Achondroplasia
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Achondroplasia
Achondroplasia
Paul D. Sponseller MD
Description
-
Achondroplasia is the most common skeletal dysplasia.
-
Characteristics:
-
Patient height <4.5 feet at maturity
-
The greatest shortening occurs in the proximal humerus and femur (1).
-
Hypoplasia of the midface and frontal bossing may be present (Fig. 1).
-
Arthritis is rarely seen, but spinal stenosis is the most serious possible complication.
-
Affects the skeletal and neurologic systems
-
Its features are immediately evident at birth, but life expectancy is not substantially altered in the heterozygote:
-
Skeleton: Ligamentous laxity, undergrowth of long bones
-
Neurologic: Stenosis of the foramen magnum in infancy or the lumbar spine near maturity
-
Skeletal dysplasia: Rhizomelic short stature
-
-
Epidemiology
Incidence
-
The incidence of spinal stenosis and degenerative disc disease increases with age.
-
It affects males and females equally.
Prevalence
1 per 15,000 population (1)
Risk Factors
-
Parental age >37 years
-
Achondroplastic parent
Genetics
-
Autosomal dominant
-
Acquired by most patients (70%) as a new mutation (1,2)
-
Homozygous patients (with 2 affected parents) usually die.
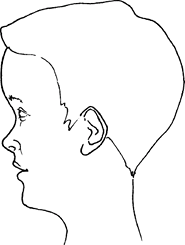 Fig. 1. Frontal bossing and midface hypoplasia are seen in achondroplasia.
Fig. 1. Frontal bossing and midface hypoplasia are seen in achondroplasia.
Pathophysiology
-
Growth plates show decreased cellular organization and activity, resulting in a defect in endochondral osteogenesis.
-
Bones and other tissues are otherwise normal.
-
Growth plates are of normal width;
microscopically, the normal, orderly arrangement of cartilage cells
into columns is defective. -
Membranous bone formation, which accounts for circumferential growth of the shafts of the long bones, proceeds normally.
-
Changes can be recognized radiographically as early as 3 months of gestation.
Etiology
-
Achondroplasia results from a defect in the fibroblast growth factor receptor-3 protein (1).
-
The pathologic process begins in utero: The epiphyseal cartilage plate growth is slowed and disordered, with a resulting decrease in longitudinal growth.
Associated Conditions
-
Spinal stenosis
-
± Hydrocephalus
-
Overweight
Signs and Symptoms
-
Disproportionately short stature, long trunk, and rhizomelic shortening of the limbs are evident at birth (Fig. 2).
-
Large head, with a prominent forehead and parietal bossing
-
Midfacial hypoplasia
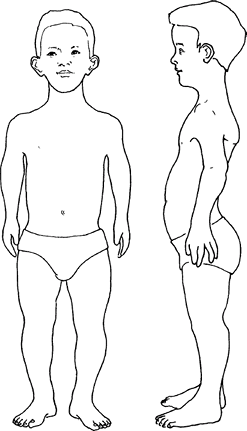 Fig.
Fig.
2. Characteristic features in achondroplasia include rhizomelic
shortening (thighs and upper arms most markedly shortened) and
increased lumbar lordosis. -
Initially, the legs appear straight, but genu varum may develop with growth.
-
Short, broad, and stubby digits (Fig. 3)
-
Restricted elbow extension (but little functional importance)
-
Excessive lumbar lordosis and anterior pelvic tilt, as well as a waddling gait
-
Stenosis of the lumbar spine, prolapse of
the intervertebral discs, osteophytes, and deformed vertebral bodies
may compress the spinal cord and nerve roots. -
Adult height ranges from 42–56 inches.
History
-
A developmental history should be taken.
-
Although milestones are not met at the usual times, norms are available for this condition.
-
In many cases, stenosis of the foramen magnum resolves spontaneously.
-
Physical Exam
-
Head: Frontal bossing; midface hypoplasia
-
Spine: Exaggerated lumbar lordosis; possible thoracolumbar kyphosis
-
Extremities:
-
Short, especially proximally in the humerus and femur
-
Muscular appearance
-
-
Elbow flexion contracture ± dislocated radial head
-
Space between long and ring fingers, giving appearance of ‘trident’ hand (3 groups of digits)
-
Bowed (varus) knees common; varus–valgus laxity and hyperextension often are seen in childhood.
-
Lumbar stenosis in adults, possibly producing motor weakness in ankles, feet, and bladder function
-
Cervical or thoracic stenosis, possibly causing hyperreflexia
Tests
Lab
-
No characteristic laboratory findings
-
DNA testing is not used clinically.
Imaging
-
Radiography:
-
Skull:
-
A shortened skull base, a large cranium
with prominent frontal and occipital areas, and superimposition of the
spheno-occipital synchondrosis over the mastoid -
Small foramen magnum
![]() Fig. 3. A characteristic separation between the 3rd and 4th fingers leads to the “trident hand” of achondroplasia.
Fig. 3. A characteristic separation between the 3rd and 4th fingers leads to the “trident hand” of achondroplasia.
-
-
Lumbar spine:
-
Decreased interpedicular distance, spinal stenosis, and posterior scalloping of the vertebral bodies
-
Thoracolumbar kyphosis, commonly seen in
infancy, usually disappears with ambulation and is replaced by an
exaggerated lumbar lordosis.
-
-
Pelvis: Broad with wide, “square” iliac
wings, small and deep greater sciatic notches, and horizontal superior
acetabular margins
P.9 -
-
MRI:
-
Obtain of the head and neck if milestones are delayed beyond the achondroplastic norms
-
Diagnostic Procedures/Surgery
-
Sleep studies are possibly indicated for infants with developmental delay.
-
Routine genetic testing is not indicated.
Pathological Findings
None
Differential Diagnosis
-
Pseudoachondroplasia: Normal facial appearance; irregular epiphyses of hips and knees
-
Hypochondroplasia: Height usually >54 inches, no spinal stenosis, no caudal approximation of the pedicles
General Measures
-
No effective treatment for the cartilage growth difference is available.
-
Occasionally, osteotomy is required to correct specific limb deformities (1,2).
-
In adults, low back pain may require symptomatic measures.
-
Neurologic complications, including
hydrocephalus, nerve root compression, spinal stenosis, and paraplegia,
may necessitate surgery. -
Foramen magnum decompression is performed for severe infantile stenosis (2).
-
Thoracolumbar kyphosis is monitored, and
patients are treated with a brace if the condition persists beyond the
age of 2–3 years. -
Laminectomy is indicated for severe
spinal stenosis and should include fusion for a patient with severe
kyphosis or skeletal immaturity. -
Restriction from sports is not usually necessary.
-
Custom chairs and automobile hand controls are helpful.
-
Close follow-up for any signs of neurologic compromise is important.
-
Children with achondroplasia should not
be evaluated against normal developmental milestones but, rather,
against standards developed for children with the condition. -
Motor skills often are delayed because of the physical difficulties imposed by short limbs and hypotonia.
-
Cognitive skills usually are attained at the expected ages.
Special Therapy
Physical Therapy
A therapist may be helpful in adapting a child to the environment or monitoring developmental progress.
Surgery
-
Tibial valgus-derotation osteotomy:
-
Usually indicated for persistent varus and torsion of the knees; internal tibial torsion usually accompanies the varus.
-
Fibular shortening has not been proven effective in this condition.
-
-
Spinal fusion:
-
Indicated for severe kyphosis of >40° that fails to respond to bracing by the age of 8–10 years (3,4)
-
-
Laminectomy:
-
If indicated for spinal stenosis, it
should be extensive: Usually decompression of the entire lumbar spine
and sometimes of the lower thoracic spine. -
Kyphosis may need to be corrected at the same time if it is severe or if the patient is growing.
-
-
Limb lengthening:
-
May produce substantial gains in height
-
May improve lumbar lordosis and stenosis by stretching hamstrings
-
Usually, however, bilateral lengthening
of the femur, tibia, and humerus is necessary to achieve acceptable
proportions, a treatment program that lasts several years.
-
-
Foramen magnum decompression:
-
Should be done by an experienced neurosurgeon, after multidisciplinary consultation, if patient fails to improve.
-
Prognosis
-
Good, except for spinal stenosis
-
Visceral involvement is absent.
-
The rare, homozygous form usually results in death in a few weeks to months.
-
Heterozygous individuals have a normal life span.
-
Intelligence is normal.
-
Patients usually are independent in daily life.
Complications
-
Spinal stenosis
-
Nerve root compression
-
Knee pain
Patient Monitoring
-
Given the high propensity to orthopaedic problems, patients should be seen routinely.
-
Periodic examinations of extremity strength and bladder control are warranted.
References
1. Sponseller
PD, Ain MC. The skeletal dysplasias. In: Morrissy RT, Weinstein SL,
eds. Lovell and Winter’s Pediatric Orthopaedics, 6th ed. Philadelphia:
Lippincott Williams & Wilkins, 2006:205–250.
PD, Ain MC. The skeletal dysplasias. In: Morrissy RT, Weinstein SL,
eds. Lovell and Winter’s Pediatric Orthopaedics, 6th ed. Philadelphia:
Lippincott Williams & Wilkins, 2006:205–250.
2. Nicoletti B, Kopits SE, Ascani E, et al. Human Achondroplasia. A Multidisciplinary Approach. New York: Plenum Press, 1988.
3. Ain MC, Shirley ED. Spinal fusion for kyphosis in achondroplasia. J Pediatr Orthop 2004;24:541–545.
4. Ain MC, Shirley ED, Pirouzmanesh A, et al. Postlaminectomy kyphosis in the skeletally immature achondroplast. Spine 2006;31: 197–201.
ICD9-CM
-
259.4 Dwarfism
-
724.00 (general) Spinal stenosis
-
756.4 Achondroplasia
Patient Teaching
-
Genetic counseling
-
Weight control, which is often a problem and is helped by exercise
-
Early detection of spinal stenosis
-
Vocational counseling, to avoid physical labor occupations
-
Usually no restriction on activity unless spinal stenosis occurs
-
Mention Dwarf Amateur Athletic Association, a competitive forum
Activity
-
Counsel patient to:
-
Remain physically active on a regular basis
-
Avoid excessive weight gain
-
Avoid hyperextension stress
-
Prevention
Patients should be told about the signs and symptoms of
spinal stenosis so that it can be detected at the earliest possible
point.
spinal stenosis so that it can be detected at the earliest possible
point.
FAQ
Q: How should a patient with achondroplasia be followed?
A:
Especially in childhood, a geneticist usually has the most knowledge
about the entire spectrum of the condition. He or she should see the
patient at least yearly and can consult other specialists as needed.
Especially in childhood, a geneticist usually has the most knowledge
about the entire spectrum of the condition. He or she should see the
patient at least yearly and can consult other specialists as needed.
Q: What are the signs and symptoms of spinal stenosis in achondroplasia?
A:
Spinal stenosis is heralded by thigh and leg pain that is worse with
walking and not localized just to the knee. Physical stamina may become
challenged. The need to stoop forward and rest holding the thighs is a
characteristic move.
Spinal stenosis is heralded by thigh and leg pain that is worse with
walking and not localized just to the knee. Physical stamina may become
challenged. The need to stoop forward and rest holding the thighs is a
characteristic move.

