CHAPTER 16 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
Section – Surgical Techniques of the Rotator Cuff
CHAPTER 16 – Arthroscopic Rotator Cuff Repair: Single-Row Technique
Brian J. Cole, MD, MBA
Arthroscopic treatment of rotator cuff tears has become a routine procedure following a general trend toward less invasive surgery. Proponents of this technique emphasize the decreased risk of complications, such as infection, stiffness, and deltoid avulsions; critics mention the lack of long-term studies, the controversy about the strength of fixation, and the technical challenge of all-arthroscopic repair of large tears for nonspecialists. The goal of arthroscopic rotator cuff repair is to relieve pain and to improve shoulder function while addressing all concomitant intraarticular disease in a minimally invasive manner. Many technical aspects of arthroscopic rotator cuff surgery are evolving as our understanding of failure mechanisms and patient outcomes grows. Many issues remain controversial, such as the need for routine acromioplasty, management of incomplete tears, optimal suture management, and anchor configuration (single row versus double row). The successful arthroscopic treatment of rotator cuff tears depends on recognition of tear patterns, appropriate use of releases, secure fixation with restoration of the footprint under minimal tension, and proper rehabilitation. This and the following chapter provide an overview of the indications, surgical technique, rehabilitation, and results of arthroscopic rotator cuff repair. To provide a balanced perspective, we present the standard single-row technique here;
Chapter 17
discusses double-row and suture bridge techniques, which we currently use in all but small and uncomplicated tears.
Factors Affecting Surgical Indication
Factors Affecting Surgical Planning
Magnetic Resonance Imaging and Magnetic Resonance Arthrography (
Fig. 16-1
)
|
|
|
|
Figure 16-1 |
Partial tears generally involve less than 50% of the tendon thickness and do not lead to retraction of the muscle. On the basis of location within the tendon, partial tears are classified as intrasubstance, bursal sided, or articular sided (undersurface); the last constitutes approximately 90% of partial tears. Weakness is uncommon in partial-thickness tears but can arise from pain, which is often greater than in complete tears.
In contrast, full-thickness tears represent complete discontinuity of rotator cuff fibers, resulting in communication between the articular and bursal spaces. The extent of the lesion on imaging studies is described in both anteroposterior and mediolateral directions; 1 cm is generally considered small, 1 to 3 cm medium, 3 to 5 cm large, and more than 5 cm massive. Tears that involve two or more tendons are automatically classified as massive and occasionally require more complex reconstruction. Larger tears with chronic tendon retraction lead to fatty degeneration of the associated muscle that may be irreversible, making results of direct repair less predictable.
Rotator cuff tears can be further classified on the basis of tear configuration. Crescentic, L-shaped, and U-shaped tears have been described, all of which require slight modifications in repair technique (see later).
Indications and Contraindications
The primary indication for surgical treatment is persistent pain unresponsive to nonoperative measures or, more rarely, acute weakness due to a traumatic tear in a younger individual; poor function and diminished strength are relative indications with less reliable outcomes. The ideal surgical candidate is a compliant patient with few comorbidities and adequate tendon quality who can follow a rigorous postoperative rehabilitation program. All patients should recognize that the results are dependent on many factors, including size and retraction of the tear, tissue quality, muscle degeneration and atrophy, and overall health of the patient.
Contraindications include active or recent infection, medical comorbidities that preclude surgery, and advanced glenohumeral arthritis. Relative contraindications may include significant muscle degeneration and fixed superior migration of the humeral head.
Arthroscopic rotator cuff repair is usually performed under general anesthesia with endotracheal intubation or laryngeal mask ventilation, regional anesthesia through an interscalene nerve block, or a combination thereof. The decision is made in collaboration with the patient and anesthesiologist. Regional anesthesia has been found especially helpful for pain management in outpatient procedures because its effects commonly continue for several hours. Preemptive analgesia with anti-inflammatory drugs given before the operation is increasingly being used and is usually continued for several days postoperatively. This treatment will have to be re-evaluated in light of emerging reports of potential detrimental effects of anti-inflammatory drugs on early tendon healing.
On the basis of the surgeon’s preference, the patient is placed in either the beach chair or lateral decubitus position. Whereas each position has unique advantages and limitations, both are acceptable choices for arthroscopic rotator cuff repair.
Surgical Landmarks, Incisions, and Portals
| • | Clavicle | |
| • | Acromion | |
| • | Acromioclavicular joint | |
| • | Coracoid process | |
| • | Scapular spine |
| • | Anterior portal | |
| • | Posterior portal | |
| • | Standard lateral portal | |
| • | Posterolateral portal |
A portal that we have recently described and find particularly useful is the posteromedial portal, which is placed approximately 3 cm medial to the standard posterior portal. This portal allows in-line passage of a suture-retrieving instrument (i.e., penetrating suture grasper).
When it is necessary to achieve ideal anchor orientation, the surgeon can make accessory portals that deviate from the standard portals. These portals should be kept as small as possible to minimize trauma to the deltoid muscle and be used only for percutaneous anchor placement without the use of a cannula.
| • | Deltoid muscle and axillary nerve with lateral portals | |
| • | Musculocutaneous nerve with anterior portals | |
| • | Suprascapular nerve with Neviaser portal |
Examination Under Anesthesia and Diagnostic Arthroscopy
Before preparation and draping, the shoulder joint is put through a range of motion to assess for stiffness, which, if significant, requires additional capsular releases.
A brief diagnostic glenohumeral arthroscopy is performed through standard anterior and posterior portals to evaluate potentially associated pathologic processes, such as biceps tendinitis, chondral damage, and labral disease. After the rotator cuff tear is visualized, it is often helpful to mark the exact location by percutaneous passage of a suture through the tear, especially in small and partial tears, which can be difficult to localize from the subacromial space.
Specific Steps (
Box 16-1
)
After routine glenohumeral arthroscopy to evaluate for and address any associated pathologic process, the arthroscope is placed into the subacromial space through either a standard posterior portal or a separate posterolateral portal.
| Surgical Steps | |||||||||||||||
|
1. Acromioplasty and Bursectomy
Currently, many surgeons routinely perform an acromioplasty before rotator cuff repair, which can improve visualization and may reduce potential external compression of the cuff from an anterolateral spur. A complete release of the coracoacromial ligament should be avoided, especially in large and massive rotator cuff tears, because it provides a restraint to superior escape of the humeral head in the rotator cuff–deficient shoulder. An adequate acromioplasty, however, can easily be performed even without complete release of the coracoacromial ligament. A bursectomy and limited acromioplasty are performed with an arthroscopic bur and radiofrequency ablation device through the lateral portal with visualization from posteriorly, or vice versa; this is described in more detail in
Chapter 23
. Next, the footprint on the greater tuberosity is prepared to obtain an optimal environment for healing (
Fig. 16-2
). This can be performed with the shaver or a bur; however, extensive decortication has largely been abandoned because it does not appear to improve healing and can compromise secure anchor fixation.
|
|
|
|
Figure 16-2 |
Adhesions frequently form between retracted rotator cuff tears and surrounding tissues. It is necessary to release these adhesions before attempting to reduce and repair the cuff to the footprint. To assess cuff mobility, the surgeon can apply traction to the tendon edge with either a grasper or traction suture through the lateral portal. A thorough release should be performed if the tendon edge cannot be reduced to the footprint in a tension-free manner. We prefer to visualize through the posterior portal while using a Bankart elevator or electrothermal device through the lateral and anterior portals to release any adhesions. Most commonly, it is necessary to release both upper and lower aspects of the rotator cuff; adhesions form superiorly with the acromion and inferiorly with the capsulolabral complex, glenoid, and glenoid neck. In long-standing tears, where the cuff is adherent to the glenoid neck, release of the capsule adjacent to the superior and posterior labrum is particularly useful. However, the suprascapular nerve and vessels are at risk during this dissection, which should not extend farther than 1 cm medial to the glenoid rim. Anterior releases along the rotator interval can separate adhesions between the supraspinatus and the coracoid and subscapularis. Rarely, posterior release between the supraspinatus and infraspinatus is required.
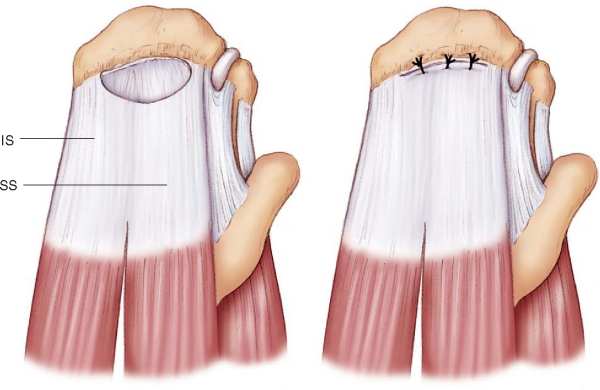
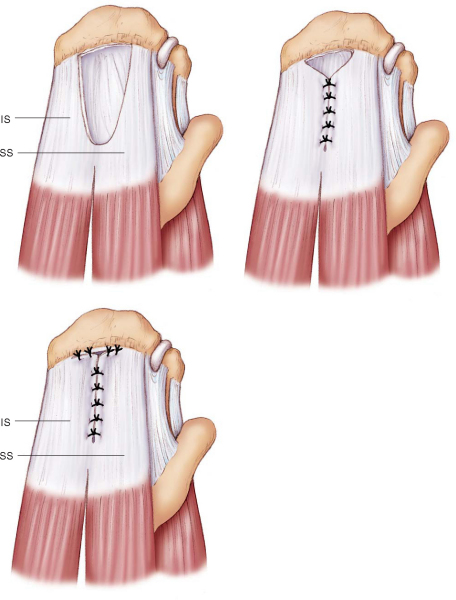
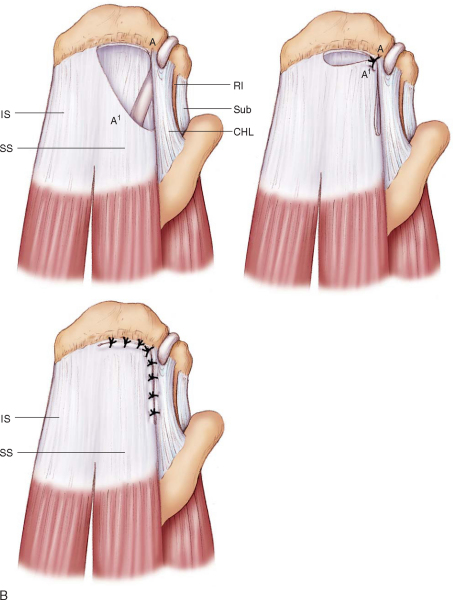
3. Tear Patterns and Margin Convergence
Several tear configurations have been described. Crescentic tears are more commonly found acutely or subacutely and usually are easily mobilized and repaired directly to bone with suture anchors (
Fig. 16-3
). U-shaped tears are generally larger and may require side-to-side repair (i.e., margin convergence) to reduce tear size and decrease tension on the leading edge, thus allowing a more stable repair to the tuberosity (
Fig. 16-4
). L-shaped tears are best addressed with a side-to-side repair of the longitudinal limb before the horizontal limb is secured to bone with suture anchors (
Fig. 16-5
).
|
|
|
|
Figure 16-3 (Redrawn from Lo IK, Burkhart SS. Arthroscopic repair of crescent-shaped, U-shaped, and L-shaped rotator cuff tears. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004:217-240.) |
|
|
|
|
Figure 16-4 (Redrawn from Lo IK, Burkhart SS. Arthroscopic repair of crescent-shaped, U-shaped, and L-shaped rotator cuff tears. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004:217-240.) |
|
|
|
|
Figure 16-5 (Redrawn with modification from Lo IK, Burkhart SS. Arthroscopic repair of crescent-shaped, U-shaped, and L-shaped rotator cuff tears. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004:217-240.) |
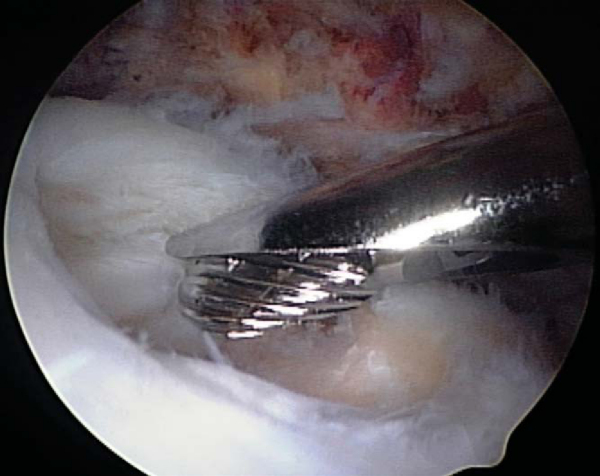
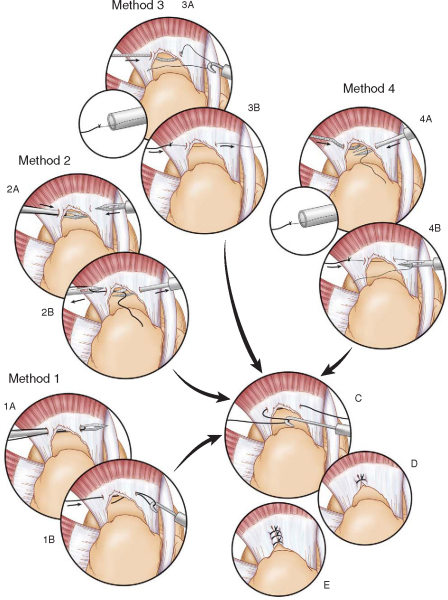
Side-to-side repairs are performed in a medial to lateral progression with free sutures that can be passed through the tendon substance by a variety of instruments and techniques (
Fig. 16-6
). Our preference is to use a straight penetrating suture grasper when working in the posterior two thirds of the cuff as well as during repair of the more medial extent of the side-to-side component of a tear. Laterally and anteriorly, a shuttle-type suture-passing device is more effective. Sutures should generally be tied directly after passing and before anchor placement to reduce the risk of suture entanglement (
Fig. 16-7
).
|
|
|
|
Figure 16-6 |
|
|
|
|
Figure 16-7 |
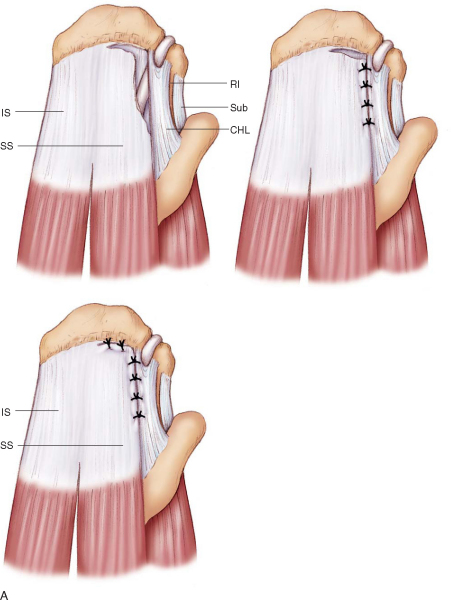
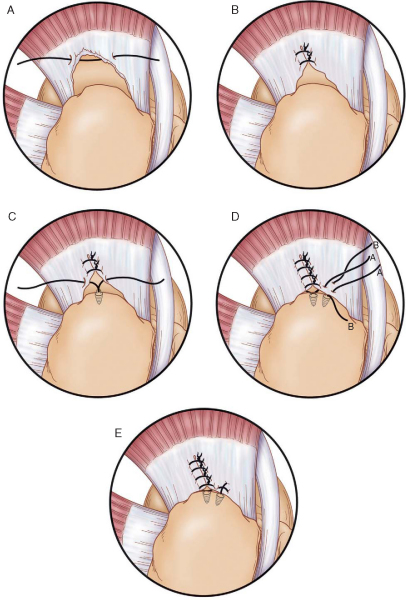
4. Footprint Preparation and Anchor Placement
In general, suture anchors are placed in the medial aspect of the footprint for a single-row technique; they should be placed in a systematic fashion to help with suture management, often from posterior to anterior. After placement, the corresponding sutures are stored in unused cannulas to avoid entanglement. Anchor placement can be performed either through the standard portals or through additional percutaneous stab incisions as needed to obtain the optimal anchor orientation of 45 degrees, tilted laterally (dead man’s angle).
For the repair of large crescentic tears or U-shaped tears after margin convergence (
Fig. 16-8A and B
), we place our initial anchor medial (in the frontal plane) and central (in the sagittal plane), approximately 5 mm off the articular margin. We consecutively retrieve all four suture limbs with a penetrating suture grasper, thus forming two independent horizontal mattress sutures, which further converge the two leaves of the tear (
Fig. 16-8C
). Next, we place at least two additional anchors, one more posterior and lateral to the first, and the final anchor is typically placed just behind the bicipital groove. A combination of horizontal mattress and simple stitches can be used, constructing a modified Mason-Allen equivalent (
Fig. 16-8D and E
).
|
|
|
|
Figure 16-8 . B, The sutures are tied individually after passing. C, A double-loaded anchor is placed (only one suture is depicted), and one limb from each suture is retrieved through the anterior and posterior leaves. These sutures are tied, effectively forming additional, but anchored, margin convergence sutures. D, Additional anchors are placed anterior and posterior to the first anchor. Both limbs of one suture (A) are passed through the tendon, but only one limb of the other suture (B) is passed. E, Suture limbs A are tied as a horizontal mattress suture, then suture limbs B are tied over the top as a simple stitch, forming a modified Mason-Allen equivalent. The procedure is repeated for the remaining anchor to secure the other leaf of the tear. |
The senior author prefers a low-profile penetrating suture grasper for the posterior cuff in combination with a 45-degree ipsilateral (i.e., right curve for right shoulder) curved suture shuttle device for the more anterior aspect of the tear. Alternatively, various devices are available that can be passed with a loaded suture through the anterolateral or lateral portal (while viewing from posteriorly) and antegrade directly through the lateral tendon edge. Whether a shuttle or a suture-passing device is used, only one suture limb should be kept within a cannula at any given time to avoid entanglement.
Most tears of the supraspinatus and infraspinatus tendons retract in a posteromedial rather than purely medial direction. Therefore, sutures should be placed more posteriorly into the tendon relative to the anchor to properly restore the tendon edge to its original, more anterior insertion site.
Arthroscopic knot tying is a crucial technical aspect of a successful repair. Although many different sliding and nonsliding techniques have been described, the senior author prefers simple half-hitches on alternating posts. This reliable and simple method does not require sliding of the suture through the tissue, which has been associated with suture cutout. Irrespective of the technique used, care must be taken to ensure that the knot tightly reduces the tendon to the anchor and bony bed of the footprint to allow healing.
Postoperative rehabilitation is of crucial importance in achieving a good outcome. Postoperatively, patients are placed in a sling with a supportive abduction pillow, which is worn at all times except for showering and therapy. The rehabilitation program is divided into three phases on the basis of the progression of tendon healing.
Phase 1 (weeks 0-4): Exercises are restricted to passive range of motion only. Restrictions are based on intraoperative assessment of construct stability, commonly limiting passive external rotation to 40 degrees and forward flexion to 90 degrees. Therapeutic exercises during this phase include pendulum exercises; elbow, wrist, and hand range of motion; grip strengthening; and isometric scapular stabilization.
Phase 2 (weeks 4-8): The sling is discontinued, and range of motion is progressed to 140 degrees of forward flexion, 40 degrees of external rotation, abduction to 60 to 80 degrees, and posterior capsular stretching to maintain or to improve internal rotation. Therapeutic exercises are advanced to gentle active-assisted exercises in the supine position with progression to active exercises with resistance at 6 weeks. Deltoid and biceps strengthening is initiated, with the arm kept close to the side to minimize lever arm forces on the rotator cuff.
Phase 3 (approximately weeks 8-12) is characterized by progression to full motion, as tolerated. Scapular strengthening is continued, and internal and external rotation isometric exercises are added to the program. During the final phase of rehabilitation, sport-specific activities are initiated, flexibility is maintained, and strengthening exercises are continued. Formal physical therapy is usually discontinued after approximately 4 months, with return to unrestricted athletic activities at 6 months.
Complications are relatively rare, with reported infection rates of less than 1%. Significant fluid extravasation with subcutaneous edema has been implicated in airway obstruction. More common are hypotensive episodes in up to 20% of patients undergoing shoulder arthroscopy with interscalene block in the sitting position. These potentially serious episodes are reportedly caused by activation of the Bezold-Jarisch reflex and can be addressed by preemptive beta-blockade.
The incidence of minor complications related to edema from fluid extravasation is unknown and is typically inconsequential. However, there have been reports of subcutaneous emphysema causing serious pulmonary complications during shoulder arthroscopy, which emphasizes the need for continued monitoring of the patient’s shoulder and neck for excessive swelling or crepitation.
Clinical outcomes after arthroscopic rotator cuff repair have been comparable to those of open reconstruction, despite the fact that radiologic investigations have demonstrated a comparatively higher rate of recurrent tears on magnetic resonance imaging followup (
Table 16-1
). Between 77% and 98% of patients are satisfied with their outcome after rotator cuff repair, with excellent pain relief and functional improvement in more than 80%. Benefits of arthroscopic repair versus open or mini-open techniques include smaller incisions with less soft tissue dissection, avoidance of deltoid detachment, improved visualization of the entire glenohumeral joint for evaluation and treatment of concomitant pathologic processes, and decreased postoperative pain. However, arthroscopic repair has been associated with a significant rate of recurrent tears.[2] Our results have demonstrated a recurrent tear rate of up to 47% at 2 years on magnetic resonance imaging examination. Nonetheless, clinical results do not seem to suffer in these patients. We have found significantly improved functional and pain scores, as well as improved strength, even in the setting of a recurrent tear; patients rated the postsurgical shoulder at 85% of the normal, contralateral side.
| Author | Followup | Patients | Outcome |
|---|---|---|---|
| Youm et al[6] (2005) | 3 years | 42 | 95% good–excellent results |
| Wilson et al[5] (2002) | 5 years | 100 | 88% good–excellent results |
| Murray et al[4] (2002) | 3.3 years | 48 | 95% good–excellent results |
| Burkhart et al[1] (2001) | 3.5 years | 59 | 95% good–excellent results |
| Gartsman et al[3] (1998) | 2.5 years | 73 | 84% good–excellent results |
1.
Burkhart SS, Danaceau SM, Pearce CE: Arthroscopic rotator cuff repair: analysis of results by tear size and repair technique—margin convergence versus direct tendon-to-bone repair.
Arthroscopy 2001; 17:905-912.
2.
Galatz LM, Ball CM, Teefey SA, et al: The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears.
J Bone Joint Surg Am 2004; 86:219-224.
3.
Gartsman GM, Khan M, Hammerman SM: Arthroscopic repair of full-thickness tears of the rotator cuff.
J Bone Joint Surg Am 1998; 80:832-840.
4.
Murray Jr TF, Lajtai G, Mileski RM, Snyder SJ: Arthroscopic repair of medium to large full-thickness rotator cuff tears: outcome at 2- to 6-year followup.
J Shoulder Elbow Surg 2002; 11:19-24.
5.
Wilson F, Hinov V, Adams G: Arthroscopic repair of full-thickness tears of the rotator cuff: 2- to 14-year followup.
Arthroscopy 2002; 18:136-144.
6.
Youm T, Murray DH, Kubiak EN, et al: Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcomes and patient satisfaction.
J Shoulder Elbow Surg 2005; 14:455-459.
Burkhart et al., 1996.
Burkhart SS, Athanasiou KA, Wirth MA: Margin convergence: a method of reducing strain in massive rotator cuff tears.
Arthroscopy 1996; 12:335-338.
Gartsman and O’Connor, 2004.
Gartsman GM, O’Connor DP: Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: a prospective, randomized study of one-year outcomes.
J Shoulder Elbow Surg 2004; 13:424-426.
Lo and Burkhart, 2003.
Lo IK, Burkhart SS: Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff.
Arthroscopy 2003; 19:1035-1042.
Loutzenheiser et al., 1995.
Loutzenheiser TD, Harryman 2nd DT, Yung SW, et al: Optimizing arthroscopic knots.
Arthroscopy 1995; 11:199-206.