CHAPTER 37 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 37 – Ulnar Collateral Ligament Reconstruction
Champ L. Baker III, MD
Injury to the medial side of the elbow is common in overhead athletes, such as baseball pitchers, tennis players, and javelin throwers. The overhead throwing motion places a tremendous amount of valgus stress on the elbow that is resisted by the medial structures. The anterior bundle of the ulnar collateral ligament (UCL) has been demonstrated to be the primary restraint to valgus stress about the elbow.[6] Repeated high valgus stresses imparted from the repetitive act of throwing can result in chronic attenuation or acute rupture of the UCL. In the throwing athlete, UCL insufficiency can be manifested as disabling elbow pain with the inability to compete effectively. Since the first description of UCL reconstruction in the landmark work of Jobe et al,[8] there have been several modifications to the original technique. These modifications have attempted to reduce the amount of soft tissue dissection and the incidence of ulnar nerve complications and to provide more consistent and secure fixation. Constants in all described techniques include accurate diagnosis, appropriate selection of patients, anatomic reconstruction of the anterior bundle of the UCL, and maintenance of a specific rehabilitation program to allow the athlete to return successfully to sport.
The typical history in a throwing athlete with UCL injury is episodic medial elbow pain that prevents him or her from competing effectively. Pain is usually elicited in the early acceleration phase of throwing. Affected pitchers complain of loss of velocity or accuracy. On occasion, the athlete will sustain an acute injury with sudden onset of medial pain accompanied by a “pop” followed by an inability to continue throwing. Symptoms of ulnar nerve irritability, such as paresthesias, in the little and ring fingers may also be present.
A thorough physical examination of the throwing athlete includes the following:
Several tests have been described to evaluate the integrity of the UCL:
| • | Manual valgus stress test performed at 30 degrees of elbow flexion | |
| • | “Milking maneuver”[16] | |
| • | Moving valgus stress test[10] |
These tests may elicit medial elbow pain with valgus stress, or the examiner may appreciate medial joint line opening with stress especially in comparison with the contralateral elbow. Consideration of concurrent posteromedial impingement in the thrower’s elbow can be evaluated with the valgus extension overload test.[2] If reconstruction of the UCL is considered, the presence of an ipsilateral or contralateral palmaris longus should be assessed.
| • | Anteroposterior, lateral, and axial views of the elbow |
Plain radiographs are inspected for loose bodies, evidence of degenerative changes such as posteromedial osteophytes of the olecranon, medial joint line spurring, and possible calcifications in the UCL indicative of a chronic injury.
| • | Computed tomographic arthrography | |
| • | Magnetic resonance imaging |
The senior author prefers magnetic resonance imaging as the imaging modality of choice for detailed characterization of the integrity of the UCL and evaluation of other soft tissue structures (
Fig. 37-1
).
|
|
|
|
Figure 37-1 |
Indications and Contraindications
The indication for UCL reconstruction in a throwing athlete is medial elbow pain associated with UCL insuffi ciency that prevents the athlete from competing effectively. Nonoperative treatment for elite throwing athletes is usually unsuccessful.[12] Athletes who do not plan on returning to sport and those who are able to return to sport after rehabilitation and do not subject their elbows to repeated valgus stress are not generally considered candidates for reconstruction.[4]
Concomitant procedures include ulnar nerve transposition based on preoperative symptoms suggestive of nerve irritability or subluxation. Findings of loose bodies, spurs, and posteromedial impingement can be addressed either arthroscopically or through an arthrotomy at the time of the reconstruction.
The initial graft choice is an ipsilateral palmaris longus tendon. If the tendon is not present in the patient, other choices are the contralateral palmaris longus tendon if it is present, gracilis or semitendinosus tendons, toe extensor, and allograft.
We prefer to perform the procedure under axillary block anesthesia, although on the basis of the surgeon’s, patient’s, and anesthesiologist’s preferences, general anesthesia or a combination of general and regional anesthesia can be used. The patient is placed supine on the operating table with the affected extremity abducted and placed on an attached hand table. A sterile or nonsterile pneumatic tourniquet is placed about the arm as proximal as possible for exposure. The arm is then prepared and draped in the usual sterile fashion.
Specific Steps (
Box 37-1
)
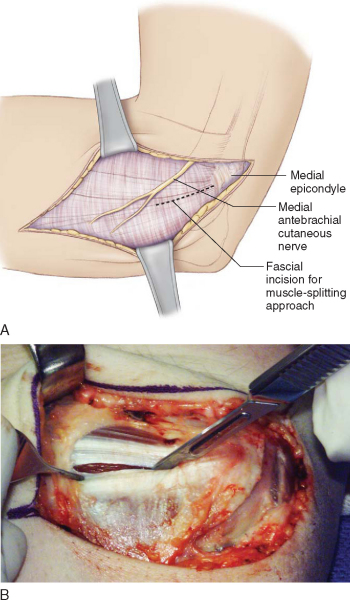
The limb is exsanguinated, and the tourniquet is inflated. The medial epicondyle is identified, and an approximately 8- to 10-cm curvilinear incision is made centered over the medial epicondyle. During the exposure, care is taken to identify and to protect the branches of the medial antebrachial cutaneous nerve that cross the operative field. Injury to these nerves can result in either sensory loss along the medial aspect of the forearm or a painful neuroma. Dissection is carried down to the level of the forearm fascia and the flexor-pronator aponeurosis (
Fig. 37-2
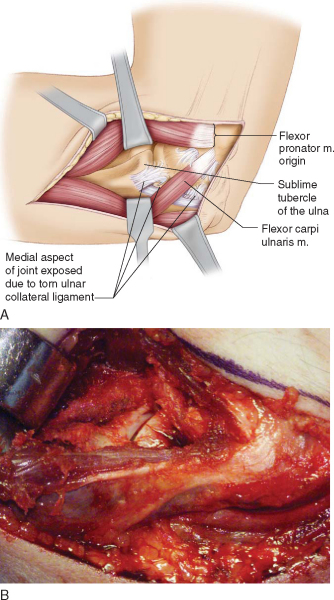
). We prefer the muscle-splitting approach[14] for exposure of the UCL. A fascial raphe can usually be identified in the flexor-pronator mass at the junction of the anterior two thirds and posterior third of the muscle group. This raphe represents an internervous plane between the median nerve–innervated palmaris longus and deeper flexor digitorum superficialis and the ulnar nerve–innervated flexor carpi ulnaris. The fascia is split through the raphe from the medial epicondyle to a point approximately 1 cm distal to the sublime tubercle. The sublime tubercle can be palpated deep under the flexor mass. More distal dissection risks denervation of the surrounding musculature from crossing nerve branches. The muscle is then bluntly divided down to the level of the underlying UCL (
Fig. 37-3
). Care is taken during the split and division of the muscle because the ulnar nerve lies just posterior to the approach. A blunt self-retainer is used to retract the musculature, and a small periosteal elevator can be used to clean any remaining muscle fibers from the UCL. Application of a valgus stress should reveal excessive medial joint line opening consistent with UCL insufficiency. After external inspection of the ligament, a longitudinal incision is made in the direction of its fibers to assess undersurface tears and degeneration. As much of the native, intact UCL is preserved as possible. Also through this incision, the joint can be inspected for loose bodies and other intraarticular disease.
| Surgical Steps | ||||||||||||||||||
|
|
|
|
|
Figure 37-2 |
|
|
|
|
Figure 37-3 |
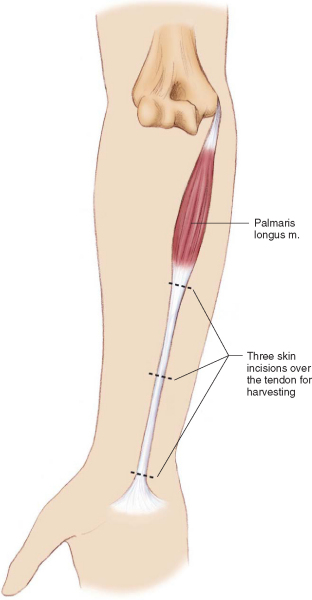
If it is present, the ipsilateral palmaris longus tendon is harvested as the preferred graft (
Fig. 37-4
). The tendon is identified at the level of the proximal wrist flexion crease as it inserts into the palmar fascia. A small 1- to 2-cm transverse incision is made directly over the tendon. A small hemostat is used to dissect the tendon, with care taken to protect the underlying median nerve. Tension is applied to the tendon with the hemostat, and two additional transverse incisions are made proximally over the tendon and myotendinous junction approximately 8 cm apart. The tendon graft is then incised proximally and distally and delivered out of the wound (
Fig. 37-5
). Ideally, the graft length is 12 to 15 cm. The graft is cleaned of muscle, and a running whipstitch is placed in both ends of the graft with No. 2 FiberWire (Arthrex, Inc., Naples, Fla).
|
|
|
|
Figure 37-4 |
|
|
|
|
Figure 37-5 |
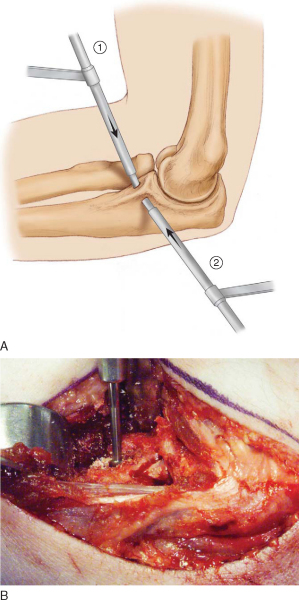
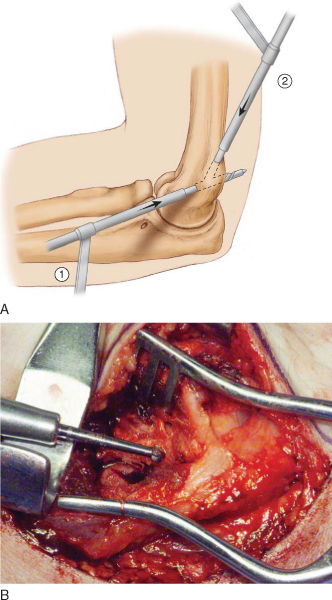
3. Preparation of Ulnar Tunnels
With careful subperiosteal dissection, the medial aspect of the ulna distal to the sublime tubercle is exposed in preparation for the ulnar bone tunnels. By use of a 3.2-mm drill bit, two converging tunnels are made at right angles to each other anterior and posterior to the sublime tubercle, with care taken to maintain a good bone bridge of approximately 6 to 8 mm (
Fig. 37-6
). A small curved curet is used to clean the tunnel entrance of bone debris and to connect the tunnels.
|
|
|
|
Figure 37-6 |
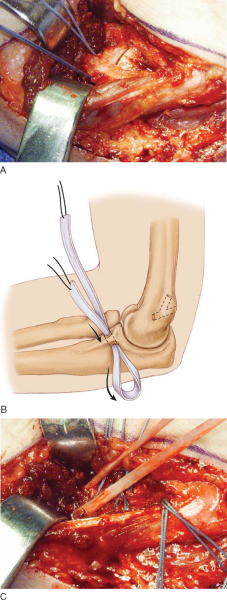
4. Preparation of Humeral Tunnels
The insertion of the UCL is traced back to its origin on the medial epicondyle. The insertion is located on the anteroinferior surface of the epicondyle, usually in the middle two thirds of the epicondyle in the coronal plane.[9] A 3.2-mm drill bit is used to make a bone tunnel starting at the insertion and through the back of the medial epicondyle (
Fig. 37-7
). The ulnar nerve is carefully protected during this portion to avoid iatrogenic injury from the drill. Next, a minimal release is performed to allow safe retraction of the nerve. The proximal portion of the epicondyle anterior to the medial intermuscular septum is then carefully exposed subperiostally. A 3.2-mm drill bit is used to make a second bone tunnel starting anterior to the medial intermuscular septum and aiming distally to approximately the middle portion of the previously drilled tunnel. Care is taken to maintain an adequate bone bridge of at least 5 mm between the tunnels and the trochlear articular surface. A small curved curet is then used to clean the tunnels of bone debris.
|
|
|
|
Figure 37-7 |
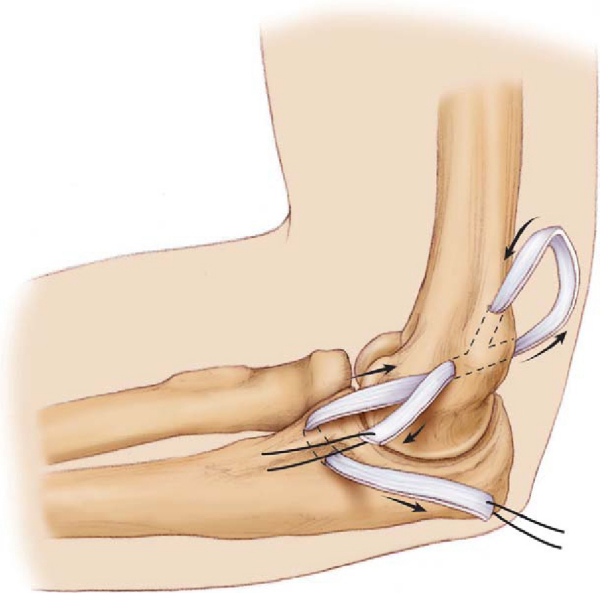
5. Passage and Tensioning of the Graft
The prepared graft is then passed from anterior to posterior in the ulnar tunnel with the help of a Hewson suture passer (
Fig. 37-8
). The graft is passed through the humeral tunnels in a figure-of-eight fashion with a three-ply reconstruction (
Fig. 37-9
). The elbow joint is then reduced with the application of a varus stress, and the elbow is flexed to approximately 45 degrees as tension is applied across the graft. The graft is then sutured to itself with No. 2 FiberWire in a mattress fashion (
Fig. 37-10
). The native UCL is also sutured to itself and to the graft to reinforce the reconstruction.
|
|
|
|
Figure 37-8 |
|
|
|
|
Figure 37-10 |
The tourniquet is deflated, and meticulous hemostasis is obtained to prevent a postoperative hematoma. The wound is thoroughly irrigated before closure. The flexor-pronator mass is closed with No. 0 Vicryl suture, followed by routine skin closure. A sterile dressing is applied, and the arm is splinted in approximately 90 degrees of flexion with the forearm in neutral rotation.
One week after surgery, the sutures are removed and a hinged elbow brace is applied.
A specific rehabilitation protocol is crucial to successful return to athletic competition.
| • | Ulnar nerve irritation is the most common postoperative complication with a reported incidence of up to 21%.[7] | |
| • | Trauma to the medial antebrachial cutaneous nerve | |
| • | Hematoma | |
| • | Superficial or deep infection | |
| • | Fracture of the humeral or ulnar tunnels from an insufficient bone bridge |
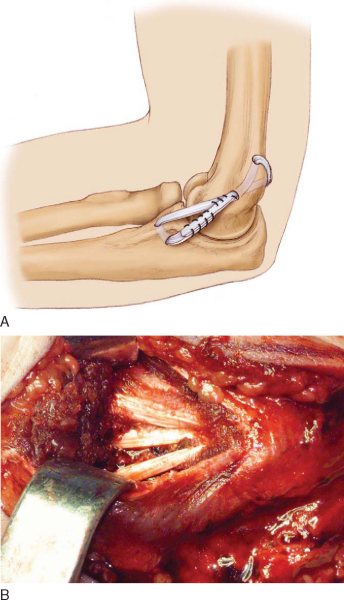
The results of UCL reconstruction are best measured by the athlete’s return to sport. Successful return to elite throwing is a far more stringent outcome measure than is objective testing of valgus laxity.[13] Since the original description of the technique by Jobe, there have been several modifications to the technique to attempt to decrease morbidity and postoperative complications while allowing the athlete to safely return to sport (
Table 37-1
). Current techniques allow the competitive throwing athlete to return successfully to the same or higher level of sport approximately 79% to 92% of the time. Successful return also depends on completion of a dedicated prolonged rehabilitation protocol. Continued advances in technology, such as interference screw fixation[1] and hybrid techniques, may allow an even greater chance of success in the future, but clinical validation is pending.
| Author | Technique | Results |
|---|---|---|
| Jobe et al[8] (1986) | Original “Tommy John” method | 10/16 (63%) throwing athletes returned to same level |
| Flexor-pronator mass detached | ||
| Figure-of-eight graft | ||
| Submuscular ulnar nerve transposition | ||
| Conway et al[7] (1992) | Original method | 38/56 (68%) athletes returned to same level |
| Flexor-pronator mass detached | 12/56 (21%) postoperative ulnar nerve irritability | |
| Figure-of-eight graft | Reconstruction better than repair | |
| Submuscular ulnar nerve transposition | ||
| Azar et al[3] (2000) | Andrews modification of original Jobe technique | 78 UCL reconstructions; 41% professional |
| Flexor mass divided with partial detachment of flexor carpi ulnaris | 79% of athletes returned to same or higher level | |
| Figure-of-eight graft | Average return: 9.8 months | |
| Subcutaneous ulnar nerve transposition | ||
| Thompson et al[15] (2001) | Modified Jobe technique | 83 UCL reconstructions; 65% professional |
| Muscle-splitting approach | 100% of athletes returned to sport | |
| Figure-of-eight graft | 82% returned to same or higher level | |
| No ulnar nerve transposition | 5% transient ulnar nerve irritability | |
| Rohrbough et al[13] (2002) | Docking procedure modification | 36 UCL reconstructions |
| Routine arthroscopic assessment | 33/36 (92%) returned to same or higher level | |
| Muscle-splitting approach | Average 3.3-year followup | |
| Two tendon ends of graft docked into single humeral tunnel | ||
| Selective subcutaneous ulnar nerve transposition | ||
| Cain et al[5] (2002) | Andrews modification of original Jobe technique | 342 UCL reconstructions with minimum 2-year followup |
| 96% baseball players; 45% professional, 45% collegiate, 10% high-school | ||
| 83% returned to same or higher level | ||
| Average return: 11.4 months | ||
| Paletta and Wright[11] (2002) | Docking procedure | 25 UCL reconstructions in professional or collegiate throwing athletes; 2-year minimum followup |
| 4-strand technique reconstruction | 23/25 (92%) returned to same or higher level | |
| Average return: 12.5 months |
1.
Ahmad CS, Lee TQ, ElAttrache NS: Biomechanical evaluation of a new ulnar collateral ligament reconstruction technique with interference screw fixation.
Am J Sports Med 2003; 31:332-337.
2.
Andrews JR, Whiteside JA, Buettner CM: Clinical evaluation of the elbow in throwers.
Oper Tech Sports Med 1996; 4:77-83.
3.
Azar FM, Andrews JR, Wilk KE, Groh D: Operative treatment of ulnar collateral ligament injuries of the elbow in athletes.
Am J Sports Med 2000; 28:16-23.
4.
Breazeale NM, Altchek DW: Ulnar collateral ligament injuries.
In: Baker CL, Plancher KD, ed. Operative Treatment of Elbow Injuries,
New York: Springer-Verlag; 2002:89-100.
5.
Cain EL, Andrews JR, Dugas JR, et al: Outcome of ulnar collateral ligament reconstruction of the elbow: minimum two-year followup.
Transactions of the annual meeting of the American Orthopaedic Society for Sports Medicine 2002;173.
6.
Callaway GH, Field LD, Deng XH, et al: Biomechanical evaluation of the medial collateral ligament of the elbow.
J Bone Joint Surg Am 1997; 79:1223-1231.
7.
Conway JE, Jobe FW, Glousman RE, Pink M: Medial instability of the elbow in throwing athletes: treatment by repair or reconstruction of the ulnar collateral ligament.
J Bone Joint Surg Am 1992; 74:67-83.
8.
Jobe FW, Stark H, Lombardo SJ: Reconstruction of the ulnar collateral ligament in athletes.
J Bone Joint Surg Am 1986; 68:1158-1163.
9.
O’Driscoll SW, Jaloszynski R, Morrey BF, An KN: Origin of the medial ulnar collateral ligament.
J Hand Surg Am 1992; 17:164-168.
10.
O’Driscoll SW, Lawton RL, Smith AM: The “moving valgus stress test” for medial collateral ligament tears of the elbow.
Am J Sports Med 2005; 33:231-239.
11.
Paletta Jr GA, Wright RW: The docking procedure of elbow MCL reconstruction: two year follow up in elite throwers.
Transactions of the annual meeting of the American Orthopaedic Society for Sports Medicine 2002;172.
12.
Rettig AC, Sherrill C, Snead DS, et al: Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes.
Am J Sports Med 2001; 29:15-17.
13.
Rohrbough JT, Altchek DW, Hyman J, et al: Medial collateral ligament reconstruction of the elbow using the docking technique.
Am J Sports Med 2002; 30:541-548.
14.
Smith GR, Altchek DW, Pagnani MJ, Keeley JR: A muscle splitting approach to the ulnar collateral ligament of the elbow: neuroanatomy and operative technique.
Am J Sports Med 1996; 24:575-580.
15.
Thompson WH, Jobe FW, Yocum LA, Pink M: Ulnar collateral ligament reconstruction in athletes: muscle splitting approach without transposition of the ulnar nerve.
J Shoulder Elbow Surg 2001; 10:152-157.
16.
Veltri DM, O’Brien SJ, Field LD, et al: The milking maneuver: a new test to evaluate the MCL of the elbow in the throwing athlete.
J Shoulder Elbow Surg 1995; 4:S10.22.