Patellar Fractures: Open Reduction Internal Fixation
majority of displaced patellar fractures. Surgical options include open
reduction and internal fixation (ORIF), partial or complete
patellectomy, with the choice of treatment dependent on the fracture
pattern and the amount of comminution. Although there is no widely
accepted classification system for patellar fractures, most are based
on an anatomic descriptive classification. Important factors include
the location of fracture, direction of fracture lines, and the amount
of comminution. In the AO/OTA classification, the patella is delineated
as 45 and subdivided into A, B, or C depending on whether the fracture
is extra-articular, partial articular without disruption of the
extensor mechanism, or complete articular with disruption of the
extensor mechanism. For the most part, 45B patella fractures are
managed nonoperatively whereas 45A and 45C fractures require surgery.
mechanism of the knee as well as an articular component of the knee
joint. The patella’s position in the body and the nature of its role in
lower-limb function cause it to be susceptible to injury. Traction
forces that pull the patella cephalad are the result of several
different vectors caused by contraction of the quadriceps muscle. The
quadriceps muscle, extensor retinaculum, along with the iliotibial
band, participates in knee extension. The undersurface of the patella,
which articulates with the notch of the femur, has the thickest
cartilage found in the body. It is this articulation that acts as a
fulcrum for extension. Forces measured at the patellofemoral
articulation can be over seven times body weight during routine
activities such as stair climbing and squatting. Tensile forces can be
well over 3,000 N. The importance of the patella for normal knee
function cannot be overestimated. Patellectomy results in the loss of
the patellar fulcrum, a decrease in the moment arm, and relative
lengthening of the quadriceps. This can lead to instability of the
knee, extension lag, atrophy of the quadriceps, and loss of extension
strength. Therefore, whenever possible, the patella should be repaired
rather than excised.
patella is so severely comminuted that an acceptable reduction and
stable fixation cannot be achieved with internal fixation.
Partial
patellectomy is indicated for cases that have severe comminution of
either the inferior or superior pole that is not amenable to ORIF
techniques.
have fragments large enough to be reduced and stably repaired and is
the treatment of choice for the majority of displaced patellar
fractures in physiologically young patients. Many comminuted fractures
can be salvaged. The goal of surgery is to achieve anatomic reduction
of the articular surface with restoration of the continuity of the
extensor mechanism. Displacement more than 3 mm and articular
incongruity of more than 2 mm are considered strong indications for
surgical treatment.
surgical treatment include nondisplaced or minimally displaced stable
fracture patterns. Also, contused or injured skin that precludes safe
surgical approaches to the fracture, active infection involving the
extremity with the patellar fracture, and medical conditions of the
patient that would preclude safe surgical intervention are
contraindications for surgery.
should be performed. The mechanism of injury may explain the severity
of injury as well as the fracture pattern. It is helpful to know
whether the injury occurred as a result of a direct blow (e.g., a fall
on the knee) or from resisted flexion of the knee resulting in a
traction-type injury.
evaluation of the extremity, with the surgeon looking for signs of
direct trauma and swelling. The presence of fracture blisters,
lacerations, abrasions, and contusions should be documented. It is
essential to determine whether the fracture is open. Superficial or
small wounds should be checked and if necessary carefully explored to
determine whether they are in continuity with the fracture or the knee
joint. In displaced patellar fractures, a visible or palpable defect is
often noted between the fragments, although this may be masked by
significant swelling, which develops rapidly. In some cases, a
hemarthrosis is not apparent because of a large retinacular tear that
allows blood to dissipate into the surrounding soft tissues. The
absence of a hemarthrosis does not rule out a patellar fracture.
next. A painful, tense hemarthrosis often complicates this part of the
examination. Aspiration of the knee with injection of a local
anesthetic usually decreases pain. The patient is asked to contract the
quadriceps mechanism and attempt to extend the knee fully. The ability
to do this does not rule out a patellar fracture because the medial and
lateral retinacula may still be intact, providing partial continuity of
the extensor mechanism. However, the inability to lift the leg usually
indicates that a patella fracture that tears the medial and lateral
retinaculum exists. Gentle stress testing of the knee for stability
should be carefully performed. Knee flexion should be avoided because
this may further displace the fracture in addition to causing
significant discomfort to the patient. The peripheral pulses and the
compartments of the leg should be evaluated, and a neurologic
examination performed.
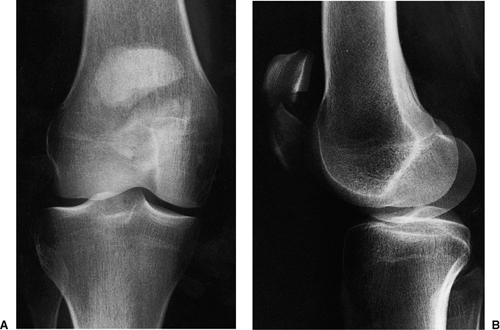
following injury include anteroposterior (AP), lateral, and axial views
of the patella. A supine AP radiograph is obtained, centered over the
patella (Fig. 24.1). The lateral radiograph can
be taken as a cross-table lateral, with the knee slightly flexed. For
an axial view, a Merchant’s view is most easily and safely obtained in
the injured patient (Fig. 24.2). The patient is
placed supine on the x-ray table with the knee flexed 45 degrees over
the end of the table. The x-ray beam is angled at 30 degrees from the
horizontal, and the cassette is placed perpendicular to this x-ray beam
1 foot below the knee. Comparison views of the uninjured knee can be
helpful in selected patients (i.e., those with a bipartite patella).
Occasionally in patients with complex fracture patterns, a computed
tomography (CT) scan is indicated.
lateral views and are best visualized on the axial view. Larger
displaced-fracture lines can be readily seen, although smaller
nondisplaced-fracture lines are often obscured because of the
superimposition of the patella on the femur in the AP view. In most
cases, the fracture is more comminuted than is
apparent
on the radiographic evaluation. Displacement more than 3 mm and
articular incongruity more than 2 mm are indications for surgery.
 |
|
Figure 24.1. A. AP and lateral radiographs (B)
showing a transverse fracture of the patella with comminution of the distal fragment. The lateral view shows significant comminution involving the articular surface in addition to displacement of the proximal and distal pole fragments. |
fracture patterns. Surgeons should make a tracing on both the AP and
lateral views of the uninjured contralateral side and then superimpose
the fracture lines from the injured side onto the normal template. The
fixation should be drawn and the procedural steps carefully listed. The
operating room should be informed of the equipment required based on
the preoperative plan. Equipment needed for surgery usually includes
various-sized pointed bone-reduction clamps, small curettes, wire
cutters, benders, and wire tighteners, and small Kirschner (K) wires.
Power drills and wire drivers will also be necessary. Small and mini
fragment screws and instruments should be available.
 |
|
Figure 24.2.
Axial view of the patella showing a vertical fracture of the lateral facet of the patella. There is minimal displacement of the fragments. |
been prepared and appropriate preoperative plans completed. If the
fracture is open, surgery must be done urgently. Closed fractures
should be surgically addressed when the soft-tissue injury and the
general condition of the patient permit.
table. Because there is a tendency for the leg to externally rotate, a
small bump can be placed under the ipsilateral hip. A tourniquet is
placed high on the involved thigh. The procedure can be done under a
general or spinal anesthetic. Regional nerve blocks (femoral nerve
block) can be very helpful to control postoperative pain. The patient
is prepped in a standard fashion, and the leg is draped free by using
an extremity drape. The limb is exsanguinated with a sterile Esmarch,
and the tourniquet inflated to a pressure appropriate for the size of
the leg and the patient’s blood pressure. Before inflating the
tourniquet, the quadriceps is pulled distally to ensure that it is not
trapped under the tourniquet, which can displace the patella
proximally, making reduction more difficult. A sterile bump can be
placed behind the knee, which allows the knee to flex 15 to 20 degrees.
Appropriate antibiotic prophylaxis should be given before inflating the
tourniquet.
longitudinal. A longitudinal incision is preferred when more proximal
and distal dissection is necessary for the repair of a comminuted
fracture and when later reconstruction procedures are anticipated. For
cosmetic reasons, the transverse incision is preferred. It also avoids
potential damage to the saphenous branch of the femoral nerve.
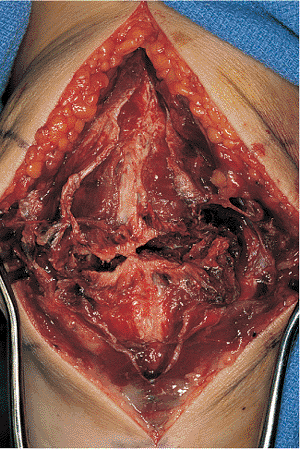
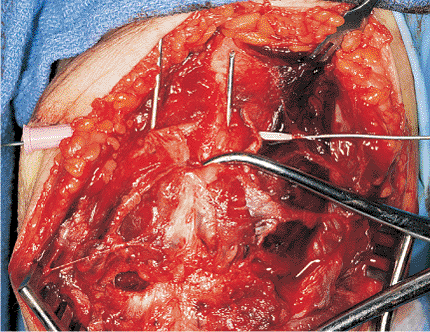
tissue and the prepatellar bursa. A hematoma is usually encountered as
soon as the bursa is opened, and it usually leads directly into the
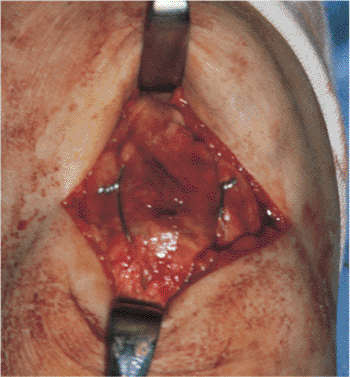
fracture site (Fig. 24.3). Care should be taken
to minimize direct dissection of the fracture fragments. The soft
tissues surrounding the patella often hold nondisplaced fractures in
place, and if these are disrupted, the fragments may displace, creating
a more complicated and unstable fracture pattern. The major fracture
fragments should be exposed. Clot
should
be removed with a combination of small curettes and the use of a small
suction-tip device. Irrigation should be used liberally to help remove
the hematoma and small inconsequential comminuted fragments. The extent
of the medial and lateral retinacular injuries should be identified and
the edges tagged for later repair. The undersurface of the patella, in
addition to the patellofemoral groove, should be inspected for evidence
of articular damage. The knee joint should be inspected and irrigated
to remove any loose fragments.
 |
|
Figure 24.3.
Surgical exposure through a vertical midline incision showing the transverse fracture of the patella with medial and lateral retinaculum tears. The soft tissues have been left intact over the surfaces of the patella. |
 |
|
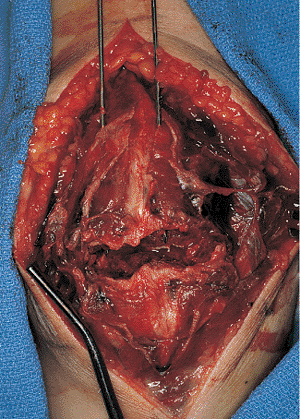
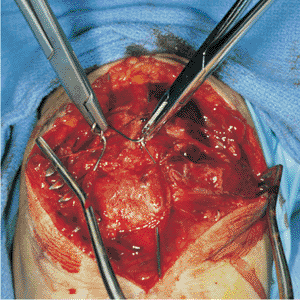
Figure 24.4.
The hematoma has been evacuated, and the joint and fracture lines have been debrided. The K wires have been advanced retrograde through the patella, and the patella fragments are now ready to be reduced. |
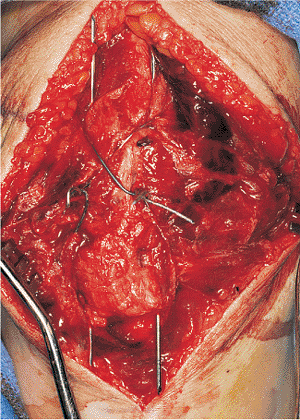
thoroughly irrigated, the fracture edges carefully exposed, and the
fracture pattern thoroughly delineated, a preliminary reduction is
performed. The small bump behind the knee will need to be removed at
this time because flexion of the knee will make the reduction more
difficult. In the case of a simple, transverse, middle-third fracture,
one can proceed directly to the tension band technique. In other more
complex fractures, the goal is to try to reduce the fragments to create
a two-part transverse-fracture pattern that can then be further
stabilized with a tension band technique. For example, if there is a
vertical split through either the proximal or distal fragment, the
vertical split is first reduced and held temporarily with large,
pointed, reduction forceps. This is then temporarily stabilized with a
1.2-mm K wires. Definitive stabilization of this fragment depends on
its size and can be done with either K wires or small-fragment or
mini-fragment screws. After this has been performed, the tenaculum
clamps and the provisional fixation are removed.
tension-band wire technique is performed. By using a 2-mm drill, two
parallel drill holes are placed in a retrograde fashion through the
proximal bony fragment. A 1.6- or 1.8-mm K wire is then advanced
through these holes and out through the quadriceps tendon (Fig. 24.4).
They are advanced until the sharp tip of the K wire is fully within the
proximal bony fragment. The two fracture fragments are then reduced and
held with large, pointed, reduction forceps.
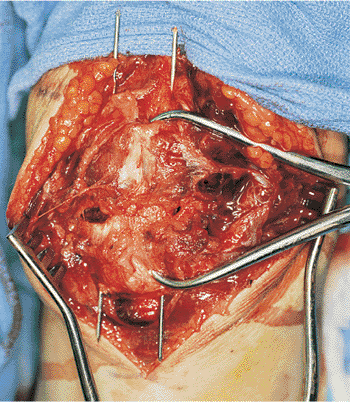
surface is anatomically reduced by inspecting both the anterior
cortical and posterior articular surfaces. The articular surface can be
inspected through the preexisting tears in the retinaculum. If there is
no significant tear in the retinaculum, a small, medial or lateral
arthrotomy should be made to allow inspection or palpation of the
articular surface.
They should be advanced distally at least 1 cm beyond the inferior tip
of the patella. Once again, the adequacy of the reduction should be
checked. A 30-cm segment of 1-mm wire is passed adjacent to the patella
and quadriceps mechanism proximally and distally, passing behind the K
wires and closely approximated to both the proximal and distal poles of
the patella. If this is not achieved, the wire will not obtain adequate
fixation and may loosen, eventually resulting in loss of fixation and
reduction. To facilitate passage of the wire, pass a 16-gauge
angiocatheter through the quadriceps mechanism just above the superior
pole of the patella and behind the K wires (Fig. 24.6). The 1-mm wire is passed through the catheter, which is then removed. The identical technique is performed distally.
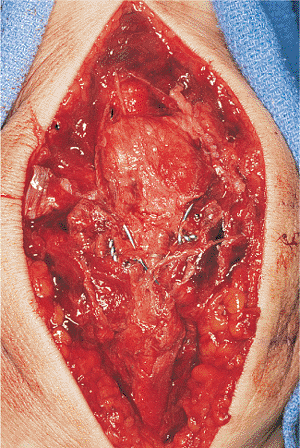
double-loop technique is recommended. A twist is placed in the wire on
its continuous side, and on the contralateral side, the two ends of the
wires are hand tightened and twisted. Excessive wire is removed. By
using either a large needle driver or a large clamp specifically
designed for wire tightening, the two ends of the wire are sequentially
tightened (Fig. 24.7). The technique of wire
tightening is critical. Before twisting, the wire should be tensioned
by lifting up on the clamp. The wire is then gently twisted. This will
ensure that both wires twist around each other rather than one wire
wrapping around the other wire. The wires are sequentially tightened in
this manner until adequate compression has been achieved.
The twisted wire is clipped, and the ends are bent over by using a
large needle driver and gently flattened by using a bone tamp and a
mallet so that they lie close to the superior surface of the bone. The
K wires are bent by stabilizing the wire close to the bone with a
needle driver and then using the wire bender, trying to bend the wire
to 110 degrees. The excess wire is then cut. The remaining wire is then
rotated 180 degrees posteriorly and advanced into the quadriceps
mechanism. If it is not advanced into the quadriceps mechanism, it will
cause excessive irritation, in addition to having an increased chance
of backing out. The distal ends of the wires are then cut so they are
not excessively prominent within the patellar tendon. The retinacular
defects are repaired with absorbable sutures (Figs. 24.9 and 24.10).
 |
|
Figure 24.5.
The transverse fracture has been anatomically reduced by using a pointed fracture-reduction clamp, and the K wires have been advanced antegrade through the distal fragment. The K wires are parallel to each other. |
 |
|
Figure 24.6.
A 16-gauge angiocath is passed through the quadriceps tendon behind the K wires and just superior to the patella. The cerclage wire is being passed through the angiocatheter, which will then be removed. An identical procedure is then performed through the distal pole. |
 |
|
Figure 24.7.
A double-tensioning technique is performed by consecutively tightening each side of the tension band wire. The fracture gap can be seen closed down with this technique. |
 |
|
Figure 24.8.
The tension band wires have been tightened, clipped short, and bent. The K wires have not yet been shortened, and the retinaculum has not yet been repaired. |
 |
|
Figure 24.9.
The final tension-band construct with the K wires cut and bent and buried within the quadriceps and patellar tendon. The retinaculum has been repaired. |
 |
|
Figure 24.10. Alternative transverse incision with final construct visualized through the wound.
|
electrocoagulation. A suction drain is placed in the knee joint.
Closure should be meticulous, including closure of the prepatellar
bursa as a separate layer by using 2-0 Vicryl. The subcutaneous tissue
is closed by using simple inverted 2-0 Vicryl. Skin closure is
dependent on the integrity of the skin. Subcuticular closure gives
excellent cosmetic results but should be reserved for those cases
without skin injuries and only minimal swelling. If there is concern
regarding damage to the skin, nylon sutures should be used. A sterile
dressing is applied consisting of fluffs, Webril, and an Ace wrap. The
patient is placed into either a knee immobilizer or a hinged knee brace
with the knee locked in full extension.
the use of 4-0 cannulated screws with the tension band wire passed
through the cannulated screws and tightened in a standard double-loop
technique (Fig. 24.11). In the case of a
distal-pole patella fracture, the tension-band wire technique can be
used, although the K wires must be placed closer together so that they
both capture the distal fragment. An alternative to this is the use of
retrograde cannulated or standard 4.0 screws in addition to a tension
band technique. With very small fragments, a single screw can be used.
In the case of a stellate fracture, circumferential cerclage wire can
be helpful to bundle the fracture fragments together (Fig. 24.12).
In stellate fractures, it is critical not to violate the soft tissues
around the fragments because this will cause significant disruption of
the fracture fragments.
the resultant stability after osteosynthesis. The extremity is usually
placed in a well-padded compressive dressing and a knee immobilizer or
a hinged knee brace locked in extension. In patients with stable
fixation, knee motion is begun immediately. On the first postoperative
day, the patient is mobilized out of bed to ambulate weight bearing as
tolerated with the knee locked in full extension. The hinges can either
be loosened or the knee immobilizer removed for range-of-motion
exercises. Active flexion and extension are initiated. Quad sets can be
started in the immediate postoperative period. The drain is removed at
48 hours, and the patient is usually discharged home shortly
thereafter. Patients are seen in follow-up in approximately 7 to 10
days for a dressing change and suture removal. If the wound is well
healed, active extension and straight-leg-raising exercises are begun,
and the patient is referred to physical therapy. Patients are seen at 4
to 6 week intervals, and radiographs of the patella are obtained out of
the brace. If there is radiographic evidence of healing, progressive
resistive exercises are started. The patient is progressively weaned
from the brace, depending on the motion and strength. Full
rehabilitation usually takes 4 to 6 months. If there are any symptoms
or signs of loss of fixation during this postoperative period,
range-of-motion exercises are stopped, and the patient is immobilized
and followed up closely.
secure, early range of motion is not possible. The repair should be
protected in either a knee immobilizer or a knee brace with the hinges
locked. The braces are removed only for wound checks and extremity
cleansing. Quad sets can be initiated, but the repair is protected
until there are signs of healing. Range of motion is delayed for 3 to 6
weeks.
complications include hemarthrosis and infection. A hemarthrosis can
usually be avoided by the use of a postoperative suction drain and a
compressive dressing. If the drain was either not used or was removed
prematurely, the hemarthrosis can be aspirated. This is necessary only
if a tense hemarthrosis causes significant pain or limits
rehabilitation.
can usually be avoided by careful timing of surgery and meticulous
surgical techniques in addition to the appropriate
perioperative
antibiotics. If infection develops, it should be aggressively treated
with antibiotics and debridement with drainage. Physical therapy and
early range-of-motion activities should be stopped while treating the
infection. If the infection involves the knee joint, it must be drained
and irrigated surgically. Culture-specific intravenous antibiotics
should be used for 3 to 6 weeks. Internal fixation in general should
not be removed until the fracture is healed.
 |
|
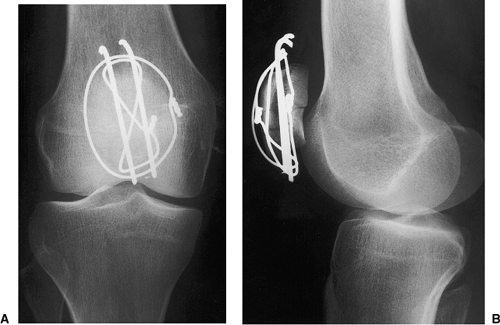
Figure 24.11. A. An AP x-ray of a fractured patella. B. A lateral x-ray of a fractured patella. C. AP x-ray of ORIF in which cannulated screws and wire have been used. D. Lateral x-ray of ORIF in which cannulated screws and wire have been used.
|
complications after surgical repair of patella fractures. This is more
common in complex fracture patterns, in noncompliant
patients,
and when therapy is overly aggressive. If there are signs of loss of
fixation without significant loss of reduction, this can be treated
with immobilization. If there are signs of loss of fixation along with
loss of reduction, then revision internal fixation is indicated.
 |
|
Figure 24.12. A. Postoperative AP and (B)
lateral radiographs of a comminuted patellar fracture fixed with a combination tension-band and cerclage-wire technique. The articular surface has been restored anatomically. |
either failure of fixation or inadequate initial reduction. The
complications can usually be avoided by good reduction and fixation
techniques and close postoperative follow-up. Delayed unions can be
treated with repeated cerclage-wire techniques. Significant malunions
usually require a patellectomy.
common complications after patella fractures. These complications are
more common in severely comminuted fractures and those fractures
requiring prolonged immobilization. The majority of patients can be
treated with aggressive and persistent physical therapy, although an
occasional patient will require manipulation under anesthesia. It is my
preference to do an arthroscopic evaluation at the time of
manipulation. This allows inspection of the patellar surfaces, a direct
lysis of the arthrofibrosis involving the suprapatellar pouch and the
lateral gutters, in addition to adhesions from the fat pad into the
intercondylar notch. Arthroscopic debridement and manipulation should
be followed by aggressive physical therapy to maintain motion and
increase strength. Retropatellar arthrofibrosis and patella baja are
rare but extremely difficult complications to correct and have a
negative effect on patellar function and outcomes.
inadequate reduction of the articular surface or injuries to the
articular surface that occur at the time of injury. In the early
stages, arthroscopy and patellar debridement can decrease some
symptoms. Ultimately in the young patient, a patellectomy may be the
treatment of choice. In the elderly patient who also has involvement of
the medial and lateral compartments, a total knee replacement may be
the treatment of choice.
variable and the causes include severity of injury, fracture pattern,
articular damage, displacement, preexisting disease, accuracy of
reduction, and postoperative regimen. Reliable radiographic (objective)
measurements of
clinical
outcomes do not exist. The best outcomes are seen in patients with
anatomic reductions, restoration of normal biomechanics, and
preservation of the articular surfaces. Loss of all or even part of the
patella may result in loss of extensor strength and function. With the
appropriate surgical and postoperative regimen, good functional results
can be achieved even in complex displaced fractures.
J, Hungerford DS, Zindel M. Patello-femoral joint mechanics and
pathology: 1. Functional anatomy of the patello-femoral joint. J Bone Joint Surg Br 1986;58:287–290.
