Spina Bifida
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Spina Bifida
Spina Bifida
Paul D. Sponseller MD
Description
-
Incomplete closure of the laminar arches of the spine (Fig. 1)
-
Occurs at birth but may not be detected until later
-
An unrelated variety, spina bifida
occulta, is a small defect in the 5th lumbar or 1st sacral arches, a
benign finding of no clinical consequence. -
May be a clinically significant problem if it is associated with congenital neurologic deficit at the open bony levels
-
May occur at any level of the spine or at multiple levels, although it is most common at the caudal aspect of the spine
-
In the presence of a neurologic deficit, secondary problems may develop in the genitourinary tract and lower limbs.
-
Classification:
-
Spina bifida occulta: Skin-covered defect
in the lower lumbar spine with no neurologic deficit, associated with
slightly increased risk of spondylolisthesis -
Myelomeningocele:
-
Combination of several absent laminae, with exposed meninges and usually neurologic deficit at the same level
-
High risk of hydrocephalus
-
-
Lipomeningocele:
-
Caudal fatty mass arising from the spinal
canal, palpable under the skin, with an associated neurologic deficit
but no substantial risk of hydrocephalus (1)
-
-
-
All patients with spina bifida should be classified by motor level (i.e., the lowest level with antigravity strength).
-
Synonyms: Spinal dysraphism; Neural tube defect; Myelomeningocele
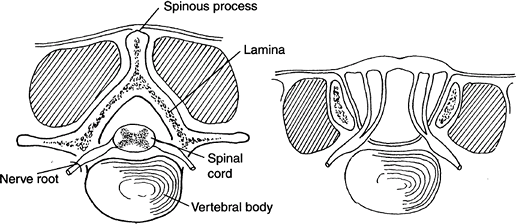 Fig. 1. Normal posterior spinal elements (left) are disrupted in spina bifida (right).
Fig. 1. Normal posterior spinal elements (left) are disrupted in spina bifida (right).
General Prevention
Folate, 0.4 mg daily, used in the 1st few months of pregnancy, may prevent spina bifida.
Epidemiology
Males and females are affected equally.
Incidence
-
The incidence of spina bifida occulta is 2–3% of the general population (2).
-
The overall incidence of neural tube defects in the United States is ~1 per 1,000 births (2).
-
The risk of occurrence in 1st-degree relatives is slightly higher than that in the general population (3.2%) (2).
Prevalence
-
Slightly higher in Caucasians and lower in African Americans than in the general population (1,2).
-
The rate varies from country to country.
Risk Factors
-
Affected 1st-degree relatives
-
Poor perinatal nutrition
Genetics
-
Not inherited in a Mendelian fashion
-
Follows a polygenic pattern
-
No known single genetic defect
Etiology
-
Failure of closure or late rupture of neural tube:
-
Mechanism of this failure is unknown.
-
Associated Conditions
-
Hydrocephalus
-
Chiari malformation
-
Syringomyelia
-
Kyphosis
-
Scoliosis
-
Renal problems
-
Latex allergies
-
Sprengel deformity
-
Pathologic fracture
Signs and Symptoms
-
Local signs:
-
Abnormality in the skin of the back over site of lesion, ranging from a dimple to a hairy or vascular marking
-
Fatty mass (lipomeningocele)
-
Exposure of the meninges (myelomeningocele)
-
Spina bifida occulta has no physical signs.
-
-
Generalized signs:
-
Motor weakness
-
Atrophy of the calf or thigh
-
Sensory defect corresponding to the motor defect
-
Neurogenic bladder
-
-
Symptoms:
-
None are attributable directly to the
spina bifida, except that it predisposes to an increased incidence of
tethered cord and spondylolisthesis, which may cause backache.
-
Physical Exam
-
Examine the patient for scoliosis and kyphosis.
-
Note the quality of the skin covering because it predicts the late risk of breakdown.
-
Record the motor level of the lesion on each limb as the lowest that has contraction against resistance.
-
Record the strength in the major muscle groups for future comparison.
-
Record the lowest level of sensation because it predicts pressure sores.
-
Note the presence of contractures or deformities of each joint.
-
Observe the patient’s gait, if possible.
-
Look for signs of hydrocephalus or Chiari malformation (Fig. 2).
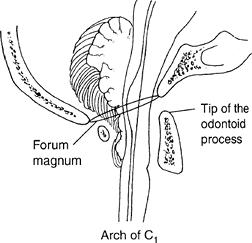 Fig. 2. Chiari malformation with cerebellar compression may cause brainstem symptoms in spina bifida.
Fig. 2. Chiari malformation with cerebellar compression may cause brainstem symptoms in spina bifida.
P.411
Tests
Lab
-
Prenatal screening with amniocentesis and
determination of α-fetoprotein and acetylcholinesterase are available
for those at increased risk of a neural tube defect. -
Ultrasound may be used as a prenatal imaging test.
Imaging
-
Radiography:
-
Baseline radiography of the spine early
in infancy to rule out congenital anomalies such as hemivertebrae and
fusion between vertebrae, which are present in up to 20% of children
with true spina bifida (1,3) -
Baseline AP pelvis radiograph
-
-
MRI of the neuraxis, if needed, to determine the presence of a syrinx, Chiari malformation, or tether of the spinal cord
Pathological Findings
-
The pathologic features of a typical
myelomeningocele include a flattened spinal cord with scarring and
abnormal neural elements. -
Often present is associated hydrocephalus
or Chiari malformation with herniation of the cerebellar tonsils
through the foramen magnum.
Differential Diagnosis
-
Defect from previous laminectomy
-
Radiographic delay in ossification of an intact arch
General Measures
-
An experienced neurologist, as well as a neurosurgeon, orthopaedic surgeon, and urologist, should see the child at birth.
-
Avoid latex exposure (4).
-
Offer genetic counseling to the family.
-
Prescribe long-term, low-dose prophylactic antibiotic therapy for patients with recurrent urinary tract infections.
-
Monitor motor strength and sensory level and record throughout the patient’s life to detect tethering or other complications.
-
Treat clubfoot deformities by casting initially.
-
Treat other deformities by stretching, bracing, or surgery.
-
Teach the family how to protect insensate skin.
-
Involve the family in a support group such as the Spina Bifida Association of America.
-
Some instances of hip subluxation do not
need surgery, especially if the condition is high and bilateral in a
nonambulatory patient.
Activity
-
Encourage patients to maximize activity by the most efficient means, either by using a wheelchair or by walking with braces.
-
Offer wheelchair sports to those athletically inclined, as a means of building social skills and self-image.
Special Therapy
Physical Therapy
-
Patients should be followed throughout
growth to maximize mobility, to monitor use of equipment (wheelchair or
braces), and to monitor muscle strength. -
A therapist and a nutritionist may help the patient to prevent weight gain.
Surgery
-
Clubfoot:
-
The 1st step is the Ponseti treatment (2,5) (casting), which may result in partial or total correction.
-
Surgery, if needed, to lengthen tendons and realign bones to create a foot that will be flat on the ground
-
-
Other foot and leg correction may be offered as needed.
-
Spine surgery is indicated for patients
with scoliosis or kyphosis causing unbalanced sitting, to straighten
and fuse the spine with implanted rods (3,6).
Prognosis
-
Currently, infant mortality is only
slightly higher than that in the general population, especially for
those with severe degrees of spina bifida cystica, because of excellent
neonatal care. -
Long-term independence is not possible for some patients with central nervous system complications.
Complications
-
Shunt failure
-
Cord tethering at the site of opening, causing weakness with growth
-
Fracture: Higher risk with higher neurologic deficit
-
Signs of fracture in patient with spina bifida include:
-
Low-grade fever
-
Swelling
-
Warmth without pain
-
-
-
Pressure sore over insensate skin, especially of the ischium, foot, or trochanter
-
Renal failure secondary to poor self-care
Patient Monitoring
-
Follow patients with myelomeningocele every 4–6 months (5):
-
To detect new deformities
-
To monitor the fit of braces and equipment (6,7)
-
To monitor for signs of neurologic deterioration (1), which may be secondary to shunt failure, syrinx (cyst in the cord), tethering of the cord, or Chiari malformation
-
References
1. McLone DG, Herman JM, Gabrieli AP, et al. Tethered cord AS a cause of scoliosis in children with a myelomeningocele. Pediatr Neurosurg 1990;16:8–13.
2. Lindseth
RE. Myelomeningocele. In: Morrissy RT, Weinstein SL, eds. Lovell and
Winter’s Pediatric Orthopaedics, 5th ed. Philadelphia: Lippincott
Williams & Wilkins, 2001:601–632.
RE. Myelomeningocele. In: Morrissy RT, Weinstein SL, eds. Lovell and
Winter’s Pediatric Orthopaedics, 5th ed. Philadelphia: Lippincott
Williams & Wilkins, 2001:601–632.
3. Guille
JT, Sarwark JF, Sherk HH, et al. Congenital and developmental
deformities of the spine in children with myelomeningocele. J Am Acad Orthop Surg 2006;14:294–302.
JT, Sarwark JF, Sherk HH, et al. Congenital and developmental
deformities of the spine in children with myelomeningocele. J Am Acad Orthop Surg 2006;14:294–302.
4. Tosi LL, Slater JE, Shaer C, et al. Latex allergy in spina bifida patients: Prevalence and surgical implications. J Pediatr Orthop 1993;13:709–712.
5. Asher M, Olson J. Factors affecting the ambulatory status of patients with spina bifida cystica. J Bone Joint Surg 1983;65A:350–356.
6. Mazur JM, Kyle S. Efficacy of bracing the lower limbs and ambulation training in children with myelomeningocele. Dev Med Child Neurol 2004;46:352–356.
7. Mitchell LE, Adzick NS, Melchionne J, et al. Spina bifida. Lancet 2004;364:1885–1895.
Codes
ICD9-CM
-
741.93 Lumbar spina bifida
-
756.17 Spina bifida occulta
Patient Teaching
-
Teach which products contain latex and how to avoid them.
-
Discuss signs and symptoms of shunt failure, if applicable.
-
Teach prevention of skin pressure sores.
-
Teach bowel and bladder continence.
-
Encourage weight control early in childhood.
Prevention
Folate, 0.4 mg daily, used periconceptually, may prevent spina bifida.
FAQ
Q: If my 1st child has spina bifida occulta, what are my chances that a subsequent child will have spina bifida cystica?
A:
The risk is approximately the same as that of the general population.
Spina bifida occulta does not increase appreciably the risk of neural
tube defects.
The risk is approximately the same as that of the general population.
Spina bifida occulta does not increase appreciably the risk of neural
tube defects.
Q: Do patients with spina bifida have normal intelligence?
A:
Intelligence varies widely. Hydrocephalus and its complications can
take its toll. In general, the mean IQ is diminished somewhat in the
population with spina bifida, but many patients can become independent
and receive advanced degrees.
Intelligence varies widely. Hydrocephalus and its complications can
take its toll. In general, the mean IQ is diminished somewhat in the
population with spina bifida, but many patients can become independent
and receive advanced degrees.
Q: What are the chances that my child with spina bifida can walk?
A: They vary with the motor level of the child. Patients affected at a high lumbar level or above do little functional walking.
