Cerebral Palsy
Editors: Tornetta, Paul; Einhorn, Thomas A.; Cramer, Kathryn E.; Scherl, Susan A.
Title: Pediatrics, 1st Edition
Copyright ©2004 Lippincott Williams & Wilkins
> Table of Contents > Section III: – Specialty Clinics > 18 – Cerebral Palsy
18
Cerebral Palsy
Arabella I. Leet
Cerebral palsy results in a wide spectrum of disease
ranging from severely affected children who rely on wheelchairs for
ambulation and who have low cognitive function to mildly involved
children who are difficult to distinguish from idiopathic toe walkers.
Cerebral palsy is a disorder of the central nervous system that causes
neuromuscular derangements in a cascade from abnormality in muscle tone
and strength that can, in turn, have secondary deleterious effects on
bones and joints. Orthopaedic management cannot address the true
location of pathology, which is in the brain, but instead focuses on
making the child more independent with increased functional capacity.
ranging from severely affected children who rely on wheelchairs for
ambulation and who have low cognitive function to mildly involved
children who are difficult to distinguish from idiopathic toe walkers.
Cerebral palsy is a disorder of the central nervous system that causes
neuromuscular derangements in a cascade from abnormality in muscle tone
and strength that can, in turn, have secondary deleterious effects on
bones and joints. Orthopaedic management cannot address the true
location of pathology, which is in the brain, but instead focuses on
making the child more independent with increased functional capacity.
Since cerebral palsy may encompass such a large spectrum
of involvement, both physical and cognitive, treatment must be geared
to the needs of the individual child. The first step is to try to
estimate what might be the highest level of function achievable for a
child, and next devise ways to reach this highest level of function
whether through nonsurgical means (such as braces, medications, or
therapy) or by surgical interventions that can lengthen muscles or
correct bone deformity.
of involvement, both physical and cognitive, treatment must be geared
to the needs of the individual child. The first step is to try to
estimate what might be the highest level of function achievable for a
child, and next devise ways to reach this highest level of function
whether through nonsurgical means (such as braces, medications, or
therapy) or by surgical interventions that can lengthen muscles or
correct bone deformity.
If the orthopaedist understands that what is most
essential to adults with cerebral palsy is the ability to communicate,
the neuromuscular issues become only a part of the management of
cerebral palsy. Thus, a team approach involving therapists,
physiatrists, orthotists, neurologists, developmental pediatricians,
and social workers is often necessary in order to more completely
address the complex needs of an individual patient.
essential to adults with cerebral palsy is the ability to communicate,
the neuromuscular issues become only a part of the management of
cerebral palsy. Thus, a team approach involving therapists,
physiatrists, orthotists, neurologists, developmental pediatricians,
and social workers is often necessary in order to more completely
address the complex needs of an individual patient.
PATHOGENESIS
Etiology
Cerebral palsy is caused by an injury to the developing
brain. By definition the injury is nonprogressive and occurs before age
2, when glialization of the brain is still occurring. The brain
injuries that cause cerebral palsy are diverse. Children with
hemiplegia tend to have a fixed focal lesion in the brain caused by
brain malformation, infection, or embolic event. The pattern of
diplegia results from injury around the third ventricle where the
corticospinal tracks descend from the motor cortex as the corona
radiata en route to the internal capsule. Since the tracks for the legs
are closest to the third ventricle, hemorrhage around the third
ventricle leads to the pattern of injury seen in diplegia where both
legs are involved. Bleeds around the third ventricle, diagnosed by
ultrasound in the nursery can be a predictive sign of diplegia, as can
periventricular leukomalacia (PVL).
brain. By definition the injury is nonprogressive and occurs before age
2, when glialization of the brain is still occurring. The brain
injuries that cause cerebral palsy are diverse. Children with
hemiplegia tend to have a fixed focal lesion in the brain caused by
brain malformation, infection, or embolic event. The pattern of
diplegia results from injury around the third ventricle where the
corticospinal tracks descend from the motor cortex as the corona
radiata en route to the internal capsule. Since the tracks for the legs
are closest to the third ventricle, hemorrhage around the third
ventricle leads to the pattern of injury seen in diplegia where both
legs are involved. Bleeds around the third ventricle, diagnosed by
ultrasound in the nursery can be a predictive sign of diplegia, as can
periventricular leukomalacia (PVL).
Many causes can contribute to cerebral palsy, but almost
50% of children with cerebral palsy are born full term and 35% of the
time the exact etiology remains unknown (Box 18-1).
50% of children with cerebral palsy are born full term and 35% of the
time the exact etiology remains unknown (Box 18-1).
Epidemiology
Cerebral palsy is thought to have an incidence of 1 to 3
per 1,000 live births. It affects over 700,000 children and adults in
the United States. The incidence has remained unchanged over time, but
there has been a shift in the last half century from children with
ataxia (secondary to Rh incompatibility, which is now easily diagnosed
and treated) to children with diplegia (occurring as lower birthweight
children survive with better neonatal intensive care unit management).
Cerebral palsy is associated with prematurity (less than 32 weeks
gestation) and low birthweight (less than 1,500 g).
per 1,000 live births. It affects over 700,000 children and adults in
the United States. The incidence has remained unchanged over time, but
there has been a shift in the last half century from children with
ataxia (secondary to Rh incompatibility, which is now easily diagnosed
and treated) to children with diplegia (occurring as lower birthweight
children survive with better neonatal intensive care unit management).
Cerebral palsy is associated with prematurity (less than 32 weeks
gestation) and low birthweight (less than 1,500 g).
BOX 18-1 POSSIBLE CAUSES OF CEREBRAL PALSY
Prenatal
-
Maternal toxemia
-
Maternal epilepsy
-
Third trimester bleeding
Perinatal
-
Hypoxia (risk factors: placental abruption, nuchal cord)
-
Intracranial hemorrhage
-
Prematurity (low birthweight)
P.199
Pathophysiology
The mechanism of brain injury is not yet completely
understood. Prematurity or endotoxins from maternal infection may
increase the brain tissue sensitivity to injury from other sources such
as hypoxia. After initial injury, there appears to be a cascade of
cellular events that generate the release of cytokines causing further
cellular damage by increasing apoptosis (programmed cell death).
Research on the causes of brain injury is ongoing.
understood. Prematurity or endotoxins from maternal infection may
increase the brain tissue sensitivity to injury from other sources such
as hypoxia. After initial injury, there appears to be a cascade of
cellular events that generate the release of cytokines causing further
cellular damage by increasing apoptosis (programmed cell death).
Research on the causes of brain injury is ongoing.
Classification
Children with cerebral palsy are classified both by the type of muscle tone exhibited and the location of the disease (Table 18-1).
For example, a child whose leg involvement is greater than arm
involvement and who is spastic would be classified as cerebral palsy
subtype spastic diplegia.
For example, a child whose leg involvement is greater than arm
involvement and who is spastic would be classified as cerebral palsy
subtype spastic diplegia.
DIAGNOSIS
Usually the diagnosis of cerebral palsy also is
multidisciplinary involving the pediatrician, neurologist,
orthopaedist, and physical therapist. Depending on the history, workup
often includes:
multidisciplinary involving the pediatrician, neurologist,
orthopaedist, and physical therapist. Depending on the history, workup
often includes:
-
Computed tomography or magnetic resonance imaging or ultrasound of the brain
-
Serology to rule out intrauterine infection
-
Physical therapy evaluation for developmental assessment.
-
Orthopaedic evaluation of the musculoskeletal system
-
Other tests depending on the age and
needs of the child and the presence of visual or hearing impairments,
mental retardation, or medical problems (seizures or pneumonia)
Prognosis
-
Life expectancy is variable and generally
depends on the overall medical condition of the child, including
history of recurrent pneumonias, seizures, and nutritional status. -
Parents often want to know whether their child will walk. Predictors of the ability to walk include:
-
□ Loss of primitive reflexes before 24 months:
-
□ Moro
-
□ Parachute
-
□ Asymmetric tonic neck reflex
-
□ Extensor thrust
-
□ Neck-righting reflex
-
-
□ Sitting by 2 years
-
□ Development of reciprocal activities (e.g., crawling)
-
□ In general, if walking is not achieved
by 7 years, then it is unlikely that a child will develop the ability
to walk in the future.
-
|
TABLE 18-1 CLASSIFICATION OF CEREBRAL PALSY
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||
Physical Examination and History
Physical Examination
-
Observation of extraneous movements (i.e., athetoid motion)
-
Muscle tone
-
□ Subjectively graded as high to low
-
-
Selective control (ability to place limbs in a desired location in space)
-
Sensibility
-
Contracture
-
□ Fixed loss of motion to be distinguished from resistance secondary to high tone.
-
□ There can be a high degree of
variability between exams based on the child’s ability to relax. Tone
will increase if the patient is upset, cold, or frightened.
-
-
Torsional deformity (results in lever arm dysfunction)
-
□ Femoral anteversion
-
□ External tibial torsion
-
-
Balance and equilibrium
-
Gait evaluation
-
□ Observational gait analysis (Box 18-2)
-
□ Three-dimensional gait analysis
-
□ Computer-based evaluation including kinetics, kinematics, and electromyelograph (EMG) analysis
-
-
-
Special physical exam tests used for
cerebral palsy to test muscles that cross two joints that are often
more specifically involved-
□ Phelps test: tests if gracilis muscle is involved compared with hip adductorsP.200
-
□ The patient is positioned prone with the knee flexed.
-
□ As the knee is extended, the hip is observed for adduction.
-
-
□ Silverskiöld test: used to distinguish involvement of gastrocnemius from the soleus.
-
□ With the patient supine, the ankle is dorsiflexed with the knee extended and then again with the knee flexed.
-
□ Since the gastrocnemius attaches at the
distal femur it is relaxed with knee flexion, allowing the foot to
dorsiflex if the soleus is not spastic or contracted.
-
-
□ Duncan-Ely test: distinguishes whether
the rectus femoris or iliopsoas is contracted by observing the pelvis
rising with knee flexion when the patient is prone. -
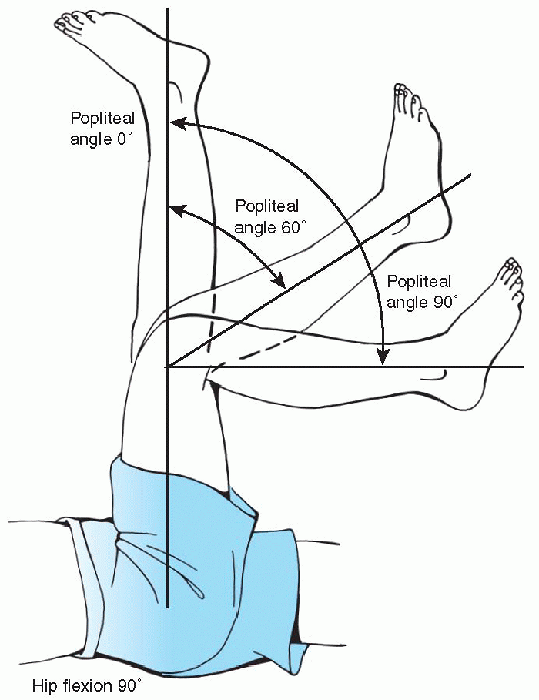
□ Popliteal angle: determines the extent of hamstring involvement across the hip and knee joints (Fig. 18-1).
-
BOX 18-2 FIVE COMPONENTS OF NORMAL GAIT
-
Conservation of energy
-
Stability in stance
-
Clearance in swing
-
Pre-positioning of the foot in swing
-
Adequate step length
Adapted from Gage JR. Gait analysis in cerebral palsy.
Oxford: MacKeith Press, 1991.
History
-
Prematurity
-
Low birthweight
-
Maternal toxemia
-
Placental complications: abruption or previa
-
Medical history to identify seizure
disorders, gastrointestinal reflux, pneumonias, and
strabismus—disorders often seen in children with cerebral palsy -
Developmental milestones
-
Handedness
-
□ Unusual to show hand dominance before 18 months
-
□ Suspect hemiplegia if child is not using both hands
-
 |
|
Figure 18-1 The popliteal angle is measured with the child supine and the hip flexed at 90 degrees.
|
Clinical Features
Children with severe involvement often have microcephaly
apparent to observation, as are extraneous movements. Assessment of
motor tone, by range of motion of joints, reveals increased tone,
clonus, or contractures. Specific secondary orthopaedic developments
from the brain injury include:
apparent to observation, as are extraneous movements. Assessment of
motor tone, by range of motion of joints, reveals increased tone,
clonus, or contractures. Specific secondary orthopaedic developments
from the brain injury include:
-
Hip subluxation/dislocation
-
□ Children with cerebral palsy have
structurally normal hips at birth, but muscle imbalance over time
(especially increased adduction and flexion) can cause the hips to
sublux and finally to dislocate completely causing hip pain and
difficulty with seating and perineal care.
-
-
Scoliosis
-
□ Curves tend to be long C-shaped or S-shaped curves that often include the pelvis.
-
-
Foot deformity
-
□ Pes planovalgus in children with diplegia
-
□ Equinovarus feet develop more commonly in children with hemiplegia.
-
-
Gait deviations
-
□ Caused by deformities to joints from contractures or spasticity
-
□ Proximal compensations are necessary to accommodate distal pathology.
-
□ Problems with balance
-
□ Gait analysis can be a useful tool to
sort deformities (which can respond to surgical correction) from
compensations (which will resolve without the need for intervention
once the true pathology is resolved).
-
-
Upper extremity involvement
-
□ Typically involves elbow flexion,
forearm supination (from pronator spasticity), wrist volar flexion, and
finger fisting or thumb-in-palm deformity -
□ Sensibility may be lost, making
eventual use of arm problematic because correcting the deformity may
not make up for the fact that there is poor sensory information being
relayed back to the brain. -
□ The size of the involved arm has been shown to correlate well with the amount of sensibility:
-
□ If the involved arm is considerably
smaller then the uninvolved side, much of the sensibility in the
involved arm can be assumed to be decreased. -
□ Hygiene problems can result from fisted hand position or from thumb in palm deformity.
-
-
-
Pathologic fracture
-
□ Most children with cerebral palsy have
a significant decrease in bone density. The etiology of low bone
density includes the following:-
□ Non-weightbearing
-
□ Seizure medications (Dilantin, Carbamazepine) can impede vitamin D absorption.
-
□ Poor nutrition leads to insufficient intake of calcium and vitamin D.
-
□ Casting after surgery leads to disuse osteopenia.
-
□ Fractures can occur with transfers or
spontaneously (no recognized event), and are managed by casting (which
can be difficult secondary to shortening while in a cast caused by
muscle spasticity) or alternatively operative strategies including
external or internal fixation.
P.201 -
-
Differential Diagnosis
-
Genetic syndromes
-
□ Familiar spastic paraplegia
-
□ Hereditary microcephaly
-
-
Progressive neurologic disorders
Radiographic Features
-
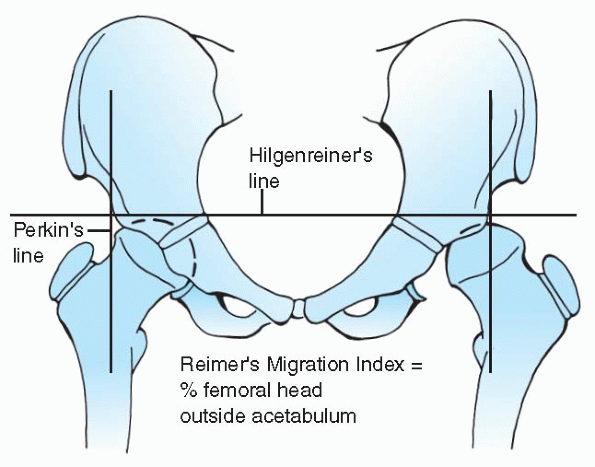
Anteroposterior pelvis: Check for hip subluxation using the Reimer Migration Index (Fig. 18-2).
-
Spine films: Use the Cobb angle technique to measure the amount of scoliosis.
TREATMENT
Decreasing Spasticity
-
Medical
-
□ Baclofen: GABA antagonist, given either orally or intrathecally through pump.
-
□ Botulinum toxin: temporary muscle paralysis.
-
□ Valium: given at 0.1 mg/kg, most
effective of all agents as a muscle relaxant, but also leads to central
nervous system effects
-
-
Surgical
-
□ Selective dorsal rhizotomy usually
performed by a neurosurgeon; dorsal nerve rootlets are identified, and
30% to 60% are divided from L1-S2. Candidate selection for rhizotomy
must be done carefully. The procedure is best for ambulatory spastic
diplegics. The most common complication of rhizotomy is weakness after
the procedure.
-
 |
|
Figure 18.2 Reimer’s Migration Index is a measure of the percentage of femoral head outside the acetabulum.
|
Maintaining Positioning
-
Bracing upper and lower extremities to maintain functional positions
-
□ Ankle foot orthosis (AFO) made out of semi-rigid material
-
□ May be solid or articulated, depending on ambulatory status
-
-
Seating system in nonambulatory children
-
□ Position the trunk upright, head forward, so children can interact with the world around them
-
□ Accommodate trunk and pelvic deformity in design of wheelchair
-
□ Use of tilt chairs prevents skin breakdown in children who cannot shift their weight while sitting
-
□ Use electric wheelchairs, if child capable of steering safely.
-
□ Traditional custom wheelchairs are
often difficult to transport in a car, thus families also will need a
stroller-type device that is more portable.
-
Managing Deformity
-
Soft-tissue release: lengthening a
muscle, whether at the musculotendinous junction or through the tendon,
treats fixed contractures but also results in muscle weakness.-
□ Adductor tenotomy
-
□ Indications: a Reimer Migration Index
of more than 50 percent, or loss of more than 30 degrees of hip
abduction in hip extension resulting in difficulty with diapering, or
perineal hygiene
-
-
□ Gastrocnemius recession
-
□ Indication: for ankle equinus and a positive Silverskiöld test (soleus not contracted)
-
-
□ Tendo-Achilles lengthening
-
□ Reserved for equinus involving both gastrocnemius and soleus muscles
-
□ Must be careful not to over lengthen the tendo-Achilles, which will result in an iatrogenic crouch gait
-
□ Hamstring lengthening
-
□ Indications: popliteal angles greater
than 45 to 60 degrees or difficulty with sitting secondary to extension
of the pelvis from the proximal attachment of the hamstrings -
□ Medial or medial and lateral depending on the amount of the popliteal angle preoperatively
-
-
-
Tendon transfer: aimed to rebalance muscles around a joint
-
□ SPLATT/SPLOTT (split anterior or posterior tibialis tendon transfer)
-
□ Indications: hindfoot varus, passively
correctable, and identification of spasticity (may require EMG) in
either the posterior or anterior tibialis muscle
-
-
-
Osteotomies: correction of bone for torsional correction or to address deficiency of structures (i.e., acetabulum)
-
□ Varus derotation osteotomy (VDO) of the proximal femur
-
□ Pelvic osteotomy (Dega, Chiari)
-
□ Indications: acetabular deficiency
-
□ Acetabulum usually deficient in
children with cerebral palsy posteriorly or laterally, as opposed to
hip dysplasia where the deficiency tends to be anterior
-
-
□ May be performed in combination with VDO
-
□ Os calcis lengthening
-
□ Indications: for flexible pes planovalgus
-
□ Navicular is subluxed on the talar head
-
-
-
Fusion
-
□ Spine
-
□ Indications: for scoliotic curves of
greater than 50 degrees that are rigid. Traction films can help
determine curve flexibility, as can clinical examination. -
□ Add anterior release or fusion for excessively large curves (more than 70 to 80 degrees)
-
□ Fuse to include the pelvis if there is pelvic obliquity
-
□ Since fusions are long, allograft often used as bone graft
-
-
□ Subtalar joint
-
□ Indications: for pes planovalgus that is not passively correctable
-
□ Great toe for hallux valgus deformity
-
□ Routine bunion corrections less reliable
-
□ Must fuse in 20 to 30 degrees of dorsiflexion
-
-
SUGGESTED READING
Abel
MF, Damiano DL, Pannunzio M, et al. Muscle-tendon surgery in diplegic
cerebral palsy: functional and mechanical changes. J Pediatr Orthop
1999;19:366-375.
MF, Damiano DL, Pannunzio M, et al. Muscle-tendon surgery in diplegic
cerebral palsy: functional and mechanical changes. J Pediatr Orthop
1999;19:366-375.
Bleck EE. Orthopedic management in cerebral palsy. Oxford: Blackwell Scientific Publications, 1987.
Comstock
CP, Leach J, Wenger DR. Scoliosis in total-body involvement cerebral
palsy. Analysis of surgical treatment and patient caregiver
satisfaction. Spine 1998;23:1412-24.
CP, Leach J, Wenger DR. Scoliosis in total-body involvement cerebral
palsy. Analysis of surgical treatment and patient caregiver
satisfaction. Spine 1998;23:1412-24.
Cosgrove
AP, Graham HK. Botulinum toxin A prevents the development of
contractures in the hereditary spastic mouse. Dev Med Child Neurol
1994;36:379-385.
AP, Graham HK. Botulinum toxin A prevents the development of
contractures in the hereditary spastic mouse. Dev Med Child Neurol
1994;36:379-385.
Dolk
H, Pattenden S, Johnson A. Cerebral palsy, low birthweight and
socio-economic deprivation: inequalities as a major cause of childhood
disability. Pediatr Perinatal Epidemiol 2001;15:359-363.
H, Pattenden S, Johnson A. Cerebral palsy, low birthweight and
socio-economic deprivation: inequalities as a major cause of childhood
disability. Pediatr Perinatal Epidemiol 2001;15:359-363.
Gage JR. Gait analysis in cerebral palsy. Oxford: MacKeith Press, 1991.
Miller F, Cardoso Dias R, Dabney, KW, et al. Soft-tissue release for spastic hip subluxation. J Pediatr Orthop 1997;17:571-584.
Rang M, Douglas G, Benner GC, et al. Seating for children with cerebral palsy. J Pediatr Orthop 1981;1:279-286.
Sussman MD. The diplegic child. evaluation and management. Rosemont, IL: American Academy of Orthopedic Surgery, 1992.
Winters
TF, Gage JR, Hicks R. Gait patterns in spastic hemiplegia in children
and young adults. J Bone Joint Surg (Am) 1987;69:437-441.
TF, Gage JR, Hicks R. Gait patterns in spastic hemiplegia in children
and young adults. J Bone Joint Surg (Am) 1987;69:437-441.
