Pediatric Shoulder
-
These account for <5% of fractures in children.
-
Incidence ranges from 1.2 to 4.4 per 10,000 per year.
-
They are most common in adolescents owing to increased sports participation and are often metaphyseal, physeal, or both.
-
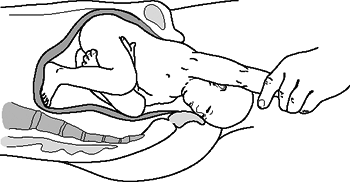
Neonates may sustain birth trauma to the proximal humeral physis, representing 1.9% to 6.7% of physeal injuries (Fig. 43.1).
-
Eighty percent of humeral growth occurs at the proximal physis, giving this region great remodeling potential.
-
There are three centers of ossification in the proximal humerus:
-
Humeral head: This ossifies at 6 months.
-
Greater tuberosity: This ossifies at 1 to 3 years.
-
Lesser tuberosity: This ossifies at 4 to 5 years.
-
The greater and lesser tuberosities coalesce at 6 to 7 years and then fuse with the humeral head between 7 and 13 years of age.
-
-
The joint capsule extends to the metaphysis, rendering some fractures of the metaphysis intracapsular (Fig. 43.2).
-
The primary vascular supply is via the
anterolateral ascending branch of the anterior circumflex artery, with
a small portion of the greater tuberosity and inferior humeral head
supplied by branches from the posterior circumflex artery. -
The physis closes at age 14 to 17 years in girls and at age 16 to 18 years in boys.
-
The physeal apex is posteromedial and is associated with a strong, thick periosteum.
-
Type I physeal fractures occur through
the hypertrophic zone adjacent to the zone of provisional
calcification. The layer of embryonal cartilage is preserved, leading
to normal growth. -
Muscular deforming forces: The
subscapularis attaches to lesser tuberosity. The remainder of the
rotator cuff (teres minor, supraspinatus, and infraspinatus) attaches
to posterior epiphysis and greater tuberosity. The pectoralis major
attaches to anterior medial metaphysis, and the deltoid connects to the
lateral shaft.
-
Indirect: This results from a fall
backward onto an outstretched hand with the elbow extended and the
wrist dorsiflexed. Birth injuries may occur as the arm is hyperextended
or rotated as the infant is being delivered. Shoulder dystocia is
strongly associated with macrosomia from maternal diabetes. -
Direct: Direct trauma to the posterolateral aspect of the shoulder can occur.
 |
|
Figure 43.1. Hyperextension or rotation of the ipsilateral arm may result in a proximal humeral or physeal injury during birth.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Newborns present with pseudoparalysis
with the arm held in extension. A history of birth trauma may be
elicited. A fever is variably present. Infection, clavicle fracture,
shoulder dislocation, and brachial plexus injury must be ruled out. -
Older children present with pain,
dysfunction, swelling, and ecchymosis, and the humeral shaft fragment
may be palpable anteriorly. The shoulder is tender to palpation, with a
painful range of motion that may reveal crepitus. -
Typically, the arm is held in internal rotation to prevent pull of the pectoralis major on the distal fragment.
![]() Figure 43.2. The anatomy of the proximal humerus.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 43.2. The anatomy of the proximal humerus.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
A careful neurovascular examination is required, including the axillary, musculocutaneous, radial, ulnar, and median nerves.
 |
|
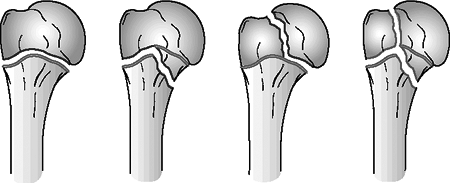
Figure
43.3. Physeal fractures of the proximal humerus. (A) Salter-Harris I. (B) Salter-Harris II. (C) Salter-Harris III. (D) Salter-Harris IV. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Anteroposterior (AP), lateral (in the
plane of the scapula; “Y” view), and axillary views should be obtained,
with comparison views of the opposite side if necessary. -
Ultrasound: This may be necessary in the newborn because the epiphysis is not yet ossified.
-
Computed tomography may be useful to help diagnose and classify posterior dislocations and complex fractures.
-
Magnetic resonance imaging is more useful
than bone scan to detect occult fractures because the physis normally
has increased radionuclide uptake, making a bone scan difficult to
interpret.
| Type I: | Separation through the physis; usually a birth injury |
| Type II: | Usually occurring in adolescents (>12 years); metaphyseal fragment always posteromedial |
| Type III: | Intraarticular fracture; uncommon; associated with dislocations |
| Type IV: | Rare; intraarticular transmetaphyseal fracture; associated with open fractures |
| Grade I: | <5 mm displacement |
| Grade II: | Displacement less than one-third the width of the shaft |
| Grade III: | Displacement one-third to two-thirds the width of the shaft |
| Grade IV: | Displacement greater than two-thirds the width of the shaft, including total displacement |
-
Most fractures are Salter-Harris type I. The prognosis is excellent.
-
Ultrasound can be used to guide reduction.
-
Closed reduction: This is the treatment
of choice and is achieved by applying gentle traction, 90 degrees of
flexion, then 90 degrees of abduction and external rotation. -
Stable fracture: The arm is immobilized against the chest for 5 to 10 days.
-
Unstable fracture: The arm is held abducted and is externally rotated for 3 to 4 days to allow early callus formation.
-
These are typically Salter-Harris type I or, less frequently, type II.
-
Treatment is by closed reduction.
-
The arm is held in a sling for 10 days followed by progressive activity.
-
Extensive remodeling is possible.
-
The metaphyseal fracture (type II) is the
most common in this age group, because this area is undergoing the most
rapid remodeling and is therefore structurally vulnerable. -
Treatment is by closed reduction.
-
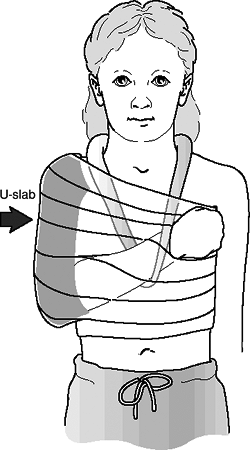
Stable fracture: A sling and swathe is used (Fig. 43.4).
-
Unstable fracture: The arm is placed in a
shoulder spica cast with the arm in the salute position for 2 to 3
weeks, after which the patient may be placed in a sling, with
progressive activity.
-
These are either Salter-Harris type II or, less frequently, type I.
-
Treatment is by closed reduction.
-
There is less remodeling potential than in younger children.
-
Stable fracture: A sling and swathe is used for 2 to 3 weeks followed by progressive range-of-motion exercises.
-
Unstable fracture and Salter Harris type
IV: Immobilization is maintained in a shoulder spica cast with the arm
in the salute position for 2 to 3 weeks, after which the patient may be
placed in a sling, with progressive activity. -
One should consider surgical stabilization for displaced fractures in adolescents.
| Age 1 to 4 years: | 70 degrees of angulation with any amount of displacement |
| Age 5 to 12 years: | 40 to 45 degrees of angulation and displacement of one-half the width of the shaft |
| Age 12 years to maturity: | 15 to 20 degrees of angulation and displacement of <30% the width of the shaft |
 |
|
Figure 43.4. Sling and swathe for immobilization of proximal humeral fracture.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Indications for open reduction and internal fixation include:
-
Open fractures.
-
Fractures with associated neurovascular compromise.
-
Salter-Harris type III and IV fractures with displacement.
-
Irreducible fractures with soft tissue interposition (biceps tendon).
-
-
In children, fixation is most often achieved with percutaneous, smooth Kirschner wires or Steinmann pins.
-
Neer-Horowitz grade I and II fractures do well because of the remodeling potential of the proximal humeral physis.
-
Neer-Horowitz grade III and IV fractures
may be left with up to 3 mm of shortening or residual angulation. This
is well tolerated by the patient and is often clinically insignificant. -
As a rule, the younger the patient, the higher the potential for remodeling and the greater the acceptable initial deformity.
-
Proximal humerus varus: Rare, usually
affecting patients less than 1 year of age, but it may complicate
fractures in patients as old as 5 years of age. It may result in a
decrease of the neck-shaft angle to 90 degrees with humeral shortening
and mild to moderate loss of glenohumeral abduction. Remodeling
potential is great in this age group, however, so observation alone may
result in improvement. Proximal humeral osteotomy may be performed in
cases of extreme functional limitation. -
Limb length inequality: Rarely
significant and tends to occur more commonly in surgically treated
patients as opposed to those treated nonoperatively. -
Loss of motion: Rare and tends to occur
more commonly in surgically treated patients. Older children tend to
have more postfracture difficulties with shoulder stiffness than
younger children. -
Inferior glenohumeral subluxation: May
complicate patients with Salter-Harris Type II fractures of the
proximal humerus secondary to a loss of deltoid and rotator cuff tone.
It may be addressed by a period of immobilization followed by rotator
cuff strengthening exercises. -
Osteonecrosis: May occur with associated
disruption of the anterolateral ascending branch of the anterior
circumflex artery, especially in fractures or dislocations that are not
acutely reduced. -
Nerve injury: Most commonly axillary
nerve injury in fracture-dislocations. Lesions that do not show signs
of recovery in 4 months should be explored. -
Growth arrest: May occur when the physis
is crushed or significantly displaced or when a physeal bar forms. It
may require excision of the physeal bar. Limb lengthening may be
required for functional deficits or severe cosmetic deformity.
-
Most frequent fracture in children (8% to 15% of all pediatric fractures).
-
It occurs in 0.5% of normal deliveries and in 1.6% of breech deliveries (accounts for 90% of obstetric fractures).
-
In macrosomic infants (>4,000 g), the incidence is 13%.
-
Eighty percent of clavicle fractures
occur in the shaft, most frequently just lateral to the insertion of
the subclavius muscle, which protects the underlying neurovascular
structures. -
Ten to 15% of clavicle fractures involve the lateral aspect, with the remainder representing medial fractures.
-
The clavicle is the first bone to ossify; this occurs by intramembranous ossification.
-
The secondary centers develop via endochondral ossification:
-
Clavicular range of motion involves
rotation about its long axis (approximately 50 degrees) accompanied by
elevation of 30 degrees with full shoulder abduction and 35 degrees of
anterior-posterior angulation with shoulder protraction and retraction. -
The periosteal sleeve always remains in the anatomic position. Therefore, remodeling is ensured.
-
Indirect: Fall onto an outstretched hand.
-
Direct: This is the most common
mechanism, resulting from direct trauma to the clavicle or acromion; it
carries the highest incidence of injury to the underlying neurovascular
and pulmonary structures. -
Birth injury: Occurs during delivery of
the shoulders through a narrow pelvis with direct pressure from the
symphysis pubis or from obstetric pressure directly applied to the
clavicle during delivery. -
Medial clavicle fractures or dislocations
usually represent Salter-Harris type I or II fractures. True
sternoclavicular joint dislocations are rare. The inferomedial
periosteal sleeve remains intact and provides a scaffold for
remodeling. Because 80% of the growth occurs at the medial physis,
there is great potential for remodeling. -
Lateral clavicle fractures occur as a
result of direct trauma to the acromion. The coracoclavicular ligaments
always remain intact and are attached to the inferior periosteal tube.
The acromioclavicular ligament is always intact and is attached to the
distal fragment.
-
Birth fractures of the clavicle are
usually obvious, with an asymmetric, palpable mass overlying the
fractured clavicle. An asymmetric Moro reflex is usually present.
Nonobvious injuries may be misdiagnosed as congenital muscular
torticollis because the patient will often turn his or her head toward
the fracture to relax the sternocleidomastoid muscle. -
Children with clavicle fractures
typically present with a painful, palpable mass along the clavicle.
Tenderness is usually discrete over the site of injury, but it may be
diffuse in cases of plastic bowing. There may be tenting of the skin,
crepitus, and ecchymosis. -
Neurovascular status must be carefully
evaluated because injuries to the brachial plexus and upper extremity
vasculature may result. -
Pulmonary status must be assessed,
especially if direct trauma is the mechanism of injury. Medial
clavicular fractures may be associated with tracheal compression,
especially with severe posterior displacement. -
Differential diagnosis
-
Cleidocranial dysostosis: This defect in
intramembranous ossification, most commonly affecting the clavicle, is
characterized by absence of the distal end of the clavicle, a central
P.485
defect, or complete absence of the clavicle. Treatment is symptomatic only.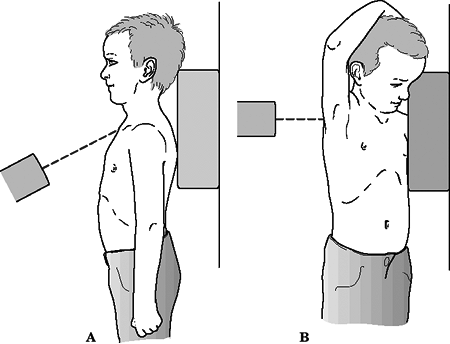 Figure 43.5. (A) Cephalic tilt views. (B) Apical lordotic view.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 43.5. (A) Cephalic tilt views. (B) Apical lordotic view.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Congenital pseudarthrosis: This most
commonly occurs at the junction of the middle and distal thirds of the
right clavicle, with smooth, pointed bone ends. Pseudarthrosis of the
left clavicle is found only in patients with dextrocardia. Patients
present with no antecedent history of trauma, only a palpable bump.
Treatment is supportive only, with bone grafting and intramedullary
fixation reserved for symptomatic cases.
-
-
Ultrasound evaluation may be used in the diagnosis of clavicular fracture in neonates.
-
Because of the S-shape of the clavicle,
an AP view is usually sufficient for diagnostic purposes; however,
special views have been described in cases in which a fracture is
suspected but not well visualized on a standard AP view (Fig. 43.5):-
Cephalic tilt view (cephalic tilt of 35
to 40 degrees): This minimizes overlapping structures to better show
degree of displacement. -
Apical oblique view (injured side rotated
45 degrees toward tube with a cephalic tilt of 20 degrees): This is
best for visualizing nondisplaced middle third fractures.
-
-
Patients with difficulty breathing should
have an AP radiograph of the chest to evaluate possible pneumothorax or
associated rib fractures. -
Computed tomography may be useful for the
evaluation of medial clavicular fractures or suspected dislocation,
because most represent Salter-Harris Type I or II fractures rather than
true dislocations.
 |
|
Figure
43.6. (A) Fracture of the medial third of the clavicle. (B) Fracture of the middle third of the clavicle. (C) Fracture of the lateral third of the clavicle. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Location
-
Open versus closed
-
Displacement
-
Angulation
-
Fracture type: segmental, comminuted, greenstick, etc.
-
Complete fracture in patients less than 2 years of age is unusual and may be caused by birth injury.
-
Clavicle fracture in a newborn will unite
in approximately 1 week. Reduction is not indicated. Care with lifting
and/or a soft bandage may be used. -
Infants may be treated symptomatically
with a simple sling or figure-of-eight bandage applied for 2 to 3 weeks
or until the patient is comfortable. One may also pin the sleeve of a
long-sleeved shirt to the contralateral shoulder.
-
A figure-of-eight bandage or sling is indicated for 2 to 4 weeks, at which time union is complete.
-
The incidence of complete fracture is higher.
-
A figure-of-eight bandage or sling is
used for 3 to 4 weeks. However, figure-of-eight bandages are often
poorly tolerated and have been associated with ecchymosis, compression
of axillary vessels, and brachial plexopathy. -
If the fracture is grossly displaced with
tenting of the skin, one should consider closed or open reduction with
or without internal fixation.
-
Operative treatment is indicated in open fractures and those with neurovascular compromise.
-
Comminuted fragments that tent the skin
may be manipulated and the dermis released from the bone ends with a
towel clip. Typically, bony fragments are placed in the periosteal
sleeve and the soft tissue repaired. One can also consider internal
fixation. -
Bony prominences from callus will usually
remodel; exostectomy may be performed at a later date if necessary,
although from a cosmetic standpoint the surgical scar is often more
noticeable than the prominence.
-
Neurovascular compromise: Rare in
children because of the thick periosteum that protects the underlying
structures, although brachial plexus and vascular injury (subclavian
vessels) may occur with severe displacement. -
Malunion: Rare because of the high
remodeling potential; it is well tolerated when present, and cosmetic
issues of the bony prominence are the only long-term issue. -
Nonunion: Rare (1% to 3%); it is probably associated with a congenital pseudoarthrosis; it never occurs <12 years of age.
-
Pulmonary injury: Rare injuries to the
apical pulmonary parenchyma with pneumothorax may occur, especially
with severe, direct trauma in an anterosuperior to posteroinferior
direction.
-
Rare in children less than 16 years of age.
-
The true incidence is unknown because
many of these injuries actually represent pseudodislocation of the
acromioclavicular joint.
-
The acromioclavicular joint is a diarthrodial joint; in mature individuals, an intraarticular disc is present.
-
The distal clavicle is surrounded by a thick periosteal sleeve that extends to the acromioclavicular joint.
-
Athletic injuries and falls comprise the majority of acromioclavicular injuries, with direct trauma to the acromion.
-
Unlike acromioclavicular injuries in
adults, in children the coracoclavicular (conoid and trapezoid)
ligaments remain intact. Because of the tight approximation of the
coracoclavicular ligaments to the periosteum of the distal clavicle,
true dislocation of the acromioclavicular joint is rare. -
The defect is a longitudinal split in the
superior portion of the periosteal sleeve through which the clavicle is
delivered, much like a banana being peeled from its skin.
-
The patient should be examined while in
the standing or sitting position to allow the upper extremity to be
dependent, thus stressing the acromioclavicular joint and emphasizing
deformity. -
A thorough shoulder examination should be
performed, including assessment of neurovascular status and possible
associated upper extremity injuries. Inspection may reveal an apparent
step-off deformity of the injured acromioclavicular joint, with
possible tenting of the skin overlying the distal clavicle. Range of
motion may be limited by pain. Tenderness may be elicited over the
acromioclavicular joint.
-
A standard trauma series of the shoulder
(AP, scapular-Y, and axillary views) is usually sufficient for the
recognition of acromioclavicular injury, although closer evaluation
includes targeted views of the AC joint, which requires one-third to
one-half the radiation to avoid overpenetration. -
Ligamentous injury may be assessed via
stress radiographs, in which weights (5 to 10 lb) are strapped to the
wrists and an AP radiograph is taken of both shoulders for comparison.
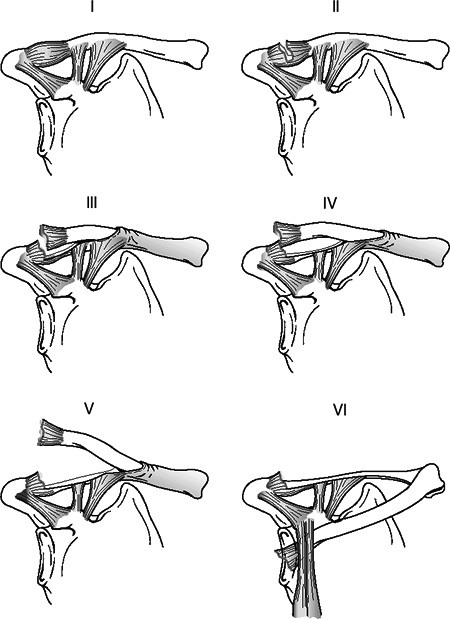
| Type I: | Mild sprain of the acromioclavicular ligaments without periosteal tube disruption; distal clavicle stable to examination and no radiographic abnormalities |
| Type II: | Partial disruption of the periosteal tube with mild distal clavicle instability; slight widening of the acromioclavicular space appreciated on radiographs |
| Type III: | Longitudinal split of the periosteal tube with gross instability of the distal clavicle to examination; superior displacement of 25% to 100% present on radiographs as compared with the normal, contralateral shoulder |
| Type IV: | Posterior displacement of the distal clavicle through a periosteal sleeve disruption with buttonholing through the trapezius; AP radiographs demonstrating superior displacement similar to type II injuries, but axillary radiographs demonstrating posterior displacement |
| Type V: | Type III injury with >100% displacement; distal clavicle may be subcutaneous to palpation, with possible disruption of deltoid or trapezial attachments |
| Type VI: | Infracoracoid displacement of the distal clavicle as a result of a superior-to-inferior force vector |
 |
|
Figure 43.7. Dameron and Rockwood classification of distal/lateral fractures.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
For Types I to III, nonoperative
treatment is indicated, with sling immobilization, ice, and early
range-of-motion exercises as pain subsides. Remodeling is expected.
Complete healing generally takes place in 4 to 6 weeks. -
Treatment for Types IV to VI is
operative, with reduction of the clavicle and repair of the periosteal
sleeve. Internal fixation may be needed.
-
Open lesion: Severe displacement of the
distal clavicle, such as with Type V acromioclavicular dislocation, may
result in tenting of the skin, with possible laceration necessitating
irrigation and debridement.
-
The scapula is relatively protected from
trauma by the thoracic cavity and the rib cage anteriorly as well as by
the encasing musculature. -
Scapular fractures are often associated with other life-threatening injuries that have greater priority.
-
These constitute only 1% of all fractures
and 5% of shoulder fractures in the general population and are even
less common in children.
-
The scapula forms from intramembranous ossification. The body and spine are ossified at birth.
-
The center of the coracoid is ossified at
1 year. The base of the coracoid and the upper one-fourth of the
glenoid ossify by 10 years. A third center at the tip of the coracoid
ossifies at a variable time. All three structures fuse by age 15 to 16
years. -
The acromion fuses by age 22 years via two to five centers, which begin to form at puberty.
-
Centers for the vertebral border and
inferior angle appear at puberty and fuse by age 22 years. The center
for the lower three-fourths of the glenoid appears at puberty and fuses
by age 22 years. -
The suprascapular nerve traverses the
suprascapular notch on the superior aspect of the scapula, medial to
the base of the coracoid process, thus rendering it vulnerable to
fractures in this region. -
The superior shoulder suspensory complex
(SSSC) is a circular group of both bony and ligamentous attachments
(acromion, glenoid, coracoid, coracoclavicular ligament, and distal
clavicle). The integrity of the ring is breached only after more than
one violation. This can dictate the treatment approach (Fig. 43.8).
-
In children, most scapula fractures
represent avulsion fractures associated with glenohumeral joint
injuries. Other fractures are usually the result of high-energy trauma. -
Isolated scapula fractures are extremely
uncommon, particularly in children; child abuse should be suspected
unless a clear and consistent mechanism of injury exists. -
The presence of a scapula fracture should
raise suspicion of associated injuries, because 35% to 98% of scapula
fractures occur in the presence of other injuries including:-
Ipsilateral upper torso injuries: fractured ribs, clavicle, sternum, shoulder trauma.
-
Pneumothorax: seen in 11% to 55% of scapular fractures.
![]() Figure
Figure
43.8. Superior shoulder suspensory complex. (A) Anteroposterior view of
the bone–soft tissue ring and superior and inferior bone struts. (B)
Lateral view of the bone–soft tissue ring.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Pulmonary contusion: present in 11% to 54% of scapula fractures.
-
Injuries to neurovascular structures: brachial plexus injuries, vascular avulsions.
-
Spinal column injuries: 20% lower cervical spine, 76% thoracic spine, 4% lumbar spine.
-
Others: concomitant skull fractures,
blunt abdominal trauma, pelvic fracture, and lower extremity injuries,
which are all seen with higher incidences in the presence of a scapula
fracture.
P.491 -
-
Rate of mortality in setting of scapula fractures may approach 14%.
-
Full trauma evaluation, with attention to
airway, breathing, circulation, disability, and exposure should be
performed, if indicated. -
Patients typically present with the upper
extremity supported by the contralateral hand in an adducted and
immobile positions, with painful range of shoulder motion, especially
with abduction. -
A careful examination for associated
injures should be pursued, with a comprehensive assessment of
neurovascular status and an evaluation of breath sounds.
-
Initial radiographs should include a
trauma series of the shoulder, consisting of true AP, axillary, and
scapular-Y (true scapular lateral) views; these generally are able to
demonstrate most glenoid, neck, body, and acromion fractures.-
The axillary view may be used to delineate acromial and glenoid rim fractures further.
-
An acromial fracture should not be confused with an os acromiale,
which is a rounded, unfused apophysis at the epiphyseal level and is
present in approximately 3% of the population. When present, it is
bilateral in 60% of cases. The os is typically in the anteroinferior
aspect of distal acromion. -
Glenoid hypoplasia, or scapular neck dysplasia,
is an unusual abnormality that may resemble glenoid impaction and may
be associated with humeral head or acromial abnormalities. It has a
benign course and is usually noted incidentally.
P.492 -
-
A 45-degree cephalic tilt (Stryker notch) radiograph is helpful to identify coracoid fractures.
-
Computed tomography may be useful for further characterizing intraarticular glenoid fractures.
-
Because of the high incidence of
associated injuries, especially to thoracic structures, a chest
radiograph is an essential part of the evaluation.
| I. | Isolated versus associated disruption of the clavicle |
| II. | Displaced versus nondisplaced |
| IA: | Anterior avulsion fracture |
| IB: | Posterior rim avulsion |
| II: | Transverse with inferior free fragment |
| III: | Upper third including coracoid |
| IV | Horizontal fracture extending through body |
| V: | Combined II, III, and IV |
| VI: | Extensively comminuted |
-
These can be associated with scapular neck fractures and shoulder dislocations.
-
Treatment is nonoperative in most cases.
Open reduction and internal fixation are indicated if a large anterior
or posterior rim fragment is associated with glenohumeral instability.
-
These are avulsion-type injuries, usually
occurring through the common physis of the base of the coracoid and the
upper one-fourth of the glenoid. -
The coracoacromial ligament remains intact, but the acromioclavicular ligaments may be stretched.
| I: | Nondisplaced |
| IA: | Avulsion |
| IB: | Direct trauma |
| II: | Displaced without subacromial narrowing |
| III: | Displaced with subacromial narrowing |
-
These are rare, usually the result of a direct blow.
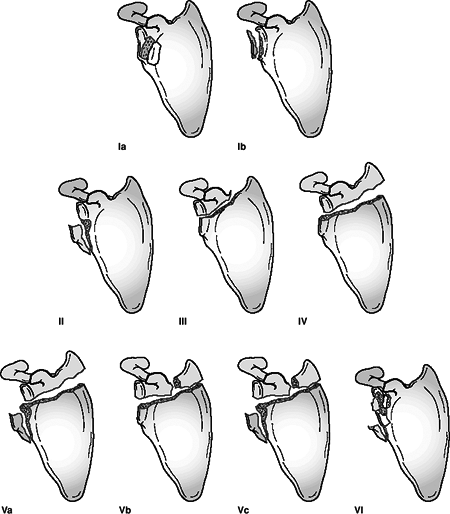 Figure 43.9. General classification of scapular/glenoid fractures.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 43.9. General classification of scapular/glenoid fractures.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
The os acromiale, which is an unfused ossification center, should not be mistaken for a fracture.
-
Conservative treatment is recommended unless there is severe displacement of the acromioclavicular joint.
-
Scapula body fractures in children are
treated nonoperatively, with the surrounding musculature maintaining
reasonable proximity of fracture fragments. Operative treatment is
indicated for fractures that fail to unite, which may benefit from
partial body excision. -
Scapula neck fractures that are
nondisplaced and not associated with clavicle fractures may be treated
nonoperatively. Significantly displaced fractures may be treated in a
thoracobrachial
P.494
cast.
Associated clavicular disruption, either by fracture or ligamentous
instability (i.e., multiple disruptions in the SSSC) are generally
treated operatively with open reduction and internal fixation of the
clavicle alone or include open reduction and internal fixation of the
scapula fracture though a separate incision. -
Coracoid fractures that are nondisplaced
may be treated with sling immobilization. Displaced fractures are
usually accompanied by acromioclavicular dislocation or lateral
clavicular injury and should be treated with open reduction and
internal fixation. -
Acromial fractures that are nondisplaced
may be treated with sling immobilization. Displaced acromial fractures
with associated subacromial impingement should be reduced and
stabilized with screw or plate fixation. -
Glenoid fractures in children, if not
associated with glenohumeral instability, are rarely symptomatic when
healed and can generally be treated nonoperatively if they are
nondisplaced.
| Type I: | Fractures involving greater than one fourth of the glenoid fossa that result in instability may be amenable to open reduction and lag screw fixation. |
| Type II: | Inferior subluxation of the humeral head may result, necessitating open reduction, especially when associated with a greater than 5 mm articular step-off. An anterior approach usually provides adequate exposure. |
| Type III: | Reduction may be difficult; fracture occurs through the junction between the ossification centers of the glenoid and are often accompanied by a fractured acromion or clavicle, or an acromioclavicular separation. Open reduction and internal fixation followed by early range of motion are indicated. |
| Types IV, V, VI: | These are difficult to reduce, with little bone stock for adequate fixation in pediatric patients. A posterior approach is generally utilized for open reduction and internal fixation with Kirschner wire, plate, suture, or screw fixation for displaced fractures. |
-
Posttraumatic osteoarthritis: This may result from a failure to restore articular congruity.
-
Associated injuries: These account for most serious complications because of the high-energy nature of these injuries.
-
Decreased shoulder motion: Secondary to subacromial impingement from acromial fracture.
-
Malunion: Fractures of the scapula body
generally unite with nonoperative treatment; when malunion occurs, it
is generally well tolerated but may result in painful scapulothoracic
crepitus. -
Nonunion: Extremely rare, but when present and symptomatic it may require open reduction and plate fixation for adequate relief.
-
Suprascapular nerve injury: May occur in
association with scapula body, scapula neck, or coracoid fractures that
involve the suprascapular notch.
-
Rare in children; Rowe reported that only
1.6% of shoulder dislocations occurred in patients <10 years of age,
whereas 10% occurred in patients 10 to 20 years of age. -
Ninety percent are anterior dislocations.
-
The glenohumeral articulation, with its
large convex humeral head and correspondingly flat glenoid, is ideally
suited to accommodate a wide range of shoulder motion. The articular
surface and radius of curvature of the humeral head are about three
times those of the glenoid fossa. -
Numerous static and dynamic stabilizers of the shoulder exist; these are covered in detail in Chapter 14.
-
The humeral attachment of the
glenohumeral joint capsule is along the anatomic neck of the humerus
except medially, where the attachment is more distal along the shaft.
The proximal humeral physis is therefore extraarticular except along
its medial aspect. -
As in most pediatric joint injuries, the
capsular attachment to the epiphysis renders failure through the physis
much more common than true capsuloligamentous injury; therefore,
fracture through the physis is more common than a shoulder dislocation
in a skeletally immature patient. -
In neonates, an apparent dislocation may actually represent a physeal injury.
-
Neonates: Pseudodislocation may occur
with traumatic epiphyseal separation of the proximal humerus. This is
much more common than a true shoulder dislocation, which may occur in
neonates with underlying birth trauma to the brachial plexus or central
nervous system. -
Anterior glenohumeral dislocation may occur as a result of trauma, either direct or indirect.
-
Direct: An anteriorly directed impact to the posterior shoulder may produce an anterior dislocation.
-
Indirect: Trauma to the upper extremity
with the shoulder in abduction, extension, and external rotation is the
most common mechanism for anterior shoulder dislocation.
-
-
Posterior glenohumeral dislocation (2% to 4%):
-
Direct trauma: This results from force application to the anterior shoulder, forcing the humeral head posteriorly.
-
Indirect trauma: This is the most common mechanismP.496
-
The shoulder typically is in the position of adduction, flexion, and internal rotation at the time of injury with axial loading.
-
Electric shock or convulsive mechanisms
may produce posterior dislocation owing to the overwhelming of the
external rotators of the shoulder (infraspinatus and teres minor
muscles) by the internal rotators (latissimus dorsi, pectoralis major,
and subscapularis muscles).
-
-
-
Atraumatic dislocations: Recurrent
instability related to congenital or acquired laxity or volitional
mechanisms may result in anterior dislocation with minimal trauma.
-
Patient presentation varies according to the type of dislocation encountered.
-
The patient typically presents with the
affected upper extremity held in slight abduction and external
rotation. The acutely dislocated shoulder is painful, with muscular
spasm in an attempt to stabilize the joint. -
Examination typically reveals squaring of
the shoulder caused by a relative prominence of the acromion, a
relative hollow beneath the acromion posteriorly, and a palpable mass
anteriorly. -
A careful neurovascular examination is
important with attention to axillary nerve integrity. Deltoid muscle
testing is usually not possible, but sensation over the deltoid may be
assessed. Deltoid atony may be present and should not be confused with
axillary nerve injury. Musculocutaneous nerve integrity can be assessed
by the presence of sensation on the anterolateral forearm. -
Patients may present after spontaneous
reduction or reduction in the field. If the patient is not in acute
pain, examination may reveal a positive apprehension test,
in which passive placement of the shoulder in the provocative position
(abduction, extension, and external rotation) reproduces the patient’s
sense of instability and pain. Posteriorly directed counterpressure
over the anterior shoulder may mitigate the sensation of instability.
-
Clinically, a posterior glenohumeral
dislocation does not present with striking deformity; moreover, the
injured upper extremity is typically held in the traditional sling
position of shoulder internal rotation and adduction. -
A careful neurovascular examination is
important to rule out axillary nerve injury, although it is much less
common than with anterior glenohumeral dislocations. -
On examination, limited external rotation
(often <0 degrees) and limited anterior forward elevation (often
<90 degrees) may be appreciated. -
A palpable mass posterior to the shoulder, flattening of the anterior shoulder, and coracoid prominence may be observed.
-
Patients present with a history of recurrent dislocations with spontaneous reduction.
-
Often the patient will report a history of minimal trauma or volitional dislocation, frequently without pain.
-
Multidirectional instability may be
present bilaterally, as may characteristics of multiple joint laxity,
including hyperextensibility of the elbows, knees, and
metacarpophalangeal joints. Skin striae may be present. -
Sulcus sign: This is dimpling of skin below the acromion with longitudinal traction.
-
This is extremely rare in children, although cases have been reported.
-
It may be associated with hereditary conditions such as Ehlers-Danlos syndrome.
-
A trauma series of the affected shoulder is indicated: AP, scapular-Y, and axillary views.
-
Velpeau axillary view: Compliance is
frequently an issue in the irritable, injured child in pain. If a
standard axillary view cannot be obtained, the patient may be left in a
sling and leaned obliquely backward 45 degrees over the cassette. The
beam is directed caudally, orthogonal to the cassette, resulting in an
axillary view with magnification. -
Special views (See Chapter 14):
-
West Point axillary view: Taken with the
patient prone with the beam directed cephalad to the axilla 25 degrees
from the horizontal and 25 degrees medially. It provides a tangential
view of the anteroinferior glenoid rim. -
Hill-Sachs view: An AP radiograph is
taken with the shoulder in maximal internal rotation to visualize
posterolateral defect (Hill-Sachs lesion) caused by an impression
fracture on the glenoid rim. -
Stryker notch view: The patient is supine
with the ipsilateral palm on the crown of head and the elbow pointing
straight upward. The x-ray beam is directed 10 degrees cephalad, aimed
at coracoid. One is able to visualize 90% of posterolateral humeral
head defects.
-
-
Computed tomography may be useful in
defining humeral head or glenoid impression fractures, loose bodies,
and anterior labral bony injuries (bony Bankart lesion). -
Single- or double-contrast arthrography
may be utilized in cases in which the diagnosis may be unclear; it may
demonstrate pseudosubluxation, or traumatic epiphyseal separation of
the proximal humerus, in a neonate with an apparent glenohumeral
dislocation. -
Magnetic resonance imaging may be used to identify rotator cuff, capsular, and glenoid labral (Bankart lesion) pathology.
-
Atraumatic dislocations may demonstrate congenital aplasia or absence of the glenoid on radiographic evaluation.
| Degree of stability: | Dislocation versus subluxation |
| Chronology: | Congenital Acute versus chronic Locked (fixed) Recurrent Acquired: generally from repeated minor injuries (swimming, gymnastics, weights); labrum often intact; capsular laxity; increased glenohumeral joint volume; subluxation common |
| Force: | Atraumatic: usually owing to congenital laxity; no injury; often asymptomatic; self-reducing |
| Traumatic: usually caused by one major injury; the anteroinferior labrum may be detached (Bankart lesion); unidirectional; generally requires assistance for reduction |
|
| Patient contribution: | Voluntary versus involuntary |
| Direction: | Subcoracoid Subglenoid Intrathoracic |
-
Closed reduction should be performed
after adequate clinical evaluation and administration of analgesics and
or sedation. Described techniques include (see the figures in Chapter 14):-
Traction-countertraction:
With the patient in the supine position, a sheet is placed in the
axilla of the affected shoulder with traction applied to counter axial
traction placed on the affected upper extremity. Steady, continuous
traction eventually results in fatigue of the shoulder musculature in
spasm and allows reduction of the humeral head. -
Stimson technique:
The patient is placed prone on the stretcher with the affected upper
extremity hanging free. Gentle, manual traction or 5 lb of weight is
applied to the wrist, with reduction effected over 15 to 20 minutes. -
Steel maneuver:
With the patient supine, the examiner supports the elbow in one hand
while supporting the forearm and wrist with the other. The upper
extremity is abducted to 90 degrees and is slowly externally rotated.
Thumb pressure is applied by the physician to push the humeral head
into place, followed by adduction and internal rotation of the shoulder
as the extremity is placed across the chest. There is a higher
incidence of iatrogenic fracture.
-
-
Following reduction, acute anterior
dislocations are treated with sling immobilization. Total time in sling
is controversial but may be up to 4 weeks, after which an aggressive
program of rehabilitation for rotator cuff strengthening is instituted.
Posterior dislocations are treated for 4 weeks in a commercial splint
or shoulder spica cast with the shoulder in neutral rotation, followed
by physical therapy. -
Recurrent dislocation or associated
glenoid rim avulsion fractures (bony Bankart lesion) may necessitate
operative management, including reduction and internal fixation of the
anterior glenoid margin, repair of a Bankart lesion (anterior labral
tear), capsular shift, or capsulorraphy. Postoperatively, the child is
placed in sling immobilization for 4 to 6 weeks with gradual increases
in range-of-motion and strengthening exercises. -
Atraumatic dislocations rarely require
reduction maneuvers as spontaneous reduction is the rule. Only after an
aggressive, supervised rehabilitation program for rotator cuff and
deltoid strengthening has been completed should surgical intervention
be considered. Vigorous rehabilitation may obviate the need for
operative intervention in up to 85% of cases. -
Psychiatric evaluation may be necessary in the management of voluntary dislocators.
-
Recurrent dislocation: The incidence is
50% to 90%, with decreasing rates of recurrence with increasing patient
age (up to 100% in children less than 10 years old). It may necessitate
operative intervention, with >90% success rate in preventing future
dislocation. -
Shoulder stiffness: Procedures aimed at
tightening static and dynamic constraints (subscapularis
tendon-shortening, capsular shift, etc.) may result in
“overtightening,” resulting in a loss of range of motion, as well as
possible subluxation in the opposing direction with subsequent
accelerated glenohumeral arthritis. -
Neurologic injury: Neurapraxic injury may
occur to nerves in proximity to the glenohumeral articulation,
especially the axillary nerve and less commonly the musculocutaneous
nerve. These typically resolve with time; a lack of neurologic recovery
by 3 months may warrant surgical exploration. -
Vascular injury: Traction injury to the
axillary artery has been reported in conjunction with nerve injury to
the brachial plexus.


