Chondroblastoma
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Chondroblastoma
Chondroblastoma
Constantine A. Demetracopoulos BS
Frank J. Frassica MD
Description
-
A benign tumor of cartilaginous origin with a predilection for the epiphysis in skeletally immature patients
-
Generally found in the epiphyses of long bones.
-
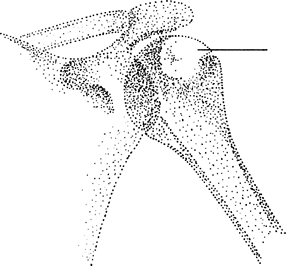
The humerus is most commonly affected, followed by the tibia and femur (1) (Fig. 1-1).
-
-
Synonyms: Codman tumor; Epiphyseal chondromatous giant cell tumor
Epidemiology
A slight male predominance (2:1) is noted (2).
Incidence
-
This tumor is rare.
-
In the largest series, chondroblastoma accounted for 1% of all skeletal neoplasms (3).
Risk Factors
None known
Genetics
No known genetic component exists.
Etiology
-
The pathogenesis is unknown.
-
Most authors agree that the neoplastic cells arise from “cartilage-forming matrix cells” or chondroblasts.
-
The tumor may be related to chondromyxoid fibroma.
Associated Conditions
Aneurysmal bone cyst
 |
|
Fig. 1. Chondroblastoma is a lucent lesion in the immature epiphysis, most often the proximal humerus.
|
Signs and Symptoms
-
Patients usually complain of mild to moderate chronic pain, often months to years in duration.
-
Stiffness and effusion of the adjacent joint also are common.
-
Local swelling is uncommon.
Physical Exam
-
The adjacent joint may have an effusion and decreased ROM.
-
A soft-tissue mass is uncommon.
-
Joint tenderness is unusual.
Tests
Lab
-
Tests are not helpful.
-
All blood tests are within normal limits, including the ESR.
Imaging
-
Radiography:
-
The radiographic appearance is that of a lytic lesion in the epiphysis with a thin sclerotic rim.
-
The sclerotic rim indicates the benign nature of the lesion.
-
It may expand or deform the bone.
-
Occasionally, punctate calcifications may be seen.
-
-
The patient’s history and plain radiographs usually are sufficient for making the diagnosis.
-
-
MRI:
-
May be used if history and radiography are not definitive
-
The boundary of the lesion on MRI scans should be distinct.
-
Pathological Findings
-
The diagnosis requires the presence of chondroblasts on microscopic section.
-
Chondroblasts are small, round or polygonal cells with round or oval nuclei.
-
Cells are described as looking “plump” or like fried eggs.
-
A lattice of calcification extends between the cells (chicken wire) (1).
-
-
Interspersed giant cells are a common feature and may lead to confusion with giant cell tumor.
-
Areas of aneurysmal bone cyst degeneration also may be present.
Differential Diagnosis
-
Enchondroma
-
Giant cell tumor
-
Osteomyelitis
-
Fibrous dysplasia
General Measures
-
Surgical excision is recommended to prevent progressive growth of the lesion with destruction of the epiphysis.
-
Bone grafting is needed.
-
Surgery is sometimes technically demanding because of the need to preserve or reconstruct the nearby joint surface.
Activity
No restrictions on activity are necessary because pathologic fracture is not a problem.
P.71
Special Therapy
Physical Therapy
Therapy may be used to regain ROM and strength after surgery.
Surgery
-
Because the tumor is considered benign, local measures suffice.
-
Surgery generally involves curettage and bone grafting.
Prognosis
-
The recurrence rate with chondroblastoma alone is 20% at 3 years (3).
-
If the tumor has an aneurysmal component, the risk of recurrence is higher (3).
Complications
-
Recurrence
-
Joint stiffness
Patient Monitoring
-
Follow-up care is necessary because recurrence is common.
-
Radiographs should be repeated every 6–12 months after excision for ~2 years.
References
1. McCarthy
EF, Frassica FJ. Primary bone tumors. In: Pathology of Bone and Joint
Disorders: With Clinical and Radiographic Correlation. Philadelphia: WB
Saunders Co, 1998:195–275.
EF, Frassica FJ. Primary bone tumors. In: Pathology of Bone and Joint
Disorders: With Clinical and Radiographic Correlation. Philadelphia: WB
Saunders Co, 1998:195–275.
2. Spjut
HJ, Dorfman HD, Fechner RE, et al. Tumors of cartilaginous origin. In:
Tumors of Bone and Cartilage. Washington, DC: Armed Forces Institute of
Pathology, 1971:33–116.
HJ, Dorfman HD, Fechner RE, et al. Tumors of cartilaginous origin. In:
Tumors of Bone and Cartilage. Washington, DC: Armed Forces Institute of
Pathology, 1971:33–116.
3. Huvos
AG. Chondroblastoma and clear-cell chondrosarcoma. In: Bone Tumors:
Diagnosis, Treatment, and Prognosis, 2nd ed. Philadelphia: WB Saunders
Co., 1991:295–318.
AG. Chondroblastoma and clear-cell chondrosarcoma. In: Bone Tumors:
Diagnosis, Treatment, and Prognosis, 2nd ed. Philadelphia: WB Saunders
Co., 1991:295–318.
Additional Reading
Masui F, Ushigome S, Kamitani K, et al. Chondroblastoma: a study of 11 cases. Eur J Surg Oncol 2002;28:869–874.
Ramappa AJ, Lee FY, Tang P, et al. Chondroblastoma of bone. J Bone Joint Surg 2000;82A:1140–1145.
Suneja
R, Grimer RJ, Belthur M, et al. Chondroblastoma of bone: long-term
results and functional outcome after intralesional curettage. J Bone Joint Surg 2005;87B:974–978.
R, Grimer RJ, Belthur M, et al. Chondroblastoma of bone: long-term
results and functional outcome after intralesional curettage. J Bone Joint Surg 2005;87B:974–978.
Codes
ICD9-CM
213.4 Chondroblastoma
Patient Teaching
-
Patients should be counseled that the lesion is benign and rarely metastasizes (<2%).
-
However, if the tumor is not removed,
local morbidity may occur because of progressive enlargement of the
involved epiphysis and destruction of the joint.
FAQ
Q: Is chemotherapy or radiation therapy needed for chondroblastoma?
A: Chondroblastoma is a benign bone tumor so there is no need for chemotherapy or radiation therapy.
Q: Is there any risk of getting a viral disease or hepatitis after curettage and bone grafting for a chondroblastoma?
A:
In general, no risk exists. The graft materials are very safe in that
all the cells and nonbone proteins are removed. The exception is
fresh-frozen grafts, which have the same risk of viral transmission as
a blood transfusion (~1 in 500,000).
In general, no risk exists. The graft materials are very safe in that
all the cells and nonbone proteins are removed. The exception is
fresh-frozen grafts, which have the same risk of viral transmission as
a blood transfusion (~1 in 500,000).
