BURN CONTRACTURES
vehicle accidents as the leading cause of accidental death in the
United States (10). Despite aggressive
techniques of acute burn wound management, crippling hand deformities
occur. In a severe burn, the hand, which accounts for 5% of the total
body surface area, is often neglected as attention is focused on
helping the burn victim to survive. By the time it has been ascertained
that the patient will survive, fixed contractures that are functionally
disabling and aesthetically displeasing often have developed, and
surgical reconstruction may be indicated (1,12,22,24).
satisfactorily without tissue replacement. Deep second-degree (i.e.,
partial-skin-thickness), third-degree (i.e., full-skin-thickness), and
fourth-degree (i.e., tendon, bone, nerve, or joint) burns that are not
debrided and covered with skin grafts or flaps heal by granulation
tissue, producing scar and contractures. Early wound closure and
splinting are essential to prevent contractures during the acute burn
period and to minimize the necessity for secondary reconstruction.
Beasley observed that the triad of edema, inflammation, and especially
immobility is responsible for the deformities produced by thermal
injuries (7). He further pointed out that the
severity of the deformities is directly proportional to the amount of
time a wound remains open.
several factors require consideration. First, the surgeon must assess
the functional needs of the patient. There is no reason to launch a
series of reconstructive procedures if a patient has fully adjusted to
his condition and is able to carry out the activities of daily living
as easily as before the burn (17). Having
decided to proceed with reconstruction, remember that other priority
areas, particularly the head and neck, may require surgical correction;
if a large area of body surface has been burned, unscarred skin may be
at a premium. Therefore, the surgeon must plan for the appropriate
allocation of skin. Preoperative radiographs are mandatory before any
procedure involving the mobilization of joints.
with a soft-tissue release, because the articular surfaces may be
incongruous on account of sepsis, dislocation, or heterotopic
ossification. Although both extremities may be burned and require
reconstruction, it may be practical to reconstruct only one extremity
because of limited skin availability, leaving the other as an assistive
appendage. If the entire extremity including the axilla is burned,
reconstruction should proceed in a proximal to distal fashion; shoulder
and elbow mobility should be restored before hand procedures are
performed. Full hand motion is useless if elbow and axillary
contractures preclude positioning the hand in space (23).
Reconstructive procedures should preferably not be performed through
scar that is hypertrophic and red. Wait until the scar has matured, a
process that can be accelerated with the use of elastic pressure
garments.
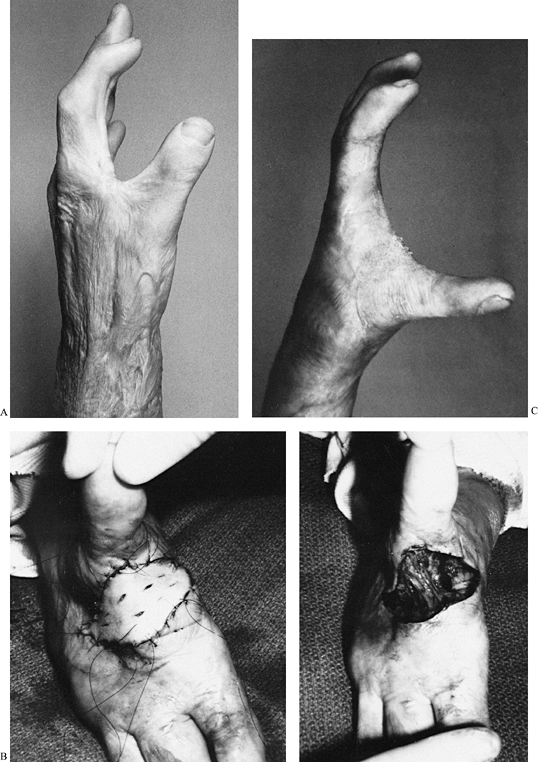
soft-tissue coverage before reconstruction of specific anatomic
locations can be accomplished (Fig. 64.1). Burn
contractures are corrected by scar incision, excision, or a combination
of both procedures. Afterward, a soft-tissue defect exists.
 |
|
Figure 64.1. Outline of the surgical treatment of burn contractures.
|
a local flap, or a combination of the two. After a burn release, local
flaps, such as Z-plasties, have limited application and should be
considered for coverage only if the flap consists of pliable, unburned
skin. Scarred skin usually does not tolerate the stress of being
rotated as a local flap, and a significant portion of the flap may
become necrotic. Local flaps, however, have the advantages of providing
a good color match and usually obviate the need for a skin graft.
contracture release or excision. Skin grafts adhere only to a
well-vascularized surface. A tendon denuded of paratenon, bone without
periosteum, and articular cartilage do not accept a skin graft; they
require flap coverage. If simultaneous or future bone, nerve, or tendon
reconstruction is being considered, a skin graft alone provides
insufficient coverage.
depend on the size and location of the defect and the availability of
unburned donor skin. A donor site should be inconspicuous and should
match the recipient defect as closely as possible. For example, a
defect on the palm would ideally be covered with adjacent, unscarred
palmar skin, but transfer is rarely possible because of the limited
availability of palmar skin. Unscarred skin is usually available from
the lateral, hair-free portion of the groin or from the buttocks, or
even from the instep of the foot. After selecting a donor site, the
physician must next choose between a split-thickness skin graft and a
full-thickness skin graft.
burned hand reconstruction. It is durable and is particularly suited
for contact areas, such as the palm and the mobile palmar surface of
the fingers. It contracts less than a split-thickness skin graft and is
less conspicuous. The donor site for a full-thickness skin graft is
closed primarily, so there is considerably less postoperative pain than
occurs after a split-thickness skin graft, in which the
reepithelializing donor site may be painful for several days after
graft harvesting.
split-thickness graft a more practical choice for coverage than a
full-thickness skin graft. If the area to be covered is large, a
split-thickness skin graft is indicated. The donor site for a
split-thickness skin graft does not require primary closure, and more
skin is available for grafting. The split-thickness skin graft can be
expanded by meshing, although meshed skin is aesthetically displeasing
and it tends to contract more than a nonmeshed graft. A split-thickness
graft is also indicated if the recipient bed has poor vascularity, as
occurs following radiation burns or with burns in which there is
residual skin ulceration and low-grade sepsis.
applicable. Fourth-degree burns, particularly if untreated during the
acute burn period, tend to leave the extremity in a contracted,
fibrotic condition (21). After the scar has been
excised, there is often exposed bone, tendon, or joint, and these
structures will not accept skin grafting of any kind. Furthermore, with
deep fourth-degree burns, it is often necessary to perform
reconstructive procedures involving the tendons (e.g., tenolysis or
tendon graft) or joints (e.g., capsulotomy); coverage with a skin graft
is not appropriate because the graft, even if it does take, adheres
tightly to the tendon or joint, limiting mobility. Always perform scar
release or scar excision before elevation of a flap. After excision of
the burn cicatrix, the recipient bed may be three to four times larger
than it was before. Knowing the dimensions of the recipient bed, the
surgeon can better design an appropriate-size flap.
involve injury to the skin alone, and a flap is usually not indicated.
If mobile structures are exposed, however, or if future reconstruction
is anticipated, do not hesitate to apply a flap.
of the hand, its functional restoration is a primary goal in
upper-extremity reconstruction after burns. For normal thumb function,
there must be adequate length, sensibility, mobility, stability, and
strength, and a satisfactory appearance. Most thermal injuries produce
skin contractures that limit thumb mobility and use. In severe burns,
loss of thumb length is usually secondary to a fourth-degree injury in
which the distal portion or more of the thumb becomes necrotic,
necessitating amputation. In children, longitudinal growth may be
restricted because of a dermal contracture or direct thermal injury to
the growth plates.
metacarpal is adducted toward the index finger metacarpal in a plane
perpendicular to the palm, is the most common contracture of the burned
thumb (26). In its mildest form, it is produced
by dorsal scarring over the thumb–index web, and the palmar skin is
usually not burned. Reconstruction of the thumb–index cleft can be
accomplished by several techniques.
-
Design it so that the palmar limb
generally follows the thenar crease, the middle limb parallels the
leading edge of the thumb–index cleft, and the dorsal limb parallels
the ulnar aspect of the thumb metacarpal. All limbs should be of equal
length. -
After incision, elevate the flaps, making
them as thick as possible, and preserve any blood vessels that
penetrate the base of the flap. -
Take care to avoid dividing the radial neurovascular bundle to the index finger that lies immediately beneath the palmar flap.
-
After the flaps have been raised, release the previously inflated tourniquet and secure meticulous hemostasis.
-
Rotate the flaps and sew them into
position. Be sure that the flaps are vascularized. A flap that is dark
and congested (e.g., in venous insufficiency) or one that is pale and
white (e.g., in arterial insufficiency) invariably becomes necrotic. If
not vascularized, return the flap to its original position and consider
an alternative form of coverage, such as skin grafting.
linear contractures and can be performed only when the skin being
rotated is relatively pliable and unburned. If the skin is scarred and
fibrotic, seek alternative techniques of coverage.
-
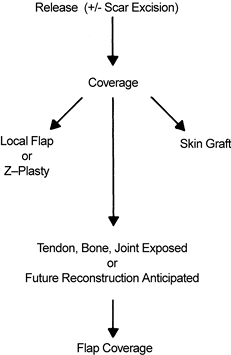
If contracture is severe, it is best to divide the contracture band sharply by incising perpendicular to it (Fig. 64.2).
Carry the incision down to the fascia overlying the first dorsal
interosseous muscle and to the leading edge of the adductor pollicis
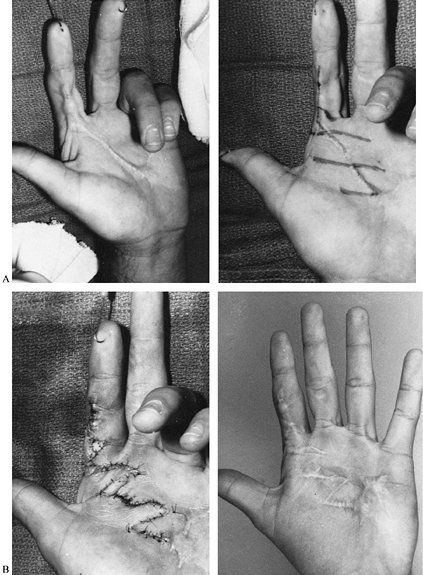
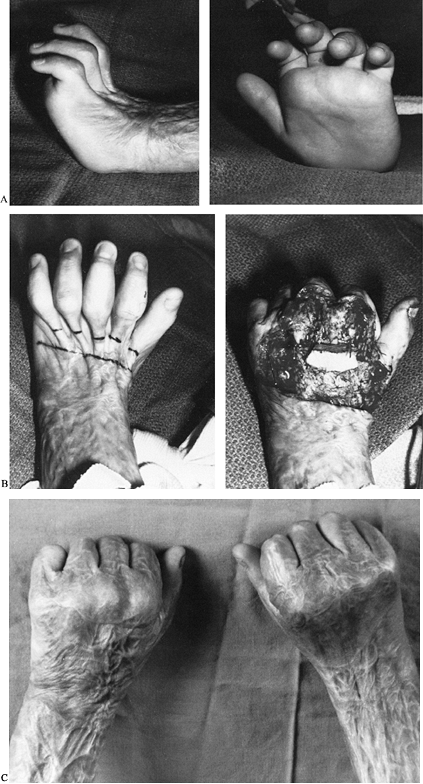
muscle.![]() Figure 64.2. A: Thumb adduction contracture of moderate severity. B: A transverse release down to the adductor pollicis and first dorsal interosseous muscles (left), followed by application of a full-thickness skin graft (right). C:
Figure 64.2. A: Thumb adduction contracture of moderate severity. B: A transverse release down to the adductor pollicis and first dorsal interosseous muscles (left), followed by application of a full-thickness skin graft (right). C:
The final result 13 months after release. (From Stern PJ, Neale HE,
Carter W, and MacMillan BG. Classification and Management of Burned
Thumb Contractures in Children. Burns 1985;11:168, with permission.) -
Cover the resultant defect, which is elliptical, with a skin graft.
-
If the patient has sustained a deep burn,
a severe adduction contracture may result. This type of contracture
involves more than skin and necessitates release of deep structures. -
Release the dermal contracture and the fascia overlying the first dorsal interosseous and adductor as outlined earlier.
-
If the thumb remains tightly adducted,
consider releasing the insertion of the adductor pollicis muscle from
the base of the proximal phalanx of the thumb. The adductor muscle in a
severe burn is often fibrotic but rarely nonfunctional; therefore, it
is advisable to reinsert the muscle more proximally on the neck or
shaft of the thumb metacarpal through a pull-out wire or suture anchor. -
Rarely, even after the skin and adductor
muscle have been released, an adduction contraction may persist. In
these instances, carry the incision down over the trapeziometacarpal
joint and release the joint capsule. -
If the contracture still persists, excision of the trapezium is indicated.
-
It is usually necessary to pass a
temporary Kirschner pin from the thumb metacarpal into the carpus to
hold the thumb in its newly released position. -
After such an extensive release, coverage
with a skin graft is usually inadequate. Plan on using a distant flap,
such as one from the hair-free inner aspect of the contralateral
forearm, to resurface and maintain breadth of the thumb–index cleft. -
After release of any adduction
contracture, postoperative splinting is mandatory. Although there are
several causes of a persistent contracture—including inadequate
surgical release, loss of skin graft, or the inappropriate use of
burned skin or flap coverage—one of the most common causes is failure
to splint the thumb metacarpal midway between palmar and radial
abduction. A splint can be fabricated from thermoplastic material and
lined with silicone to maintain satisfactory breadth between the thumb
and index finger. Have the patient wear the splint until the wound has
matured, usually 3 to 9 months. It is often helpful to alternate
splinting with use of an elastic compressive glove, which also
accelerates the scar maturity.
(i.e., when scarring over the palmar aspect of the thumb produces
flexion of the interphalangeal or metacarpophalangeal joint) (26).
As in adduction contractures, all of these contractures require
surgical incision with or without a scar excision, followed by
appropriate soft-tissue coverage and splinting.
flexion or hyperextension contractures of the interphalangeal or
metacarpophalangeal joint of the thumb often coexist, producing
articular incongruity and joint subluxation or dislocation. In such
cases, particularly if there is satisfactory mobility of two of the
three thumb joints, an arthrodesis of the dislocated joint in a
functional position is indicated.
Restoration of length can be accomplished by a number of surgical
techniques. These include toe-to-hand transfer and osteoplastic
reconstruction, consisting of a tube pedicle flap placed around a bone
graft, followed by neurovascular island transfer for restoration of
sensibility. Also possible are metacarpal osteotomy and progressive
distraction and pollicization with movement of an adjacent digit,
usually the index finger, on its neurovascular pedicle to the thumb
position. If only a small amount of thumb length has been lost, use
phalangization to increase thumb length. Release the thumb-web
contracture, and proximally transpose the adductor muscle to the thumb
metacarpal, making the thumb–index cleft deeper and giving the thumb
more apparent length (28).
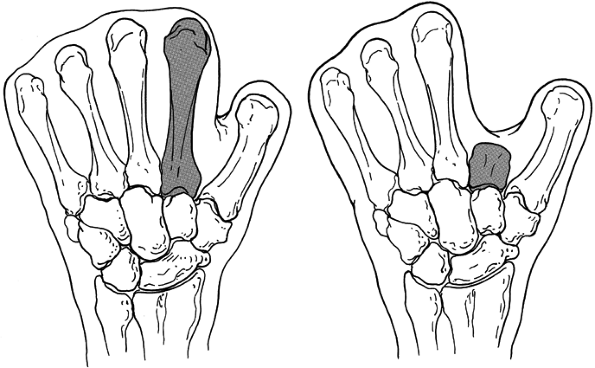
not feasible. The phalanges may have been amputated, and various
lengths of metacarpals may be encased in a cocoon of burned skin. If
thenar muscle contraction can be appreciated by manual palpation, a
“mitten hand” can be created by excising the index finger metacarpal
(leaving the base where the wrist flexor and extensor tendons attach).
Thereby a cleft is created between the thumb and ulnar digits so that
the patient can accomplish a pinch maneuver of a crude side-to-side
type (Fig. 64.3).
 |
|
Figure 64.3. A: “mitten hand” is created by excising the index metacarpal. A crude pinch maneuver is possible if the thenar motors are intact.
|
Pollicization is more likely to be successful if there is an intact
thumb trapeziometacarpal joint, functioning thenar musculature, and
relatively good sensibility of the digit to be pollicized.
excise scarred tissue in the thumb–index cleft and replace it with a
skin flap from the groin or abdomen, which can later be used to
resurface the cleft between the pollicized thumb and the remaining
ulnar digits. After flap tissue has been transferred, perform the
pollicization procedure. It is preferable to transfer the index ray,
particularly if it has been damaged and is already short (Fig. 64.4). If it is absent, any other digit can be transferred.
 |
|
Figure 64.4. A:
Preoperative photograph of a hand that is ideally suited for pollicization of the index finger. Neither the thumb nor the index remnant is functional. B: Index pollicization and application of the distal flap have resulted in creation of a useful thumb. |
thumb), design the incisions so that the pollicized digit can be
transposed and rotated to provide skin flaps for a cleft between the
thumb and the remainder of the hand. When pollicizing a burned index
finger, make the incisions along the border of areas that have
previously been scarred, exposing the index metacarpal shaft and the
tip of the thumb.
-
Reflect the interosseous muscles from the
index metacarpal shaft. They are often fibrotic and are not useful for
future motor function, as in conventional pollicizations. -
Ligate the proper digital artery to the
radial side of the middle finger, and split the common digital nerve to
the index and middle finger proximally as far as possible. -
Osteotomize the index finger metacarpal
through its base, and remove a segment of metacarpal shaft, being
careful to preserve the index metacarpophalangeal joint. -
Rotate the index finger so that it can be
put on top of the thumb remnant with the pulp of the pollicized digit
directly facing the ulnar digits. Turn the pollicized digit so that it
is 120° to 140° from the plane of the palm. It is easiest to stabilize
the skeletal structure of the pollicized digit with one or two
longitudinal Kirschner pins. -
Deflate the tourniquet to ensure that the
pollicized digit is viable and that its vascular pedicle has not been
stretched or twisted. -
Close the wound, being careful to line the thumb–index cleft with soft, pliable skin.
-
Maintain skeletal pin fixation for 6–8 weeks, and maintain splinting of the thumb in wide palmar abduction for 6–9 months.
inadequate bony fixation, or contracture of the thumb cleft cause the
most common complications of pollicization. These can usually be
prevented by careful preoperative planning and attention to
intraoperative technique.
advantage of being a one-stage procedure that does not require
microvascular techniques. It converts two relatively useless digits
into a single, functional, opposable thumb, making activities requiring
opposition and prehension possible.
flexion or extension contractures. If surgical intervention is
necessary, take preoperative radiographs of the proximal
interphalangeal joint to confirm that a cartilaginous space is present
and that the joint is not subluxed or dislocated (8).
palmar skin of the proximal interphalangeal joint or from dorsal burns
in which the central tendon over the proximal interphalangeal joint is
disrupted, resulting in a “burn boutonnière” deformity. They may also
come from a dorsal burn over the metacarpophalangeal joint, producing a
metacarpophalangeal hyperextension deformity and a proximal
interphalangeal flexion deformity secondary to the tenodesis effect of
the tightened flexor tendons (27). To treat
these contractures successfully, determine the cause and then select an
appropriate technique for surgical correction.
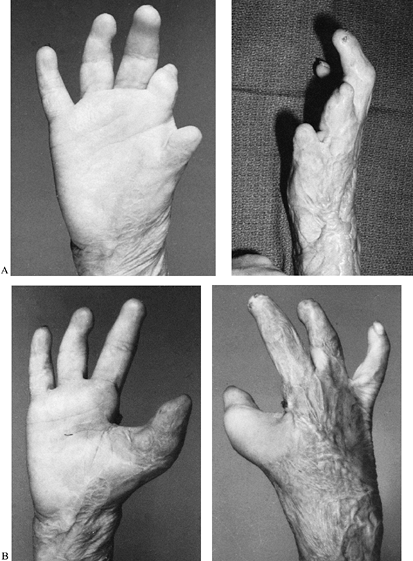
scar band across the interphalangeal or metacarpophalangeal joints,
with pliable skin on either side of the band, can be corrected by a
single Z-plasty or a series of Z-plasties (Fig. 64.5). If there is extensive scarring of the palmar skin, incision and possible excision of the scar band will be necessary (Fig. 64.6).
 |
|
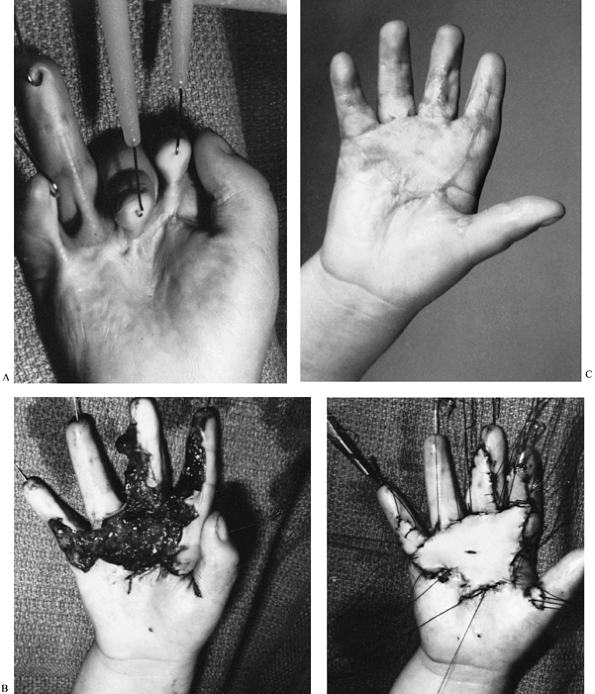
Figure 64.5. A: A linear contracture of the index finger (left) with pliable skin on each side of the scar band. A series of multiple Z-plasties is designed (right). B: The Z-plasties are rotated into position (left), and there is full digital extension after surgery.
|
 |
|
Figure 64.6. A: Moderately severe contracture of all digits as a result of a palmar contact burn. B: The burn scar was excised, the digits were pinned temporarily in extension, and a full-thickness autograft was applied. C: After surgery, nearly full digital extension is possible.
|
-
If a contracture of only the proximal
interphalangeal joint exists, incise the scar transversely across the
anterior aspect of the joint, extending the incision from the radial to
the ulnar midaxial line (4). It is usually
unnecessary to excise the contracture band completely. Carry the
incision down to the flexor tendon sheath, taking
P.1770
care not to sever the digital nerves. They are always deep to the burn scar and are usually covered by a thin layer of fat. -
If a proximal interphalangeal flexion
contracture persists after dermal release, decide whether to perform a
proximal interphalangeal capsular release. If so, the flexor tendons
will be exposed, and flap coverage, using an adjacent cross-finger flap
or a distant flap, will be necessary to prevent tendon desiccation (15). -
If the flap procedure is not feasible, do not perform a capsular release. Accomplish coverage with a skin graft.
-
Regardless of the coverage technique,
deflate the tourniquet and secure meticulous hemostasis. Assess the
newly extended finger for vascular integrity, because arterial inflow
may be compromised by the sudden digital extension. If the digit is
pale, flex it until circulation has been restored. -
Temporary proximal interphalangeal joint immobilization with an oblique transarticular Kirschner pin is often helpful.
-
Cover the defect with a full-thickness skin graft that is stented with a tie over a bolus dressing.
-
After the graft has taken, extension
splinting at night with a silicone-lined, static splint is recommended
until the graft matures.
central tendon over the dorsum of the proximal interphalangeal joint
are difficult to reconstruct, because the skin over
the
dorsum of the joint is scarred, the central tendon has been destroyed,
and usually there is a fixed contracture of the palmar plate and
collateral ligaments. Consider restitution of proximal interphalangeal
extension only if the joint can be passively extended and radiographs
show joint congruity. If these requirements are met, excise the scarred
tendon over the proximal interphalangeal joint, and advance the more
proximal, unscarred, central tendon into the dorsal base of the middle
phalanx.
free graft is necessary. After the central slip has been reconstructed,
pin the proximal interphalangeal joint in extension for 3 weeks; then
initiate active flexion. The results of this surgery are unpredictable
and often unsatisfactory. If a fixed flexion contracture exists,
arthrodesis of the joint in a functional position can provide a more
reliable result.
extension contractures are difficult to treat successfully. They are
caused by skin fibrosis over the dorsum of the joint or by ischemic
contractures of the interosseous muscles. When the contracture is
secondary to a dorsal skin burn, a simple transverse release of
tightened skin and skin graft is adequate. Often, however, it is
necessary to perform a tenolysis of the extensor apparatus, divide the
dorsal capsule, and partially divide the dorsal, cordlike portion of
the collateral ligaments. At this point, the extensor tendon over the
dorsum of the proximal interphalangeal joint is usually exposed, and
coverage with a local flap must be performed.
tightness often can be successfully corrected. To make the diagnosis,
passively extend the metacarpophalangeal joint and then passively flex
the proximal interphalangeal joint; shortened, scarred, intrinsic
muscles resist passive flexion. Conversely, if the metacarpophalangeal
joint is passively flexed, the intrinsic muscles, whose axis of motion
is palmar to the metacarpophalangeal joint and dorsal to the proximal
interphalangeal joint, are relaxed, and passive proximal
interphalangeal flexion is unresisted. An intrinsic release can usually
be performed by excising the distal fibers of the lateral bands at the
level of the neck of the proximal phalanx.
interdigital clefts. During the acute burn period, it may be difficult
to gain access to this area, particularly if the metacarpophalangeal
joints are immobilized in the “safe” position of metacarpophalangeal
flexion. Syndactyly, usually of the dorsal skin, results. The degree of
syndactyly varies; in severe cases, it may extend beyond the proximal
interphalangeal joint.
Syndactyly of any degree restricts digital abduction and makes the
grasping of large, cylindrical objects difficult. The syndactylized
digits are often subjected to a sudden abduction force that can lead to
traumatic breakdown of the scar contracture, bleeding, and additional
fibrosis. Some patients complain that they are unable to wear gloves,
and others have problems with hygiene because particles of dirt collect
in a pocket formed by dorsally syndactylized skin and the normal distal
edge of the palmar skin.
-
Use skin grafts.
-
Use flaps to line the depth of the web space.
-
Make certain release is adequate with slight overcorrection.
-
Avoid straight-line incisions in the depth of the palmar aspect of the commissure.
-
Initiate proper stent fixation of skin grafts and postoperative immobilization of the extremity.
syndactyly on the severity of the syndactyly and the condition of the
adjacent skin (3,16,19).
Mild or moderate syndactyly can be treated by a Z-plasty or a local
rotation flap. The lateral palmar rotation flap is particularly
appealing, because it allows the surgeon to create a new interdigital
cleft with supple, local, full-thickness skin that is unlikely to
recontract (Fig. 64.7). Close the donor defect for rotation flaps, primarily if it is small, or cover it with a skin graft.
 |
|
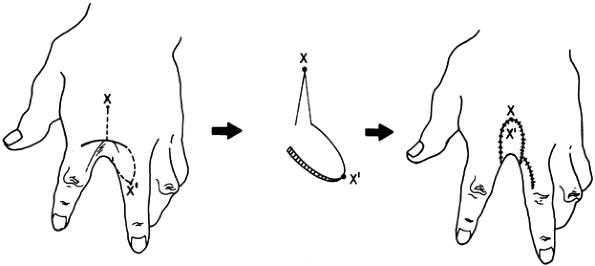
Figure 64.7. A dorsal web syndactyly exists between the index and middle fingers. A lateral volar flap (apex X′) is designed to rotate 180° so that points X and X′pr
can be opposed. In this example, the donor defect was closed primarily; however, if tension exists, a skin graft should be applied. |
The incisions on the palmar and dorsal sides should extend to the
bifurcation of the common digital artery. After the release has been
accomplished, cover it with a thick split– or full-thickness autograft.
Because the graft is placed on a concave surface, make sure that there
is
good
contact between the graft and its recipient bed. Stent the graft into
place. When you are certain the graft has taken, use night extension
splinting with the digits abducted for 6–9 months.
 |
|
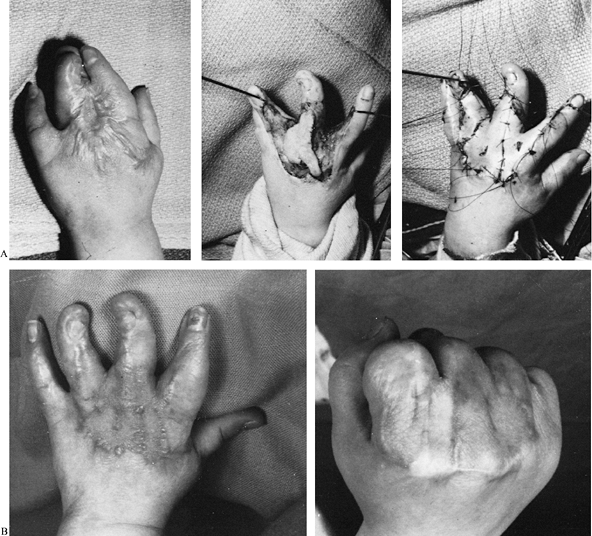
Figure 64.8. A: Severe dorsal burn syndactyly (left). Scar excision (center) is followed by application of a full-thickness graft (right). B: Postoperative extension (left) and flexion (right) views.
|
metacarpophalangeal joints occur simultaneously. These contractures
usually are the result of flame burns in which the victim tightly
clenches her fist or protects her face from thermal injury.
Metacarpophalangeal extension contractures arise from scarred skin over
the dorsum of these joints or from immobilization of the
metacarpophalangeal joints in extension during the acute burn period,
allowing the collateral ligaments and soft tissues around the
metacarpophalangeal joints to contract (13).
In mild metacarpophalangeal contractures, if the wrist is dorsiflexed
(i.e., the skin over the dorsum of the hand is relaxed), full, active,
metacarpophalangeal flexion can be accomplished. If the wrist is
passively flexed, however, metacarpophalangeal flexion is limited by
tight skin over the dorsum of the wrist and hand. A dorsal transverse
incision of the contracted skin at the level of the metacarpal necks is
often sufficient to release the contracture. If the scar tissue of the
dorsum of the metacarpophalangeal joints is thick or has been
previously grafted with meshed autograft, giving the skin a corrugated
appearance, it may be preferable to excise, rather than incise, the
burn scar. In such instances, carry the excision down to the
subcutaneous fat, taking care to
preserve the dorsal veins that are nearly always deep to the burn scar.
are produced by linear bands of scar that mimic the extensor tendons.
In such cases, the surgeon may make the error of not performing a deep
enough release for fear of severing a tendon that is mistakenly thought
to be within the burn cicatrix. This is virtually never the case. The
extensor tendons lie deep to the scar in a bed of loose, areolar,
connective tissue. After the release has been accomplished by incision,
excision, or a combination of both, soft-tissue coverage can usually be
accomplished with a skin graft.
contracture, a more aggressive surgical release is necessary. The
position of the metacarpophalangeal joint is fixed, regardless of wrist
position, and the metacarpal heads are prominent in the palm.
Metacarpophalangeal hyperextension may be so severe that the dorsal
surface of the proximal phalanx may lie on top of the dorsal surface of
the metacarpal. In such cases, associated flexion contractures of the
proximal interphalangeal joints, caused by the flexor tenodesis effect,
occur, as does destruction of the central tendon overlying the proximal
interphalangeal joint. Grasping objects of any size is difficult or
impossible, and often only a crude pinch maneuver between the index
finger and the thumb is possible.
 |
|
Figure 64.9. A: A dorsal burn caused combined wrist and metacarpophalangeal fixed extension contractures. B: Dorsal view (left)
with outline of the proposed excision. The linear bands over the metacarpophalangeal joints contain scar, not extensor tendons. After dermal release (right), metacarpophalangeal capsulotomies, and temporary pinning in flexion, a large dorsal area requires skin grafting. C: The functional result (both hands), demonstrating excellent metacarpophalangeal flexion. |
-
Release the metacarpophalangeal capsular
contractures by splitting the extensor tendon longitudinally over the
joint in its midportion and incising the dorsal capsule transversely. -
Release the collateral ligaments by
sharply dividing the origin of the ligament from the metacarpal head,
preserving the most inferior and proximal fibers to prevent lateral
joint instability. -
After the collateral ligaments and dorsal
capsule have been released, position the metacarpophalangeal joint in
70° of flexion by passing a pin from the metacarpal head into the
proximal phalanx. -
Sometimes after metacarpophalangeal
capsulotomies, the metacarpophalangeal joints and extensor tendons are
exposed, and they must be covered with a distant flap. Plan ahead for
such an eventuality to make sure that flap tissue is available. -
Initiate postoperative range-of-motion
exercises after the skin graft has taken. Begin a program of active and
passive metacarpophalangeal flexion exercises and night splinting with
the metacarpophalangeal joints in flexion to prevent recontracture.
surgical correction is often necessary because limited elbow mobility
directly affects the efficiency of hand, wrist, and
shoulder function (25).
These contractures are often subjected to the stress of sudden elbow
extension, resulting in recurrent tearing of antecubital burn scars,
pain, and additional fibrosis. Occasionally, burn scarring forms deep
pockets that collect debris and cause hygiene problems.
usually can be corrected by complete division of the dermal scar in the
antecubital fossa. The amount of scar varies from a longitudinal band
(correctable by Z-plasty, local flap, or skin graft) to diffuse
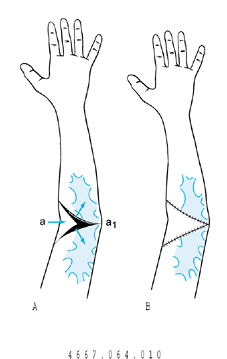
scarring (Fig. 64.10 and Fig. 64.11).
Regardless of technique, take care to extend the release to
subcutaneous tissue and avoid injuring anterior neurovascular
structures. For severe contractures, consider division of deeper
structures, which may include lengthening the biceps tendon, dividing
the brachialis fascia, and anterior elbow capsulotomy. When such
structures are divided, plan for flap coverage.
 |
|
Figure 64.10. Y–V flap. A: Scaring of the ulnar aspect of the antecubital fossa treated with a Y–V advancement flap (a is advanced to a1). B: Flap sewn into position. (From Kurtzman LC, Stern PJ. Upper Extremity Burn Contractures. Hand Clin 1990;6:261, with permission.)
|
 |
|
Figure 64.11. Full-thickness skin graft. A: Dotted line indicates incision for release of eschar, and the incision must extend to normal skin on the radial and ulnar sides. B: Diamond-shaped defect after release. C: Full-thickness skin graft applied for coverage. (From Kurtzman LC, Stern PJ. Upper Extremity Burn Contractures. Hand Clin 1990;6:261, with permission.)
|
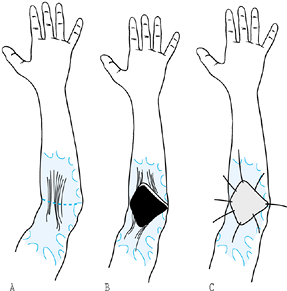
in the burn patient is heterotopic ossification bridging the elbow
joint (Fig. 64.12) (14).
The ossification forms in the acute burn period, is usually associated
with a concomitant deep burn to the elbow, and is found in
approximately 2% of patients with elbow burns. The first clinical signs
of heterotopic ossification appear 4–6 weeks after the burn injury and
are usually heralded by complaints of increasing elbow pain and a
rather rapid decrease in range of motion. Initial radiographs may be
unremarkable except for soft-tissue swelling, but follow-up radiographs
(within 3 months) show ossification bridging the elbow joint. If
heterotopic bone forms bilaterally, functional impairment is severe,
and the patient will have difficulty performing even simple activities
of daily living.
 |
|
Figure 64.12. A:
Radiographs demonstrate heterotopic ossification bridging the posteromedial surface of the elbow. The patient’s elbow was rigidly fixed in extension. B: An operative photograph shows that the ulnar nerve (marked by loops) proximal and distal to the elbow joint is encased by heterotopic ossification. It was unroofed and transposed anteriorly. C: After heterotopic bone excision, elbow flexion and extension were restored. |
appropriately. If the bone is excised when it is immature, it may
reform, making a second surgical excision even more difficult. Usually,
it takes 8–16 months for the bone to mature. Diagnostic studies used to
assess bone maturity such as serial technetium phosphate bone scans and
measurement of serum alkaline phosphatase levels may be misleading.
Despite the potential for bone reformation, we prefer early excision
(8–12 months), particularly if there is ulnar nerve compromise.
Test motor and sensory function of the ulnar nerve before surgery. If
function is impaired, an electromyogram and nerve conduction studies
are recommended. Ulnar nerve function can be anticipated to improve
following decompression (11).
-
Perform surgical excision of the bone through a long, posteromedial elbow incision.
-
Identify the ulnar nerve, proximal and
distal to the new bone. If bone encases the nerve, it is helpful to
unroof and transpose it anteriorly. -
After the nerve has been mobilized, it is
usually necessary to perform an elbow arthrotomy, because there are
often intraarticular adhesions that must be lysed. -
Detach and reinsert the medial collateral
ligament complex. After the skin has been closed, record the range of
motion, and splint the elbow for 3–5 days in 90° of flexion. Then begin
active and assisted passive range-of-motion exercises.
about the elbow have shown significant improvement in range of motion
in most cases (11). The worst results usually occur when there is complete ankylosis preoperatively.
mineralization and bone resorption, have been shown to be of some
benefit in the prevention of heterotopic bone formation in patients
undergoing total hip arthroplasty. There is, however, no evidence that
these compounds are effective in preventing bone from reforming after
excision in the burn victim. Other ancillary treatment modalities
include low-dose irradiation or oral indomethacin.
If surgical procedures are planned for more distal portions of the
extremity, correct the axillary contracture first to facilitate access
to these areas.
commonly, a band extends anteriorly from the chest to the upper arm,
parallel to the inferior edge of the pectoralis major muscle. There may
also be a posterior band from the chest to the brachium that follows
the inferior and lateral edge of the latissimus dorsi. Often, the deep
axillary skin in the apex of the axilla is unburned; in severe burns,
however, the axillary fossa may be obliterated completely.
same principles discussed earlier in this chapter. In most cases, the
treatment of choice is incision (often combined with excision) of the
scar. Carry the dissection down to the axillary fat. It is often
helpful to divide the fascia over the latissimus dorsi or pectoralis
major muscles. After the release, obtain coverage with a thick
split-thickness skin graft.
managed by release and skin grafting, this technique has the
disadvantage of prolonged postoperative splinting, occasional graft
loss, and linear contracture along the graft edges. To avoid these
problems, thin regional fasciocutaneous flaps have been successfully
used (2).
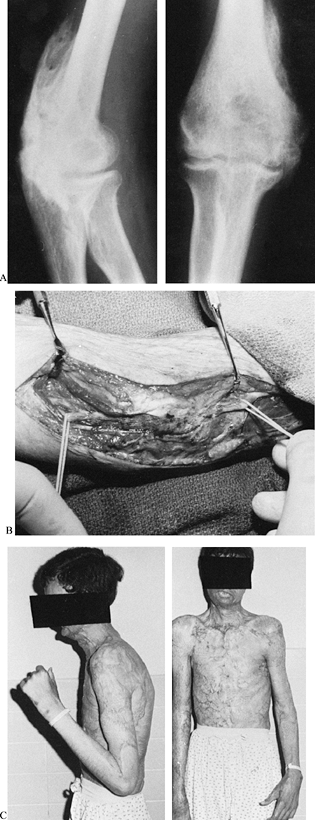
encountered in the thermally injured upper extremity can be solved with
the previously described skin grafting techniques. Complex wounds,
however, that have exposed joints, bone, or tendons resulting from
thermal injury or extensive scar release require flap coverage. Before
microsurgical free-tissue transfer, these wounds were covered with
distant pedicled flaps. The groin flap was commonly used for complex
hand wounds (Fig. 64.13).
 |
|
Figure 64.13. A: Deep contact burn with exposed tendons. B: Free microvascular lateral arm flap elevated from injured extremity for transfer to hand. C: Late follow-up showing excellent resurfacing.
|
limitations. Immobility and dependent positioning of the involved
extremity required for use of a groin flap are liabilities in the
rehabilitation of the acutely burned patient. In addition, in large
burns, availability of pedicled skin flaps may be severely limited.
Early wound coverage using free-tissue transfer techniques is a
single-stage procedure that allows for earlier rehabilitation and
salvage of the extremity (5). Free muscle flaps
are more likely to be available even after extensive burns. They are
particularly useful in reconstructive cases after patients have
finished the acute phase of their burn care.
valuable tool when growth plates, joints, tendons, and bone become
exposed, as usually occurs in deep contact burns and high-voltage
electrical injuries. Deep contact burns usually are the result of
contacting mufflers, printing presses, or roller presses (Fig. 64.13).
When such a burn occurs on the dorsum of the hand, the entire extensor
mechanism is at risk. Early debridement and coverage with a free flap
will prevent loss of the extensor mechanism. The flaps chosen for this
problem depend on the size of the wound and the availability of donor
sites. The lateral arm flap and temporalis fascia flap are useful
choices in this situation.
extremity are devastating. They frequently result in massive skin and
muscle loss. The amputation rate for high-voltage injury approaches 50%
(32). Preservation of vital structures
remaining after radical debridement and limb salvage requires early
coverage with large free flaps (9). Usually,
latissimus dorsi or rectus abdominal muscle flaps are required to cover
the entire defect. In addition, free-muscle transfer may be used to
restore function in extremities severely damaged by high-voltage
electrical injuries. Most commonly, a free gracilis muscle transfer is
used to restore finger flexion.
(Fig. 64.14).
To correct this mitten hand deformity, multiple problems need to be
addressed: A basic thumb must be created, as well as a first web space.
Additionally, established contractures in the digits and wrist must be
released. Ideally, a toe transfer offers the best result in thumb
reconstruction. Both the great toe and the second toe are acceptable
choices in restoring prehensile ability in this deformity. We prefer
the second toe in reconstructing the mitten hand and reserve the great
toe for isolated thumb reconstruction.
 |
|
Figure 64.14. A: Mitten hand deformity after a burn. B: Second toe prepared for microvascular transfer to thumb. C: Five-year follow-up showing thumb extension. D: Thumb flexion allowing prehension.
|
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
JW, MacMillan BG, Martel L. Correction of Postburn Syndactyly: An
Analysis of Children with Introduction of the VM-plasty and
Postoperative Pressure Inserts. Plast Reconstr Surg 1982;70:345.
JW, MacMillan BG, Martel L, Krummel R. Surgical Correction of Postburn
Flexion Contractures of the Fingers in Children. Plast Reconstr Surg 1981;68:218.
S, Pitkanen J, Sundell B. Microvascular Free Flaps in Early
Reconstruction of Burns in the Hand and Forearm. Case Reports. Scand J Plast Reconstr Surg 1984;18:139.
S, Meek RN, Snelling CF, et al. Range of Motion and Complications after
Postburn Heterotopic Bone Excision about the Elbow. J Trauma 1996;41:825.
TJ, Stern PJ, True MS. Classification and Treatment of Postburn
Metacarpophalangeal Joint Extension Contractures in Children. J Hand Surg [Am] 1990;15:450.
JWJ, Donelan MB, Toth BA, Wall J. Thumb Reconstruction in the Burned
Hand by Advancement Pollicization of the Second Ray Remnant. J Hand Surg [Am] 1984;9:484.
PJ, Neale HW, Graham TJ, Warden GD. Classification and Treatment of
Postburn Proximal Interphalangeal Joint Flexion Contractures in
Children. J Hand Surg [Am] 1987;12:450.
J. Discussion of Correction of Postburn Syndactyly: An Analysis of
Children with Introduction of the V-M Plasty and Postoperative Pressure
Inserts. Plast Reconstr Surg 1982;70:353.