Muscle Tone
as the tension in the relaxed muscle, or the resistance to passive
movement when voluntary contraction is absent. Because of resting tone,
normal muscles have slight resistance to passive movement even in the
relaxed state. The inherent attributes of muscle tissue—such as
viscosity, elasticity, and extensibility—contribute to resting tone.
Even apparently relaxed muscle fibers have a constant slight fixed
tension by which they hold their resting position, resist changes in
length, prevent undue mobility at joints, and are in position to
contract when necessary. Resting muscle tone is greatest in the
anti-gravity muscles that maintain the body in an erect position.
is subjective and prone to interexaminer variability. There are no
methods that can measure tone quantitatively. The determination is
based solely on the clinical judgment of the examiner; accurate
assessment of tone requires clinical experience. It is difficult to
separate slightly increased tone from poor relaxation in a tense or
apprehensive patient. Tone is especially difficult to evaluate in
infants, where there may be wide variations in apparent tone on
different examinations, in either health or disease.
cooperative patient. Small talk may help the patient relax. Simple
observation may reveal an abnormality of posture or resting position
that indicates an underlying change in tone. Muscle palpation is
sometimes useful, but well-muscled individuals may have firm muscles
despite normal resting tone, while in other individuals the muscles may
feel flabby despite an underlying hypertonicity. Muscles may have a
firm consistency to palpation because of edema, inflammation, spasm due
to pain, or pseudohypertrophy.
determination of the resistance of relaxed muscles to passive
manipulation as well as the extensibility, flexibility, and range of
motion. Abnormalities of tone are more easily detected in extremity
than in trunk muscles. The limb is moved passively, first slowly and
through a complete range of motion, and then at varying speeds. The
examiner may shake the forearm to and fro and note the excursions of
the patient’s hand, or brace a limb and then suddenly remove the
support, or note the range of movement of a part in response to a
slight blow. Bilateral examination of homologous parts helps compare
for differences in tone on the two sides of the body.
and through partial and full range of motion, documenting the
distribution, type, and severity of any abnormality. Certain specific
maneuvers may be helpful in evaluation of abnormal tone.
are passively flexed at the elbows. With hypotonicity there is
increased flexibility and mobility, and the elbows can be bent to an
angle more acute than normal. With hypertonicity there is reduced
flexibility and passive flexion cannot be carried out beyond an obtuse
angle.
relaxed, eyes closed and attention diverted. The examiner places one
hand under the patient’s occiput and with the other hand briskly raises
the head, and then allows it to drop. Normally the head drops rapidly
into the examiner’s protecting hand, but in patients with
extrapyramidal rigidity there is delayed, slow, gentle dropping of the
head because of rigidity affecting the flexor muscles of the neck. When
meningismus is present there is resistance to and pain on flexion of
the neck.
legs hanging freely. The examiner either extends both legs to the same
horizontal level and then releases them, or gives both legs a brisk,
equal backward push. If the patient is completely relaxed and
cooperative, there will normally be a swinging of the legs that
progressively diminishes in range and usually disappears after six or
seven oscillations. In extrapyramidal rigidity, there is a decrease in
swing time, but usually no qualitative change in the response. In
spasticity, there may be little or no decrease in swing time, but the
movements are jerky and irregular, the forward movement may be greater
and more brisk than the backward, and the movement may assume a zigzag
pattern. In hypotonia, the response is increased in range and prolonged
beyond the normal. In all of these maneuvers a unilateral abnormality
will be more apparent.
and shakes them briskly back and forth, observing the reciprocal motion
of the arms. With extrapyramidal disease, there will be a decreased
range of arm swing on the affected side. With hypotonia, especially
that associated with cerebellar disease, the excursions of the arm
swing will be greater than normal.
and then dropped. In spasticity, there is a delay in the downward
movement of the affected arm, causing it to hang up briefly on the
affected side; with hypotonicity the dropping is more abrupt than
normal. A similar maneuver may be carried out by lifting and then
dropping the extended legs of the recumbent patient.
disease or Sydenham chorea, may cause the hands to assume a
characteristic posture. With the arms and hands outstretched, there is
flexion at the wrists and hyperextension of the fingers (“spooning”),
accompanied by moderate overpronation. With the arms raised overhead
the overpronation is exaggerated with the palms turned outward. This
overpronation phenomenon differs from the pronator drift sign, in which
the overpronation is due to weakness of corticospinal innervated
muscles or increased tone in the pronator muscles.
to passive motion used in the assessment of tone, it is sometimes
useful to observe the reaction to direct percussion of the muscle
belly. The idiomuscular contraction is the brief and feeble contraction
of a muscle belly after it is tapped with a percussion hammer, causing
a slight depression at the site of the stimulus. The contraction
involves only those fibers tapped directly. This is different from the
reaction to muscle stretch, as in elicitation of the deep tendon or
muscle stretch reflexes. Direct muscle percussion causes a contraction
in normal muscles, even when the deep tendon reflex (DTR) is absent.
Myotatic irritability has been defined as both the response to direct
percussion as well as the ability of a muscle to contract in response
to sudden stretch.
muscle is very slight, and in most muscles is seen or felt with
difficulty. The reaction may be more pronounced in wasting diseases,
such as cachexia and emaciation, and in some diseases of the lower
motor neuron. Hyperexcitability to such stimulation occurs in tetanus,
tetany, and certain electrolyte disturbances. Occasionally, after a
muscle is percussed with a reflex hammer, a wave of contraction
radiates along the muscle away from the point of percussion. A small
ridge or temporary swelling may persist for several seconds at the
point of stimulation. This stationary muscle mounding is known as
myoedema. There is no accompanying electrical muscle activity. The
idiomuscular contraction causes a slight depression, myoedema a
rounding up. The mechanism of myoedema is poorly understood, but it is
probably a normal physiological phenomenon. Its presence alone does not
indicate a neuromuscular disorder but the response may be exaggerated
in some circumstances, most notably hypothyroid myopathy. Myotonia is a
persisting contraction following mechanical stimulation of muscle that
is quite different from myoedema.
be elicited. Muscle tenderness on squeezing the muscle belly, or even
with very slight pressure, may cause exquisite pain. Widespread muscle
tenderness to palpation may occur with inflammatory myopathy,
especially polymyositis and dermatomyositis, in some neuropathies, and
in acute poliomyelitis. Focal muscle tenderness occurs with trauma or
overexertion of muscles.
in tone. In addition, there are different varieties of hypotonicity and
hypertonicity. Hypotonicity may develop from disease of the motor unit,
the proprioceptive pathways, cerebellar lesions, and in the choreas.
The muscle may be flaccid, flabby, and soft to palpation. The involved
joints offer decreased resistance to passive movement. The excursion of
the joint may be increased with an absence of the normal “checking”
action on extreme passive motion. If the involved extremity is lifted
and allowed to drop, it falls abruptly. A slight blow causes it to sway
through an excessive excursion. The DTRs are usually decreased or
absent when hypotonia is due to a lesion involving the motor unit or
proprioceptive pathways.
there is invariably some degree of accompanying weakness. The hypotonia
that results from central processes (e.g., cerebellar disease) does not
cause weakness; muscle power is preserved even though hypotonia is
demonstrable on examination. Infantile hypotonia (floppy baby syndrome)
is a common clinical condition in which there is generalized decrease
in muscle tone, typically affecting a neonate. There are numerous
causes, both central and peripheral. Tone may also be decreased when
disease affects the muscle spindle afferent system. Hypotonicity may
occur with various types of cerebellar disease, but is never as severe
as that which occurs with diseases of the lower motor neuron.
Cerebellar hypotonia is not associated with weakness and the reflexes
are not lost, although they may be pendular; there are no
pathologic
reflexes. Muscle tone is of course decreased in deep sleep, coma, and
other states of impaired consciousness. Sudden attacks of impaired
muscle tone in an awake patient occur in akinetic epilepsy and in
cataplexy. In akinetic epilepsy the attacks of sudden loss of muscle
tone occur spontaneously, and the patient falls to the ground. In
cataplexy the attacks are typically precipitated by sudden strong
emotions, such as laughing. Cataplexy is usually a component of
narcolepsy. Sleep paralysis is a state common in narcolepsy, in which a
patient has diffusely decreased tone and is unable to move immediately
after awakening from sleep. The hemiparesis that is present acutely
following hemispheric stroke may be associated with hypotonia (cerebral
or neural “shock”), which gradually evolves into hypertonia with the
passage of time. Some conditions may cause abnormal joint laxity, which
may be confused with muscle hypotonia (e.g., Ehlers-Danlos syndrome).
routine feature of lesions that involve the corticospinal tract after
the acute stage. It can occur with diffuse cerebral disorders, with
disease involving the extrapyramidal system, with disease of spinal
cord interneurons (e.g., stiff person syndrome), and even with muscle
disorders in continuous muscle fiber activity syndromes.
tone to passive movement that occurs primarily with lesions that
involve the basal ganglia. There is a fairly constant level of
increased tone that affects both agonist and antagonist and is equally
present throughout the range of motion at a given joint. Both flexor
and extensor muscles are involved, with resistance to passive movement
in all directions. The increased tone is equally present from the
beginning to the end of the movement and does not vary with the speed
of the movement. This type of rigidity is referred to as “lead-pipe.”
The involved muscles may be firm and tense to palpation. After being
placed in a new position, the part may remain there, causing the limbs
to assume awkward postures.
hypertonicity. As the part is manipulated, it seems to give way in a
series of small steps as if the limb were attached to a heavy cogwheel
or ratchet. The jerky quality of the resistance may be due to tremor
superimposed on lead-pipe rigidity. Cogwheel rigidity is most commonly
encountered in Parkinson disease and other parkinsonian syndromes. It
appears first in proximal muscles and then spreads distally. Any muscle
may be affected, but there is predominant involvement of neck and trunk
muscles and the flexor muscles of the extremities. The rigidity of
extrapyramidal disease may be brought out by the head-dropping,
shoulder-shaking, and similar tests. The rigidity on one side may be
exaggerated by active movements of the contralateral limbs.
hypokinesia and bradykinesia, but no real paralysis. With repeated
active movements there is a gradual decrease in speed and amplitude.
This may be brought out by having the patient rapidly open and close
the eyes or mouth, open and close the hand, or oppose finger and thumb.
Patients also have loss of associated movements. Patients may also show
slowness of starting and limitation of the amplitude of movement, loss
of pendulousness of the arms and legs, inability to carry out rapid
repeated movements or to maintain two simultaneous voluntary movements,
and impairment of associated movements, such as swinging of the arms
when walking.
that is often a manifestation of diffuse frontal lobe disease. It has
been divided into inhibitory paratonia and facilitory paratonia.
Gegenhalten is a form of rigidity in which the resistance to passive
movement seems proportional to the vigor with which the movement is
attempted. The resistance of the patient increases in proportion to the
examiner’s efforts to move the part; the harder the examiner pushes,
the harder the patient seems to push back. It seems as though the
patient is actively fighting, but the response is involuntary. It is
said that the severity of gegenhalten can be judged by the loudness of
the
examiner’s
exhortations to relax. In the limb placement test, the examiner
passively lifts the patient’s arm, instructs the patient to relax,
releases the arm, and notes whether or not it remains elevated. The arm
remaining aloft, in the absence of parkinsonism or spasticity,
indicates paratonia. In facilitory paratonia, the patient cooperates
too much. The patient actively assists the examiner’s passive
movements, and the limb may continue to move even after the examiner
has released it.
pathways. The hypertonicity to passive movements differs from that of
rigidity because it is not uniform throughout the range of movement,
and it varies with the speed of movement. In addition, rigidity tends
to affect all muscles to about the same degree, whereas the hypertonia
of spasticity varies greatly from muscle to muscle. In spasticity, if
the passive movement is made slowly, there may be little resistance.
But if the movement is made quickly, there will be a sudden increase in
tone partway through the arc, causing a catch or a block as though the
muscle had impacted a stop. The relationship of the hypertonus to the
speed of movement is a key feature distinguishing spasticity from
rigidity. In the upper extremity it is useful to look for spasticity
involving the pronator muscles. With the patient’s elbow flexed to
about 90 degrees and the forearm fully pronated, the examiner slowly
supinates the patient’s hand. Unless spasticity is severe, there will
be little or no resistance to this slow movement. If, after several
slow repetitions, the examiner supinates the patient’s hand very
quickly, there will be sudden resistance at about the midrange of
movement, referred to as a “pronator catch.” The catch will then relax,
and the supination movement can be completed. When hypertonus is
severe, this maneuver may elicit pronator clonus.
to detect lower-extremity spasticity. With hands behind the knee, the
examiner slowly flexes and extends the knee of the supine and relaxed
patient. With adequate relaxation the foot remains on the bed. After
several slow repetitions, from the position of full extension, the
examiner abruptly and forcefully pulls the knee upward. When tone is
normal, the foot will scoot back, remaining in contact with the bed.
When there is spasticity, the foot flies upward in a kicking motion
(spastic kick). In the heel- or foot-dropping test, the examiner holds
the patient’s leg flexed at the knee and hip, one hand behind the knee,
the other supporting the foot. The foot is suddenly released. Normally
its descent is smooth, but when there is spasticity in the quadriceps
muscle the foot may hang up and drop in a succession of choppy
movements.
palpation. The range of movement of spastic extremities, and the degree
of hypertonicity, often vary between examinations. No devices for
quantitating spasticity exist, and clinical evaluation remains the most
useful tool. The Ashworth scale is used to quantitate spasticity on a
scale from 1 (no increase in muscle tone) to 5 (affected part rigid in
flexion or extension). In the presence of spasticity, the DTRs are
exaggerated and pathologic reflexes such as the Babinski and Chaddock
signs can often be elicited. Clonus is often present. There may be
abnormal associated movements.
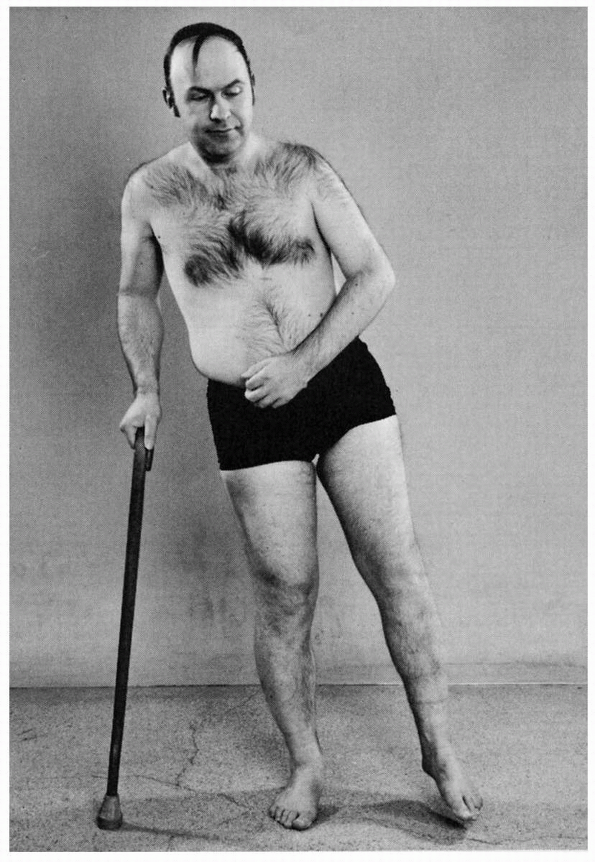
sustained contraction of specific groups of muscles. With hemiparesis
or hemiplegia, spasticity is most marked in the flexor and pronator
muscles of the upper and the extensor muscles of the lower extremity;
this causes a posture of flexion of the arm and extension of the leg,
the characteristic distribution in cerebral hemiplegia (Figure 19.1).
The arm is adducted, flexed at the elbow, and the wrist and fingers are
flexed; there may be forced grasping. The lower extremity is extended
at the hip, knee, and ankle, with inversion and plantar flexion of the
foot; there may be marked spasm of the hip adductors. There is more
passive resistance to extension than to flexion in the upper
extremities, and to flexion than to extension in the lower extremities.
With bilateral lesions the increased tone of the hip adductors causes a
scissors gait, in which one leg is pulled toward the other as each step
is taken. Although spasticity in the lower extremities usually affects
the extensors most severely, in some patients with severe myelopathy or
extensive cerebral lesions, there is marked hypertonicity in the flexor
muscles, drawing the legs into a position referred to as paraplegia in
flexion.
 |
|
FIGURE 19.1 • Left hemiparesis of 15 years’ duration. The patient circumducts his left leg as he begins walking.
|
respects similar to extrapyramidal rigidity and may be physiologically
related. There is a waxy or lead-pipe type of resistance to passive
movement that may be accompanied by posturing, bizarre mannerisms, and
evidence of psychosis. It may be possible to mold the extremities into
any position, in which they remain indefinitely.
and sustained contraction of the extensor muscles of all four
extremities; in decorticate rigidity there is flexion of the elbows and
wrists with extension of the legs and feet. Similar generalized
rigidity with neck extension can occur with severe meningismus
(opisthotonos), as well as in the tonic phase of a generalized seizure.
braced to protect against injury or in response to pain. It is often
difficult to differentiate between tension that is truly volitional and
that which is unconscious or involuntary, especially when related to
excitement, alarm, pain, or fatigue. Tense, apprehensive individuals
may show increased muscular tension at all times, and may have
exaggerated tendon reflexes. The reflex exaggeration is one of range of
response, and the latent period is not shortened. Conversely, the
reflexes may be suppressed because the semivoluntary contraction
prevents normal movement.
resemble voluntary rigidity. Rigidity of psychogenic origin may be
bizarre and may simulate any type of hypertonicity. Hysterical rigidity
may simulate decerebration or catatonia. It may be extreme, with neck
retraction and opisthotonos, the body resting with only the head and
heels upon the bed (arc de cercle).
response to afferent impulses, particularly pain. Muscle spasm is a
state of sustained involuntary contraction accompanied by muscle
shortening. The abnormal contraction is visible and palpable. Common
examples of reflex muscle spasm are the board-like abdomen of acute
abdominal disorders, rigidity of the neck and back in meningitis, and
the localized spasm in the extremities following trauma. Reflex
rigidity may follow other sensory stimuli, such as cold. Muscle
contracture may follow prolonged spasm. In some metabolic myopathies
(e.g., McArdle disease), painful muscle cramps and spasms are brought
on by exercise; the muscle cramp is a physiologic form of contracture
due to abnormal metabolism, and is not accompanied by electrical
activity.
occur in many different conditions. Tone is usually normal when the
muscles are relaxed, but contraction produces a temporary involuntary
tonic perseveration of muscle contraction with slow relaxation. Sudden
movements may cause marked spasm and inability to relax. In grip
myotonia, the patient has difficulty letting go of an object after
gripping it strongly. The myotonia usually decreases with repetition of
the movement (warm-up phenomenon). In rare instances the myotonia
increases with repetitive movement (paradoxical myotonia). Percussion
myotonia is elicited by tapping on the muscle. Percussion over the
thenar eminence produces a prolonged tonic abduction and opposition
movement lasting several seconds, over which the patient has no
control. Tapping over the extensor digitorum communis to the middle
finger causes the finger to snap into extension, after which it slowly
falls over a much longer period of time than normal. Percussion
myotonia can also be elicited over other muscles. Oblique elimination
with a penlight may help to make the slowly disappearing depression or
dimple more visible. Percussion of a tongue blade placed transversely
on edge across the tongue may produce a segmental myotonic contraction
that constricts the tongue circumferentially (napkin-ring sign).
