Ultrasound Guided Interscalene Block
Supine, with head turned to contralateral side, as far as is
comfortable for the patient. The ipsilateral arm should be adducted at
the shoulder.
The nerve plexus is sandwiched between the scalene muscles. The carotid
artery and internal jugular vein lie deep to the sternocleidomastoid
muscle and medial to the brachial plexus at this level. In some
patients, the vagus nerve may be seen between the carotid and jugular
vein and the phrenic nerve may be seen lateral to the carotid artery
and jugular vein as it courses over the anterior scalene muscle.
The skin should be prepped in sterile fashion, and the transducer
sterilized or covered with a sterile probe cover. Sterile sonographic
gel is placed on the skin over the block site. The transducer is then
placed on the skin at approximately the C6 level, and moved slowly
cephalad or caudad to obtain an optimal image. The plexus can usually
be found 1.5 to 2.5 cm lateral to the border of the internal jugular
vein. Ideally, two or three nerve roots or trunks can be imaged in
vertical alignment (Fig. 33-1).
 |
|
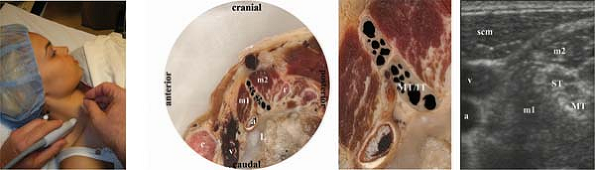
Figure 33-1.
a, carotid artery; c, clavicle; IT, inferior trunk; L, lung; m1, anterior scalene muscle; m2, middle scalene muscle; MT, middle trunk; scm, sternocleidomastoid muscle; ST, superior trunk; v, internal jugular vein. |
and predictable at the supraclavicular fossa, some practitioners begin
with the transducer at this site, in a sagittal oblique position. This
allows imaging of the trunks of the plexus cephalad and posterior to
the subclavian artery (see Figure 34-1 in Chapter 34
on ultrasound guided supraclavicular block). From the supraclavicular
fossa, the trunks can be traced cephalad to the interscalene region.
be inserted at the posterior or anterior margin of the transducer. The
needle should be kept in view along its length by keeping it parallel
to, and aligned with, the long axis of the transducer (in-plane
technique). This allows constant assessment of the tip of the needle.
(or trunk) that has been selected as the target. The nerve stimulator
may be turned on at this time to confirm the target, at a current of
0.4 to 1.0 mA. As soon as confirmation is obtained with motor or
sensory stimulation, the stimulator can be switched off (alternately,
it can be left on until injection begins, to confirm that the twitch
disappears at this time). Local anesthetic solution is then injected
under direct visualization, 1 to 3 mL at a time. The syringe should
frequently be aspirated for blood. As injection proceeds, patient
discomfort or paresthesia should be assessed, and the solution should
be evident as it distends tissues at the tip of the needle on the
ultrasound screen. Circumferential spread of the solution around the
trunk should be noted. If not, the needle tip may be slowly moved to a
position which allows this spread. Whenever the needle is moved, the
assessment for paresthesias and aspiration for blood should again be
carried out. Each root or trunk should be anesthetized unless the
injection appears to be confined to a fascial space around all of the
nerves.
-
Occasionally during interscalene block
with ultrasound guidance, “posterior” shoulder twitches will be
elicited on stimulation of the presumed target nerve. This is most
likely due to stimulation of the suprascapular nerve, which branches
quite proximally from the plexus to innervate the supraspinatus and
infraspinatus muscles. The needle should be moved to a different target
nerve to ensure complete brachial plexus block. -
All interscalene blocks can produce
hoarseness or Horner’s sign, and all produce ipsilateral diaphragmatic
paralysis. Appropriate patient selection is paramount, and patients
should be warned of this side effect. -
Because of the high level of this block
in the brachial plexus, and the injection of local anesthetic solution
at the superior trunk or C5/C6 nerve roots, incomplete block of the
inferior trunk or roots C8 and T1 may occur unless these structures are
individually
P.279
identified
and anesthetized. When roots C8 and T1 or the inferior trunk are only
partially anesthetized, there will be some sparing in the innervation
of the median, radial, and ulnar nerves of the hand.
