella medially as far as possible and hold it there while flexing the
knee passively. If the patella starts to impinge on the medial
trochlear eminence and then suddenly reduces into the groove, and the
patient confirms a reproduction of symptoms, the test is positive.
angle assessment with the patient supine, the knee extended, and the
patella anterior, measure it that way. If another method is chosen, be
consistent. Measure from the anterior superior iliac spine to the
patella (make sure the patella is centered at the trochlea) to the
tibial tubercle. The complementary angle is the Q angle (Fig. 87.2).
The average is about 15° ± 5°. Compare this measurement with the
tubercle–sulcus angle performed earlier. The importance of assessing
the lateralizing forces exerted on the patella by the position of the
tibial tubercle cannot be overemphasized. Again, it provides one more
piece of the pathomechanical puzzle for a correct diagnosis and leads
to a logical treatment plan and a more accurate prognosis. For example,
if a patient suffers recurrent patellar dislocations, and the only
abnormalities are a shallow trochlea and a tight lateral retinaculum,
the chances are excellent that an isolated lateral retinacular release
will be successful. However, the finding of a 25° Q angle ruins that
prognosis, and a medial tibial tubercle transfer will be needed in
addition.
 |
|
Figure 87.2. Quadriceps (Q) angle. Normal ~10°–15°.
|
 |
|
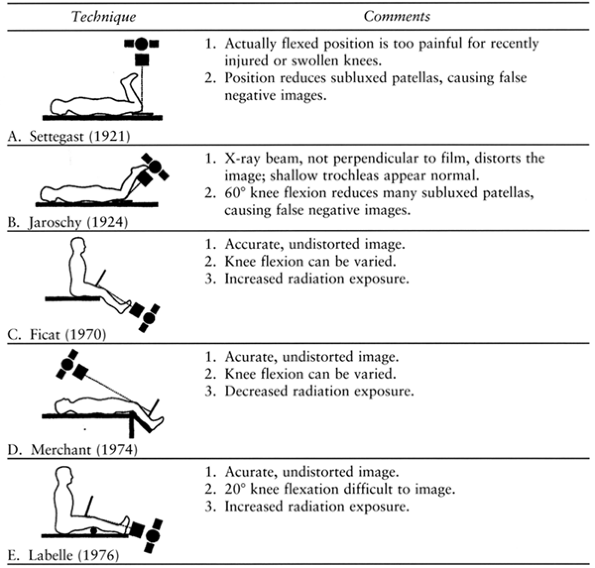
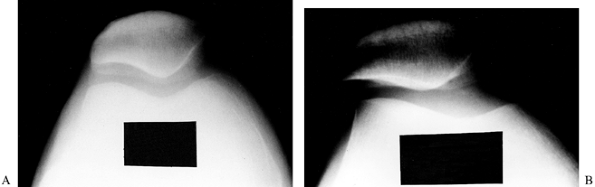
Figure 87.4. Axial patellofemoral radiographic techniques.
|
the femur can be rotated into maximal internal and external rotation to
assess internal and external femoral torsion. Then in the same position
with the ankle at neutral, the thigh–foot angle is measured for
external tibial torsion. These tests can quickly confirm a “miserable
malalignment,” as discussed previously.
and physical examination of the knee. They are, after all, a physical
image extending the physical examination. Radiographs must be used in
context with all the rest of the clinical data to reach a differential
diagnosis, the final diagnosis, and a reasonable treatment plan.
order each view based on clinical suspicions. For example, the tunnel
view is most helpful when loose bodies or osteochondritis dissecans is
suspected. Similarly, when spontaneous meniscal degeneration or
osteoarthrosis is possible, the anteroposterior (AP) view should be
taken during full (100%) weight bearing on one leg using a long
(17-in.) film in order to maximize any joint space narrowing and to
reveal angular deformity.
If the history and physical examination point to a patellofemoral
problem, the axial view will provide the most radiographic information.
Even if no such problem is suspected, it may be harmful to advise
therapy without knowing the status of the patellofemoral joint. In 1988
we demonstrated that approximately 20% of the asymptomatic general
population have objective radiographic subluxation of the patella (29).
If such a patient is placed on “open chain” quadriceps exercises (an
isokinetic machine, short-arc free weights, or isotonic free weights),
the abnormally large joint reaction forces applied to the much smaller
surface contact area can generate destructive forces very quickly,
causing an iatrogenic chondrosis (chondromalacia) that is permanent.
(standing on one leg) exposure on a long (17-in.) film if the patient
is more than 35 years of age, has had a meniscectomy, has an angular
deformity, or has signs of degenerative joint disease or a degenerative
meniscal tear. This
maximizes narrowing and reveals angulation. The posteroanterior 45° flexion weight-bearing view described by Rosenberg et al. (33)
can be selected in addition. It is more sensitive and specific in
assessing articular cartilage loss in the posterior compartments of the
knee.
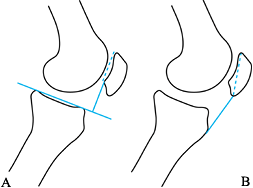
height relative to the joint line: patella alta or infera. The
Blackburne-Peel ratio is more accurate and consistent than the
Insall-Salvati measurements (3) (Fig. 87.3). A long distal patellar tip, or “nose,” can distort the ratio, and on many films the tibial tubercle is difficult to locate.
 |
|
Figure 87.3. Patellar height ratios: (A) Blackburne-Peel ratio 1:1 (±20%); (B) Insall and Salvati ratio 1:1 (±20%).
|
lateral, and the image of the patella is oblique, the patella is tilted
(rotated laterally).
for various techniques). The clinician must know what technique was
used for proper interpretation. Certain techniques cause image
distortion (Fig. 87.4B and Fig. 87.5).
 |
|
Figure 87.5. Axial radiographs of the same left knee taken at the same time. A: By the Jaroschy (“Hughston”) technique, the patella is congruent, and the trochlea appears normal. B: By the “Merchant” technique, the patella is actually subluxed, and the trochlea is actually quite shallow.
|
-
Central x-ray beam must be perpendicular to the film plane to avoid image distortion.
-
Knees flexed 30° to 45°. Less than 30° is
too technically demanding for clinical use, and more than 45° will
reduce many subluxed patellae. -
X-ray tube about 2 m (6 ft) from the knee to minimize the distortion of magnification and parallax.
-
Expose both knees on one film to allow comparisons. Dysplasias are usually bilateral.
-
Strap legs and knees together. This
prevents external rotation, which can simulate a low lateral condyle
and allows the patient to relax (quadriceps contraction will reduce a
subluxed patella).
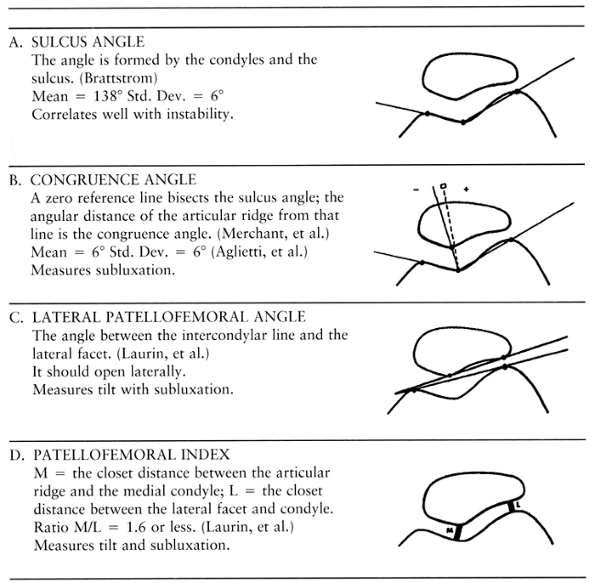
provides the least overlap between normal subjects and patients with
known recurrent dislocation of the patella compared to other
measurements. There is still some overlap, however, so it cannot be
used as the only diagnostic criterion.
 |
|
Figure 87.6. Radiographic measurements of patellofemoral congruence.
|
is the angle between the transverse plane of the patella and a
horizontal line parallel with the x-ray table. The normal value is 5°
or less. Tilt can occur without lateral subluxation (translation) and
usually is an indication of a tight lateral retinaculum, but physical
examination remains the best determinant of lateral retinacular
contracture.
 |
|
Figure 87.7. Radiographic patellar tilt. Normal ~5° or less.
|
 |
|
Figure 87.8. Radiographic clues of long-standing lateral patellar compression syndrome.
|
-
Condensation (sclerosis) of the subchondral bone of the lateral patellar facet.
-
Lateralization of trabeculae (perpendicular to the lateral facet rather than to the transverse plane of the patella).
-
Lateral traction spurs.
and physical examination will be sufficient to establish a working
diagnosis for the great majority of patients with patellofemoral
disorders. Other imaging modalities can be helpful with unusual or
problem cases. A limited CT
scan (15) can be helpful to evaluate patellar position and lateral tilt when the patient is too obese for physical assessment of a J
sign at terminal extension. The three-phase technetium bone scan
(scintigraphy) is the only clinical test that shows physiologic bone
activity (10). It can be very useful for
patients suspected of having reflex sympathetic dystrophy (RSD) and to
document progress during treatment in difficult cases. Given the
current accuracy of MRI in the community setting, it is best used for a
suspected tumor, for preoperative localization of medial patellofemoral
ligament tears (see below), or perhaps when no diagnosis can be
established.
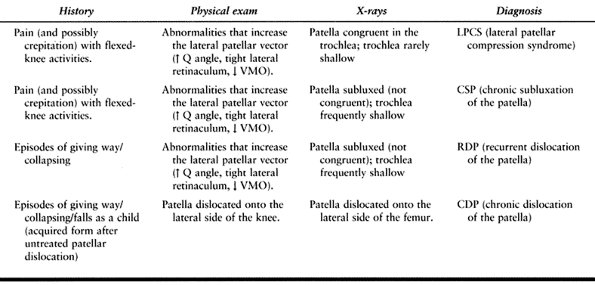
summarizing the various clinical findings needed to make the initial
diagnosis or differential diagnosis and to formulate a rational
treatment plan.
 |
|
Table 87.2. Diagnosis Grid for Patellofemoral Disorders (Dysplasia)
|
are the same: “fix what’s wrong,” with the added caveat, “with the
least risk.” Perhaps that is an oversimplification, but it might
encourage the clinician to search for the various abnormalities
affecting the extensor mechanism and then to select the safest
treatment modality for each abnormality to start treatment. This job is
even harder because each abnormality can vary from mild to severe and
thus have a mild to severe effect on the extensor mechanism, thereby
changing the prognosis for success. In patellofemoral disorders, there
is never only one treatment protocol for one diagnosis. Instead, the
clinician should try to understand the pathomechanics or
pathophysiology leading to that diagnosis in that particular patient,
then list each abnormality found in order to select an appropriate
treatment modality for each factor.
anterior knee pain after relatively minor trauma who fail to recover
after a reasonable time. Evaluation finds a few mild deformities (mild
VMO deficiency, mildly increased Q angle, and mild patellar subluxation
on x-ray), leading to the diagnosis of chronic subluxation of the
patella (CSP). Because these factors were all present before the
injury, it is reasonable to assume that the quadriceps weakness that
resulted from enforced rest and inactivity after the injury caused the
decompensation. Appropriate
quadriceps-strengthening exercises, perhaps along with a lateral
buttress patellar brace during recovery, have an excellent chance of
success. But should that same patient also have an extremely tight
lateral retinaculum that does not respond to patellar taping,
mobilization, and exercise techniques (the McConnell protocol) (18) in addition, then a lateral release will give the patient an excellent prognosis.
each patient’s abnormal extensor mechanism factors but also to each
patient’s age, weight, height, sex, conditioning, activity level,
general health, and expectations as well. For these reasons, it is not
appropriate to list a treatment protocol or algorithm for each
diagnosis but rather to list the various treatment modalities, both
nonoperative and surgical, available for each abnormal factor affecting
the extensor mechanism. The clinician can then individualize treatment
for these multifactorial patellofemoral disorders.
Surgical indications will vary with the severity of the problem, the
degree of disability for the patient, the age and health of the
patient, and the specific surgery proposed. In general, the milder the
objective findings, the longer one should persist with nonoperative
management. In other words, when pain relief is the only measurement of
surgical success, the surgeon should take a long time supervising the
treatment, monitoring the exercise goals, learning the level of patient
commitment to getting well, trying to assess the patient’s pain
threshold, learning the patient’s expectations and desires, educating
the patient on the benefits and risks of surgery, and just getting to
know the patient and significant family members before embarking on a
surgical treatment. Rather than set an arbitrary time limit such as 6
months for exercises before surgery is indicated, it is preferable to
use the expected weight level to be reached, for example, 20 pounds.
This must be monitored and verified.
These measures include the classic rest, ice, compression, and
elevation (RICE), followed by nonsteroidal antiinflammatory drugs
(NSAIDs), and finally judicious use of oral and intraarticular
steroids, if necessary.
successful treatment and rehabilitation of patellofemoral disorders. I
stress appropriate to highlight the unique
biomechanical features of the patellofemoral joint. During physiologic
loading (climbing for example), the patellar contact surface varies directly
with knee flexion and load applied. As the load increases, so does the
contact area of the patella, so the unit load on the patellar cartilage
(the
pounds per square inch) remains relatively stable. Conversely, during
nonphysiologic resistive knee extensions, the load (patellofemoral
joint reaction force) varies inversely
with patellar contact area. Thus, the shrinking contact area of the
patella must carry increasing loads; if the contact area is decreased
even more by subluxation, the unit load can increase exponentially, and
the articular cartilage can be damaged very quickly.
short-arc knee extensions, or isotonic free weights) against
resistance. Start with supine straight-leg raises, assisted if
necessary. Add straight-leg raises with weights to about 5 lb. Then
switch to seated straight-leg weight lifting using the arms to protect
the hip and lower back (Fig. 87.9). To be
successful, a weight goal of 20 to 25 lb is average; for the athlete,
even more. These exercise protocols have been shown to potentiate VMO
strengthening: isometric quadriceps with simultaneous isometric hip
adduction exercises, isometric quadriceps exercises done at 90° knee
flexion (5), and foot forward (posterior pedal contact) with open, or plie, foot alignment during resistance cycling (36).
 |
|
Figure 87.9. Isometric progressive resistive quadriceps exercises (straight-leg weight lifting)
|
-
A patellar strap can be useful for patellar tendinitis.
-
A patellar brace with full ring support can be comforting when the extensor mechanism is already balanced.
-
A patellar brace with a lateral buttress pad helps resist lateral vectors.
-
Longitudinal arch supports provide medial correction for the pronated foot.
features patellar taping techniques designed to reduce the abnormal
forces on the extensor mechanism to allow the patient to exercise and
strengthen the musculature without pain. Once muscles are strengthened,
the taping can be eliminated. However, this protocol requires a
physical therapist who is dedicated to this complex subject of
patellofemoral dysfunction and lower extremity muscular imbalance and
is specifically trained in the McConnell technique. Such a therapist
can be difficult to find.
disorders is almost never indicated. All the forces acting on this
joint are extraarticular and not visible through the arthroscope. If a
pathologic plica is suspected, the arthroscopy is therapeutic. If done
for “chondromalacia,” the surgeon had better understand the cause.
Assuming it was posttraumatic (e.g., dashboard) and the extensor
mechanism is well balanced, then the arthroscopic debridement is
therapeutic. If the chondrosis is secondary to extensor mechanism
malalignment (dysplasia), then the appropriate realignment surgery
should follow the debridement, or the debridement will have been done
in vain.
as a severe patellar subluxation on radiographs, and the younger the
patient, the sooner surgery should be performed. The results of
realignment surgery are better when there is less chondrosis
(“chondromalacia”). Conversely, salvage procedures, such as total
patellofemoral arthroplasty, can be delayed until the level of
disability and future activity expectations are appropriate.
subsequent dislocations will depend primarily on the severity of the
underlying dysplasia. Sometimes an osteochondral fracture (loose body)
with hemarthrosis is present, prompting arthroscopic surgery for its
treatment. When this happens, the surgeon should evaluate the knees
further. Axial radiography will show sulcus depth, and an MRI can
determine if (and where) the medial patellofemoral ligament is torn.
Then, under anesthesia, the lateral retinaculum can be assessed for
tightness and the Q angle measured. With this information, at the same
operation, the osteochondral fracture can be treated, a tight lateral
retinaculum can be released, and a torn medial patellofemoral ligament
can be repaired. This has a good chance of reducing the risk of future
dislocations.
patellofemoral disorders, there is never just one surgical technique
for each diagnosis. Again, the clinician must discover the various
abnormal forces producing that diagnosis, try to understand the
pathomechanics, and then select the safest technique, or combination of
techniques, that has the best prognosis for success. For example, the
lateral release is designed only to correct a tight lateral
retinaculum. If it is already lax, don’t release it. A medial tibial
tubercle transfer is designed only to decrease the Q
angle. It bears repeating that the only way to find these abnormalities is by physical examination.
-
Be as conservative as possible. Remove
only unstable cartilage. Even damaged cartilage will cushion the
subchondral bone and reduce friction better than no cartilage. -
Use as many portals as needed to
correctly position the instruments. Manipulating the patella can help
position it for debridement. -
Try the proximal superomedial portal (see the discussion on arthroscopic lateral release below) for an excellent view.
nonoperative treatment. If it is not tight, don’t release it. If the
patient has a large Q angle as well, an isolated lateral release will
not be sufficient; the tibial tubercle will usually have to be moved
also.
 |
|
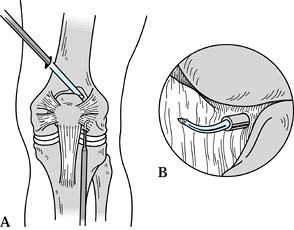
Figure 87.10. A:Arthroscopic electrocautery lateral release. B:
Inset shows the view utilizing the proximal superomedial portal. (Redrawn from Schreiber SN. Proximal Superomedial Portal in Arthroscopy of the Knee. Arthroscopy 1991;7:246.) |
it was an open procedure. As long as the main principles of hemostasis,
adequacy of release, and avoidance of overrelease are addressed, the
results will be the same. Currently, for cosmesis, we prefer the
electrocautery, arthroscopic technique.
-
Use the proximal superomedial portal for viewing (34).
-
Percutaneously insert a guide needle 1 cm lateral to the lateral corner of the patella.
-
Use the anterolateral joint line portal
for the electrocautery. Apply but do not inflate the tourniquet.
Advance slowly near the lateral superior geniculate artery in order to
coagulate it before cutting it. This technique plus the compression
dressing has almost eliminated significant postoperative hemarthroses. -
Avoid severing the vastus lateralis tendon by advancing superiorly in a straight line, not
curving medially, until muscular fibers of the vastus lateralis are
reached. Stop at this point, remove all instruments and cannulas, and
test for adequacy. If the patella can be tilted up 70° to 90° with the
knee in extension, the release is adequate. Frequently, tethering
fibers distally located near the anterolateral joint line portal need
to be cut.
is a large Q angle that is causing the patient’s symptoms, which have
not responded to appropriate nonoperative treatment. When combined with
an arthroscopic lateral release, this can be done through a short
vertical incision at the tibial tubercle for better cosmesis.
 |
|
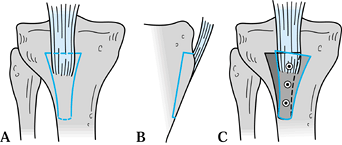
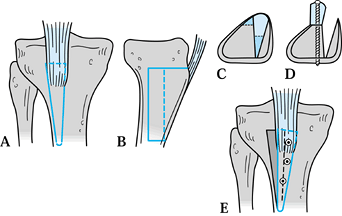
Figure 87.11. Medial tibial tubercle transfer. A,B: Tubercle step-cut proximally and drilled distally, front and side views. C: Tubercle transferred medially and fixed.
|
-
Step cut the osteotomy proximally to
provide a buttress against the quadriceps force. Thin the cut, or drill
the bone distally so it will crack and hinge there as the proximal end
is moved medially. -
Correct the Q angle to about 5° to 10°
measured intraoperatively with a large sterile metal goniometer. The
goal is to normalize and avoid overcorrection. Check the
tubercle–sulcus angle (Fig. 87.1) as well as patellar excursion with flexion and extension. -
Three-screw, bicortical, lag fixation
provides excellent security. Trim the excess bone from the medial edge
of the transferred tibial tubercle and pack it under the medial
overhang as a bone graft. Complete the repair by sewing the previously
elevated medial tibial periosteum to the medial edge of the patellar
tendon. -
Release the tourniquet for hemostasis
before closure. The anterior recurrent tibial artery lurks just lateral
to the tibial tubercle. Uncontrolled hemorrhage from this artery can
cause a disastrous compartment syndrome.
is a Q angle that is normal or has been corrected to normal and a
patella that remains subluxed laterally, causing symptoms, or that
recurrently dislocates. This occurs most frequently in the more severe
forms of patellofemoral dysplasia, which have abnormally shallow
trochleas.
 |
|
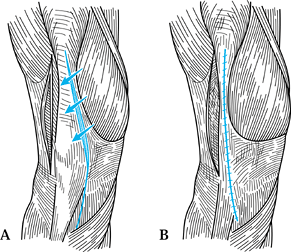
Figure 87.12. Proximal quadriceps plasty. A:Lateral release. B:Tubulization
of the extensor tendon. See text for details. (Redrawn from Insall J, Bullough PG, Burstein AH. Proximal “Tube” Realignment of the Patella for Chondromalacia. Clin Orthop 1979;144:63.) |
offers excellent flexibility to increase the forces acting medially and
reduce those acting laterally. It can be used for moderate alignment
problems and can be modified laterally by releasing the lower third or
half of the vastus lateralis from the lateral intermuscular septum and
lateral femur to perform a derotation quadriceps plasty in those
children with severe chronic dislocation of the patella.
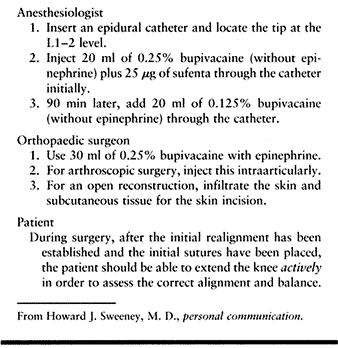
When trying to realign the extensor mechanism when the trochlea is very
shallow or flat, it is extremely difficult, if not impossible, to judge
the proper correction yet avoid overcorrection. It has been compared to
balancing a hockey puck on a cake of ice. If the patient is
cooperative, and the anesthesiologist is facile with epidural and
regional techniques, selective epidural analgesia will be extremely
helpful. Because the motor nerves are spared, the patient can remain
awake or under light short-term sedation. With adequate advance warning
the anesthesiologist can awaken the patient after the first several
repair sutures are in place. The patient then slowly extends the knee
actively from 45° to 0° and back again to test the repair. The surgeon
will see immediately if the result is correct, and adjustments can be
made until it is.
 |
|
Table 87.3. Selective Epidural Analgesia
|
is indicated in those patients with chronic dislocation of the patella
and those with recurrent dislocation of the patella in whom the
ligament is either absent or so incompetent as to be irreparable. This
ligament
has been shown to be the major static medial restraint on the patella (7,9,20).
If the trochlea is shallow and does not provide restraint to lateral
subluxation, simple imbrication of the medial retinaculum without MPFL
repair or reconstruction will frequently fail by gradually stretching
out again. Fithian and Meier (14) have described an excellent technique for repair of the MPFL if it can be identified and its femoral origin is found to be intact.
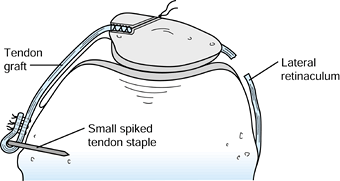 |
|
Figure 87.13. Medial patellofemoral ligament reconstruction.
|
As with the anterior cruciate ligament, reconstruction of the MPFL
requires re-creation of the original anatomy as closely as possible.
Its origin is an isometric point just anterior to the medial epicondyle
of the femur. It courses extraarticularly beneath the fascia of the VMO
to insert on the medial edge of the patella in the upper third. It has
a small cross-sectional area, so many donor sites for the autologous
graft are available. I prefer the central area of the quadriceps
tendon, which is immediately available.
-
Harvest the tendon graft from the middle
of the quadriceps tendon starting just above the patella, 5 to 7 mm
wide and 3 to 4 mm thick; the entire thickness of the tendon is not
required. Measure the length required and add about 2 cm. -
Whipstitch one end using #2 braided polyester suture leaving both ends long.
-
Drill a 5 mm hole, 10 to 15 mm deep, into
the medial edge of the patella at the insertion and enlarge it
vertically with a small burr to accept the graft. From the depth of
this socket hole, drill two smaller suture holes, diverging superiorly
and inferiorly, through the anterior cortex, exiting a minimum of 1 cm
apart. Secure the graft in the socket hole by tying the sutures over
the bone bridge anteriorly. -
Using blunt dissection, pass the graft
superficial to the synovium toward the medial epicondyle. Locate the
isometric point of origin by temporarily fixing this end and moving the
knee. P. J. Erasmus (13) has shown that, in the
normal knee, the MPFL is tight in full extension and relaxes a few
millimeters in flexion. This makes sense because it tethers the patella
medially where the trochlea is shallow and relaxes in flexion as the
increasing trochlear depth resists lateral dislocation. -
Once the isometric point has been
located, prepare a bony bed and insert a small toothed ligament staple
over the graft but do not set it. This will allow the use of a small
clamp proximal to the staple in order to make a final check for
isometricity and length. Then impact the staple securely. Finally,
reverse the small remaining end of the graft, suturing it back onto
itself and to the surrounding soft tissues with #1 braided polyester
suture.
is a salvage procedure similar to the Maquet anterior tibial tubercle
plasty. Anterior transfer increases the tibial lever arm of the
extensor mechanism and reduces the patellofemoral joint reaction force.
This is indicated when there is significant chondrosis (grade III or IV
chondromalacia) that is causing severe disability. In fact, Maquet
originally advocated anterior and medial transfer whenever medial correction was necessary (26).
In practice, the anteromedial transfer will be utilized much more
frequently than the anterior because most severe and symptomatic
patellar chondrosis is secondary to the various forms of patellofemoral
dysplasia with their attendant lateralization of the extensor
mechanism. Anterior transfer is indicated only when the extensor
mechanism is already well aligned, as in pure trauma. Any anterior
transfer is contraindicated when the chondral defect involves the
superior third of the patella because the change will extend or tip the
patella back onto the proximal lesion (32) and can make the symptoms worse.
 |
|
Figure 87.14. Anteromedial tibial tubercle plasty. A: Front view of initial cuts. B: Side view of initial and secondary (dotted line) cuts. C: Cross section of initial and secondary (dotted lines) cuts. D: Cross section after anteromedial transfer and fixation. E: Front view after anteromedial transfer and fixation.
|
and the distance of medial transfer and the distance of anterior
transfer should be independent of one another.
around the tibial tubercle and the adjacent anterior tibial cortex all
the way to the posterior cortex using thin saws and thin nontapered
osteotomes, a rather large block of underlying cancellous bone can be
lifted out carefully with the tibial tubercle (Fig. 87.14A and Fig. 87.14B).
-
Cut a flat ledge on the medial side of the tibia (Fig. 87.14C). Flatten and taper the posterior surface of the
P.2335
cancellous bone under the tibial tubercle with a thin saw. Then rotate
the tibial tubercle with its underlying bone block up onto that medial
ledge with the distal end remaining almost in its original position. As
much as 15 to 18 mm anterior elevation can be achieved with this method. -
Perform intraoperative goniometic
measurement, temporary fixation, and patellar excursion testing as in
the medial tibial tubercle transfer. Again, three-screw bicortical lag
fixation provides excellent security. Remember to release the
tourniquet before closure.
conditions; the results are best when it is done for a comminuted
patellar fracture with a normal trochlea. If it is done for chondrosis
from a patellofemoral disorder with a shallow and eroded trochlea, the
results are generally worse. Furthermore, if pain relief is not
achieved, there is no good alternative—no fall-back position.
-
Realign the extensor mechanism during the
patellectomy carefully; the shallow trochlea promotes recurrent tendon
dislocations. Either the West and Soto-Hall technique (Fig. 87.15) (35)
or a modification of Insall’s proximal realignment (discussed earlier)
with a heavy purse-string suture bunching the soft tissues to create a
“pseudopatella” work well.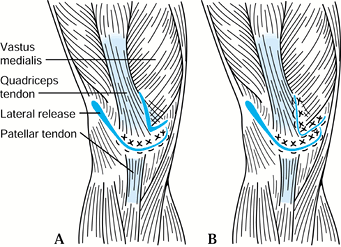 Figure 87.15. Patellectomy with realignment of the extensor mechanism. A:Lateral release and transposition and repair. B:
Figure 87.15. Patellectomy with realignment of the extensor mechanism. A:Lateral release and transposition and repair. B:
Vastus medialis advancement. See text for details. (Redrawn from West
FE, Soto-Hall R. Recurrent Dislocation of the Patella in the Adult: End
Results of Patellectomy with Quadricepsplasty. J Bone Joint Surg 1958:40-A:386. -
If reinforcement of the repair is necessary, a portion of the quadriceps tendon can be turned down.
-
If medial tibial tubercle transfer is
necessary distally, consider anteromedial transfer to improve the
postpatellectomy biomechanics. -
If trochlear chondrosis is present, patellectomy results will be worse; therefore, consider total patellofemoral arthroplasty.
procedure with indications similar to those for other total joint
arthroplasties when isolated patellofemoral arthritis exists. After its
introduction in the mid-1970s, TPFA fell into disfavor, largely, I
believe, because of improper patient selection. More recent studies (2,6,25)
have demonstrated 84% to 88% good and excellent long-term results.
Because the etiology of most patellofemoral disorders and its secondary
isolated patellofemoral arthritis is congenital, the average age of
these candidates will be younger than the usual total joint
arthroplasty patients. Therefore, it is extremely important for the
clinician to impress on patients the need for future activity
restrictions just as for total knee arthroplasty patients. If their
expectations are higher, they are not ready for this operation.
extensor mechanism must be aligned correctly at the time of TPFA if it
has not been realigned before.
that utilize a chrome-cobalt-molybdenum trochlear implant with a deep
or anatomically correct groove articulating with a high-density
polyethylene patellar replacement that mates with it.
identical with the geometry of the femoral component from a total knee
arthroplasty system by the same manufacturer. This confers a big
advantage should a revision to a total knee arthroplasty be required in
the future. At that time, only the trochlear implant will need to be
replaced by the femoral component. The patellar implant will not need
to be exchanged because its geometry will also match the new femoral
prosthesis perfectly.
focuses on two major goals: (a) regaining quadriceps strength and (b)
restoring knee flexibility while protecting the knee during healing.
tissues require protection, so follow straight-leg raises quickly by
isometric resistive (straight-leg weight-lifting)
exercises. The weight goal is the same as the preoperative treatment goal.
(“knee immobilizer”) for a minimum of 6 weeks. Weight bearing in the
extension knee splint does not stress the extensor mechanism, so it can
start immediately after surgery and progress as tolerated to full weight bearing.
as soon as pain allows. Teach the patient to sit on a bed (not dangle)
and then remove the knee splint. By reaching under the knee with both
hands and interlocking the fingers, the patient lifts the knee off the
bed, allowing the heel to slide proximally. Because the patient is in
control and can stretch the knee into as much flexion as pain allows,
postoperative stiffness gradually decreases. A program of 10
repetitions four times a day usually produces 90° flexion in 3 to 4
weeks.
immediately after surgery; it is frequently inhibited by pain. If there
is no response by 1 week postoperatively, add biofeedback and
electrical stimulation techniques. At 3 weeks, start assisted straight-leg raising with full straight-leg raising by 6 weeks. After 6 weeks, begin the patient on isometric resistive (straight-leg weight-lifting) exercises (Fig. 87.9).
These are performed daily, two sets of 10 repetitions, with about 1 lb
added every day or every other day. At 10 lb, the quadriceps is strong
enough to prevent collapse, and the patient can discontinue the splint
for walking. However, have the patient continue to lift to a 20- to
25-lb goal, depending on age and size.
dystrophy (RSD), which is much easier to prevent than to treat.
Prevention begins by being alert and sensitive to the individual with a
low pain threshold and pain out of proportion to objective findings. A
passive approach to getting well can be a clue. A prolonged active
exercise and strengthening program monitored by the surgeon is
invaluable for gaining insight about the patient’s expectations, goals,
effort, cooperation, and responses before surgery. Early recognition
and treatment is more successful than treating a full-blown case. Keep
a high index of suspicion in order to pick up the early warnings and
start treatment promptly and aggressively.
than treatment. The infrapatellar contraction syndrome begins with
postoperative quadriceps shutdown; the
patient is unable to activate this muscle. Place all patellofemoral
patients on a straight-leg weight-lifting program preoperatively, even
if it is not part of the nonoperative treatment. This trains the
patient as well as the neuromuscular pathways so that they will be more
easily recruited postoperatively. Again, early recognition and
aggressive treatment with biofeedback and electrical stimulation are
needed.
tourniquet before closure to assure hemostasis. Also, prevent injury to
the anterior recurrent tibial artery when working lateral to the tibial
tubercle by staying on the bone; avoid straying into the soft tissues
there.
lax. This is especially bad with a hyperlax individual (e.g.,
Ehlers-Danlos syndrome).
inadvertently by “getting lost” or by trying to achieve greater
correction by overreleasing when what is usually needed is medial
tibial tubercle transfer.
use nonabsorbable or permanent sutures. This will allow early motion
and exercise without risk of the soft-tissue repair stretching out.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
SC, Meier SW. The Case for Advancement and Repair of the Medial
Patellofemoral Ligament in Patients with Recurrent Patellar
Instability. Oper Tech Sports Med 1999;7:81.
JP, Schutzer SF, Ramsby G, Bernstein RA. Computerized Tomography of the
Patellofemoral Joint Before and After Lateral Release or Realignment. Arthroscopy 1987;3:19.
AJ, Weinstein RN, Buuck DA, Fulkerson JP. Correlation of Patellar
Articular Lesions with the Results from Anteromedial Tibial Tubercle
Transfer. Am J Sports Med 1997;25:533.
TD, Paulos LE, Parker RD, et al. The Forty-Five-Degree
Posterioranterior Flexion Weight-Bearing Radiograph of the Knee. J Bone Joint Surg 1988;70-A:1479.
B, Burkhardt E, Walker J, Johnson M. Preferential VMO Activation
Achieved, as a Treatment for Knee Disorders. Personal communication.
