Ankle Injuries
consists of an inversion injury of the foot with some degree of plantar
flexion. Overall, the period of recovery is relatively short and
uneventful. A more relevant injury with a completely different period
of recovery is the injury while the foot is in eversion, the so-called “high ankle sprain.” It accounts for 1% to 15% of the total ankle sprains (1).
Therefore, the first issue when approaching a patient with an ankle
sprain should be directed to identifying the mechanism of injury. Given
the frequency of fractures, it is often recommended to obtain the
history and do a brief exam using only palpation, and, if suspicion for
a fracture is present, then obtain x-rays prior to extensive physical
examination techniques.
-
Acute presentation
-
Inversion injuries.
With inversion ligamentous injuries, there is tearing of the lateral
ligaments in order from front to back. Thus, the anterior talofibular
ligament (ATFL) is the most commonly injured ligament followed by the
calcaneofibular ligament (CFL) and, in very rare instances, the
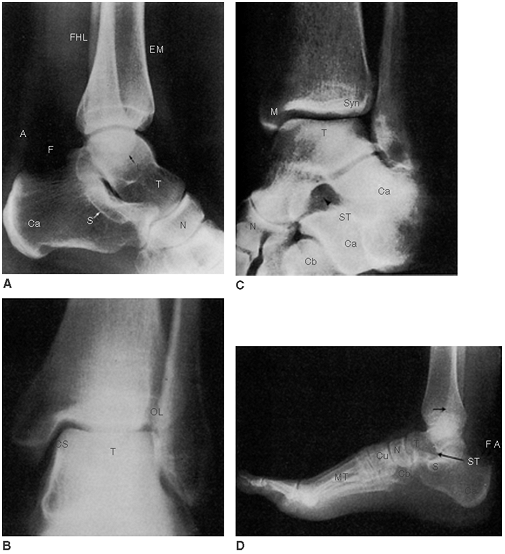
posterior talofibular ligament (PTFL).Fig. 26-1
shows the anatomic location of the ligaments. Fractures can occur with
simple inversion injuries. The most common sites are the distal fibula
and the base of the fifth metatarsal.-
Examination.
Palpation is the key to examining ankle injuries. Included in this is
palpation of the bones around the ankle. Special attention should be
drawn to the distal fibula, distal tibia, and the base of the fifth
metatarsal as per the Ottawa criteria (Table 26-1).
In more severe fractures, also palpate the proximal fibula as this can
be broken (Maissoneuve fracture). All ankle ligaments should be
palpated looking for tenderness. In the acute setting, pain is quite
limiting; therefore, it is very difficult to stress the ankle joint or
obtain ankle stress radiographs to confirm which ligaments are intact.
In the absence of fracture, soft tissue swelling and pain will dictate
the treatment. -
Radiographic imaging. The need for x-rays can be guided by consideration of the Ottawa ankle rules (Table 26-1).
It is important to note that the rules do not apply to a pediatric
population with open growth plates (to be safe, it is recommended to
x-ray those under age 18). Although not specifically listed, we
recommend strong consideration to obtain x-rays on people over the age
of 50, especially women over the age of 50 due to lower bone mass and
subsequent higher fracture rates. X-rays should include anteroposterior
(AP), lateral, and mortise views. -
Treatment. If there is no medial tenderness, the ankle joint should be considered a stable joint.
The traditional principles of rest, immobilization, compression,
elevation, and icing should be applied followed by a functional return
to activities while protected with any of the commercially available
ankle braces until the pain allows proper muscle contraction of the
dynamic stabilizers of the ankle (peroneal and deep compartment muscles
of the lower leg). In rare occasions, due to pain with weight bearing,
the patient will have to be protected for 6 to 8 weeks.If there is medial or anterior capsule tenderness, the possibility of developing talar instability is higher, and closer examination of the ankle
P.372P.373
mortise for talar dome injuries and symmetry is warranted. If
suspected, the period of immobilization in a walking cast or boot
should be longer, for 6 to 8 weeks until the medial and anterior
tenderness disappear. At that time it can be treated as a stable injury
depending on the remaining discomfort within the ankle joint.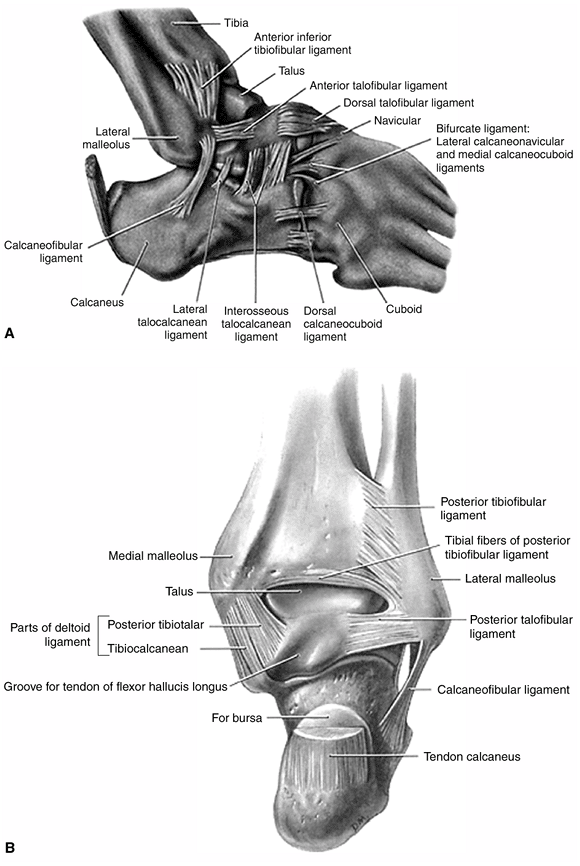 Figure 26-1. Anatomic description of the most significant ligaments and bones of the ankle and midfoot area.TABLE 26-1 Ottawa Criteria to Perform Radiographic Examination
Figure 26-1. Anatomic description of the most significant ligaments and bones of the ankle and midfoot area.TABLE 26-1 Ottawa Criteria to Perform Radiographic ExaminationAnkle injuries - Pain along the posterior margin of the most distal 6 cm of the fibula
- Pain along the posterior margin of the medial malleolus
- Unable to bear weight immediately after the injury or to take four steps in the Emergency Department (even with a limp)
- Age less than 18
Midfoot injuries - Pain along the base of the fifth metatarsal
- Pain along the navicular
- Unable to bear weight immediately after the injury or to take four steps in the Emergency Department (even with a limp)
- Age less than 18
-
-
Eversion injuries
-
Examination.
The exam will show some tenderness along the most anterior and distal
aspect of the syndesmosis of the ankle. Some tenderness along the
lateral ligament complex may be present although to a much lesser
degree than with true inversion ankle sprains. Any degree of external
rotation, which stresses the ankle mortise, will increase or reproduce
the pain. The external rotation can be applied directly by the examiner
holding the lower leg with one hand and torquing on the foot with the
opposite hand while keeping the ankle in a neutral position, so the
talus is locked in the ankle mortise. If a fracture has been ruled out,
a “squeeze test” (using both hands to push the mid-fibula and tibia
together, noting pain distal to the area of compression) can be
performed to assess syndesmotic injuries. If the patient can tolerate
weight bearing, a more sensitive test for a syndesmosis injury consists
of standing on the injured leg and applying an external rotation force
to the ankle with an internal turn of the pelvis with the knee fully
extended. If the patient can stand and perform some degree of external
rotation, the suspicion for an unstable mortise should be low. If there
is any tenderness in the proximal lower leg, full length tibia and
fibula radiographs should be obtained to rule out a proximal fibula
fracture (Maissonneuve fracture) or an unstable syndesmosis. This
projection is taken as an AP view with 30° of internal rotation (when
both malleolus are equidistant from the x-ray beam). A noncompetent
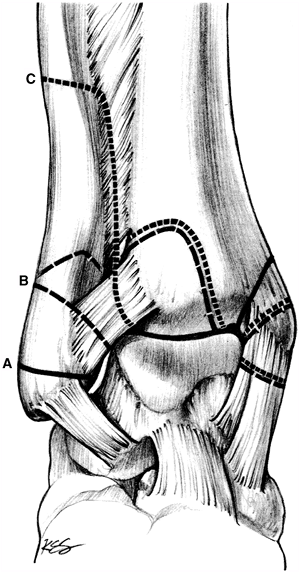
syndesmosis is defined as the one that presents on an AP view of the
ankle more than 6 mm of clear space between the tibia and the fibula
measured at 10 mm proximal from the joint line (2) (Fig. 26-2).
When it comes to x-ray measurements, the clear space in between the
tibia and the fibula has been shown to be more reliable and less
subjective to rotation than the overlap in between the tibia and fibula
(<5 mm). If the syndesmosis appears intact on a static radiograph,
but suspicion for syndesmotic injury remains high, consider stress
views of the ankle (ideally under fluoroscopic dynamic examination)
while applying external rotation to the foot. The best projection to
assess the stability of the syndesmosis is the mortise view. The
patient will have to be either sedated or injected with local
anesthetic along the syndesmosis prior to its
P.374
evaluation.
A total of 5 to 15 cc of lidocaine 1% with epinephrine should suffice
to anesthetize the syndesmosis. The injection is performed using a 25-
or 22-gauge needle along the anterior aspect of the syndesmosis,
starting immediately proximal to the joint line level and always
“walking” along the lateral cortex of the tibia from distal to
proximal. Special attention has to be paid to not angle the needle too
posteriorly, never posterior to the plane of the fibula, to avoid
damage into vital structures of the posterior compartment of the leg.![]() Figure 26-2. Radiographic appearance of the most common bony landmarks of the ankle and foot. A: Medial view of ankle region. B: Anterior view of ankle. C: Mortise view of ankle region. D:
Figure 26-2. Radiographic appearance of the most common bony landmarks of the ankle and foot. A: Medial view of ankle region. B: Anterior view of ankle. C: Mortise view of ankle region. D:
Lateral view of foot. M, medial malleolus; L, lateral malleolus; T,
talus; Ca, calcaneus; S, sustentaculum tali; N, navicular; Cu,
cuneiforms; Cb, cuboid; Mt, metatarsal; ST, sinus tarsi; A Achilles
tendon; F, fat; arrowhead, superimposed tibia and fibula; Syn,
Syndesmosis; FHL, flexor hallucis longus; EM, extensor muscles; CS,
tibiofibular clear space; OL, tibiofibular overlap. -
Treatment. If
P.375
the syndesmosis is stable
or in the absence of fractures, the patient should be immobilized in a
walking cast or boot for 6 to 8 weeks followed by a functional return
to activities of daily living and sports. If the syndesmosis is unstable
or in the presence of a proximal fibula fracture, the patient will
require fixation of the syndesmosis with screws followed by
immobilization for 6 to 8 weeks. Weight bearing should be started prior
to removal of the screws and always after warning the patient about the
possibility of screw breakage. A residual wide syndesmosis because of a
misdiagnosis or improper treatment is a devastating sequelae that will
lead to a very severe post-traumatic osteoarthritis of the ankle joint
within 1 to 2 years.
-
-
-
Subacute-chronic presentation
-
Inversion injuries.
The patient presents with some residual discomfort in areas where there
may still be some healing taking place or where an injury has been
missed. The physician has to rule out any residual instability,
reported to be present in 20% to 40% of ankle sprains, or a chondral
injury of the talus, present in 6.5% of ankle sprains (3).
If the patient continues to report instability after a period of
physical therapy, then one should consider stress views of the ankle.
If the patient still presents enough pain that the ankle will be
protected by contraction of the surrounding musculature, therefore
making the exam for stability unreliable, the patient should have some
intravenous sedation or local anesthetic injected into the ankle. A
total of 5 cc of lidocaine 2% with epinephrine should be enough to
anesthetize the ankle joint. The injection is performed with a 25- or
22-gauge needle along the most medial border of the ankle joint
immediately distal to the medial shoulder of the tibial plafond and
medial to the anterior tibialis tendon. The needle has to be angled at
45° from the coronal plane. The ankle can also be approached through
the lateral aspect over the “soft spot,”
which is defined as the junction of the tibia and fibula at the level
of the joint line. However, the chances of damaging the dorsal
cutaneous branch from the superficial peroneal nerve are relatively
high. The best chance to identify the nerve branch is with gentle
palpation of the skin, looking for a cord-like structure when the
fourth toe is forced into plantar flexion.The stress views are obtained with a lateral radiograph
while the foot is pulled forward (an anterior drawer test) in slight
plantar flexion. The most commonly injured ligament, the ATFL, is
stressed during this maneuver. A 10-mm difference of anterior
displacement between the stress view and the resting view or a 3-mm
difference of anterior displacement compared to the stressed opposite
side is indicative of ankle instability. Treatment options for chronic
instability include a formal physiotherapy program and, if that fails,
the next reasonable step is a surgical repair/reconstruction of the
lateral ligament complex of the ankle. In the absence of an obvious
chondral injury of the talus on plain x-rays, a magnetic resonance
imaging (MRI) scan is necessary to rule it out. A symptomatic chondral
injury most likely will require some surgical treatment (i.e.,
arthroscopic debridement +/- subchondral drilling) to improve the
symptoms. -
Eversion injuries.
The most common reason to present with residual pain after a
syndesmosis sprain will be some degree of remaining instability. A
careful and detailed evaluation of the patient has to be performed as
surgical fixation of the syndesmosis will be the most likely treatment
recommendation.
-
-
Classification.
Ankle fractures are intraarticular injuries, and accurate reduction as
well as maintenance of the reduction is required for a satisfactory
long-term result. To achieve reduction by closed manipulation, it is
necessary to know the direction of the forces producing the fractures.
It must be emphasized that fractures about the ankle usually are not
isolated injuries but have significant associated ligamentous ruptures.
Ankle fractures may be classified by the Lauge-Hansen scheme (Fig. 26-3).
This classification is useful because of the method used for its
description. The first term makes reference to the position of the foot
at the time of injury and the second term to the direction of the force
applied to produce the fracture. That information is extremely valuable
in planning closed reduction maneuvers.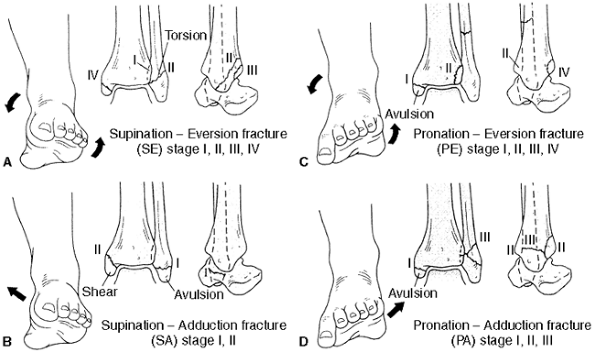 Figure 26-3. The Lauge-Hansen classification of ankle fractures. A:
Figure 26-3. The Lauge-Hansen classification of ankle fractures. A:
The supination-eversion fracture. Stage I: The avulsion of the anterior
talofibular ligament from the tibia or simple rupture of the ligament.
Stage II: The classic oblique fracture of the distal fibula, beginning
anteriorly at the joint line and extending obliquely and posteriorly
toward the shaft of the bone. Stage III: Avulsion or rupture of the
posterior tibiofibular ligament. Stage IV: Avulsion fracture of the
medial malleolus. B: The
supination-adduction fracture. Stage I: Avulsion of the tip of the
lateral malleolus or rupture of the associated ligaments. Stage II:
Vertical fracture of the medial malleolus, usually beginning at the
plafond. C: The pronation-eversion
fracture. Stage I: Avulsion of the medial malleolus or ruptured deltoid
ligament. Stage II: Rupture or avulsion of the anterior tibiofibular
ligament. Stage III: A high short oblique fracture of the fibula. Stage
IV: A posterior lip fracture of the tibia. D:
The pronation-abduction fracture. Stage I: Avulsion of the medial
malleolus or ruptured deltoid ligament. Stage II: Rupture or avulsion
of the syndesmotic ligaments. Stage III: A short, oblique fracture of
the distal fibula at about the level of the ankle joint. (From Weber
MJ. Ankle fractures and dislocations. In: Chapman MW, Madison M, eds. Operative orthopaedics, 2nd ed. Philadelphia, PA: JB Lippincott, 1993:731–745, with permission).P.376The Danis-Weber or AO Association of Osteosynthesis classification system concentrates on the pattern of the fibular fracture (Fig. 26-4).
The type A fracture is distal to the level of the syndesmosis and
frequently transverse, the type B fracture is a spiral oblique fracture
at the level of the syndesmosis, and the type C fracture is proximal to
the syndesmosis level. -
Examination. The ankle has to be palpated for tender areas. The Ottawa Criteria (Table 26-1)
for evaluation and management of ankle injuries have been proven to be
a practical way to approach these injuries. Recently, it has been shown
to have a sensitivity of no less than 99.6% for detecting fractures (4).
However, in spite of these reports, it does not seem to be used
routinely for fear of missing ankle fractures and the potential legal
consequences associated. The lack of soft tissue swelling in some
situations may be misleading, especially in the elderly population. -
Radiographs.
AP, lateral, and oblique (the mortise view) films are essential for
evaluating any ankle injury. A clearer delineation of the medial
malleolar fracture may be achieved by an additional view obtained with
the foot in 45 degrees of internal rotation. A lateral radiograph
obtained at 50 degrees of external rotation is the best way to
visualize the posterior malleolus (5). -
Treatment. The main feature that determines the treatment plan is if the ankle fracture is a stable or unstable injury.
-
Stable injuries.
A stable ankle fracture is defined as the one that presents no widening
of the medial or lateral mortise joint space. A fracture distal to the
P.377
syndesmosis
with a ruptured deltoid ligament, which is suspected if there is
significant medial tenderness, will represent an unstable ankle
fracture with a stable syndesmosis. Therefore, the definition of
stability should be an ankle joint where the fracture is distal to the
syndesmosis with no injury to the medial stabilizers and consequently
with no widening of the medial mortise. The immediate treatment
consists of elevation, reduction of the fracture, and immobilization as
soon as possible to reduce soft tissue swelling. If the fracture is
merely a small avulsion off of the distal tip of the fibula without any
involvement of the mortise, then treatment can be similar to that of
the associated ligament sprain. For stable fractures that are larger
and with some degree of displacement, a closed reduction maneuver can
be attempted. For most oblique fractures of the fibula, the reduction
is via plantar flexion and internal rotation. This can often be
achieved by lifting the patient’s limb (with the patient in the supine
position) by the great toe. Immobilize the patient’s leg in a
P.378
short
leg splint in this position. For long-term treatment (more than 4–6
weeks), the ankle must be maintained in a neutral position (90° from
the long axis of the lower leg) to prevent any Achilles contracture and
a longer than expected recovery time. The patient should be instructed
in toe-touch weight bearing until there are radiographic signs of
callus and lack of tenderness to pressure (3–4 weeks) over the lateral
malleolus. Further protect the injury in a short leg cast with the foot
in neutral position for another 3 to 4 weeks. Stable ankle fractures
have equivalent results whether treated operatively or nonoperatively (6). Consequently, we recommend an attempt at nonoperative treatment whenever possible.![]() Figure 26-4. Diagrammatic representation of the Danis-Weber classification system. A: Transverse fracture of the distal malleolus. B: Spiral fracture at the level of the mortise. C: Fractures above the mortise with disruption of the syndesmosis. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993: 340.)
Figure 26-4. Diagrammatic representation of the Danis-Weber classification system. A: Transverse fracture of the distal malleolus. B: Spiral fracture at the level of the mortise. C: Fractures above the mortise with disruption of the syndesmosis. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993: 340.) -
Unstable injuries
-
These fractures should be reduced and internally fixed as an urgent procedure if the patient is seen before significant swelling is apparent (7,8).
Preoperative planning is essential to minimize soft-tissue stripping
and maximize fixation. Patients with open fractures should be managed
with wound debridement and internal fixation; the results are generally
equivalent to those for closed fractures (9). Significant improvement can be expected to continue 6 months after the fracture occurred (10,11).-
Medial malleolar fragments
should be reattached with screws for larger fragments and with
Kirschner wires with supplemental tension band wires for smaller
fragments. With screw fixation, a length of 35 to 40 mm is appropriate
so that the metaphyseal bone is engaged and the medullary canal is
avoided with loss of screw purchase. The rate of nonunion with surgical
treatment is reported to be as low as 1% compared with 15% with
conservative treatment (12). -
Posterior malleolar fragments
are stabilized with screw fixation if they involve more than one fourth
of the articular surface. Generally these fragments are reduced by
reduction of the associated distal fibula fracture. The lag screw
placement can be done from the anterior to posterior direction
(frequently percutaneously). Formal open reduction, if required, must
be done before definitive fixation of the lateral malleolus, which may
limit the surgical exposure; the incision must be well posterior to the
fibula. -
Lateral malleolar fractures
below the ankle joint (Danis-Weber A) may be reduced as medial
malleolar fractures. If possible, an attempt should first be made to
reduce and fix the fracture with a lag screw. Fractures with disruption
of both anterior and posterior tibio-fibular ligaments can be held with
a “position” (or syndesmosis) screw inserted parallel to the plafond
into the tibia. This screw is generally placed after anatomic reduction
of a type B or C fibula fracture, with the foot fully dorsiflexed (to
prevent narrowing of the ankle mortise), through the plate, and after
gaining purchase on one or both of the tibial cortices (see iv
below). Spiral or oblique fractures with the tibio-fibular ligament
intact may be reapproximated by oblique lag screws and/or with a small,
one-third tubular plate. Prophylactic antibiotics should be utilized (13).
These plates could be placed on the posterior aspect of the fibula to
prevent irritation from the plate when in the lateral aspect, a more
subcutaneous position (14). More recently, success has been achieved with bioabsorbable implants (15,16). Repair to the deltoid ligament avulsion is generally not necessary (17).
Postoperatively, the leg may be treated in a short-leg compression
dressing with a plaster or fiberglass splint to control the position of
the foot. As soon as the swelling is controlled, at 5 to 7 days, a
removable splint can be used and early active motion started. The
patient should remain partial weight bearing for 4 to 6 weeks. If the
patient is unable to co-operate with the early, active range-of-motion
protocol, then a short-leg cast is applied for 4 to 6 weeks (18,19). Weight bearing and strengthening exercises are initiated following this period. -
iv. If the tibio-fibular syndesmosis is widened,
it is because the distal interosseous membrane is torn. This injury can
be associated with a proximal fibula fracture (the Maissoneuve
fracture). Authorities who report the best results treat this injury
with a suture repair of a ligamentous rupture when feasible and with
one or two position (or syndesmosis) screws placed parallel to the
plafond. Some authors recommend the use of 4.5-mm cortical screws; we
favor the use of one or two 3.5-mm screws with purchase through four
cortices (exit the tibia slightly to allow removal if they break). Care
must be taken to maintain the normal fibular length and, by keeping the
foot in neutral position, the proper mortise width. Some authorities
recommend delaying full weight bearing until the syndesmosis screws are
removed. However, the authors have seen many more problems following
early removal of the syndesmosis screws, and, currently, it is
recommended to leave them in as weight bearing is progressed. The
patient should be advised that the screws may break.
P.379 -
-
When swelling is already significant,
any gross malalignment should be corrected. Then the leg should be
placed in a compression dressing with splints and elevated until the
swelling has receded sufficiently for a safe open reduction. In order
to avoid wound healing complications, patients should be seen and
surgically treated as soon after the injury as possible (7). The operative complication rates are four times higher for diabetic (20,21) and obese patients managed operatively (22).
-
-
-
Complications
-
Incomplete reduction
is associated with a higher incidence of ankle joint symptoms than are
seen when anatomic restitution is achieved. This situation can be
improved by osteotomy and internal fixation even years after the
fracture occurs (23). The results after restoring the original anatomy overall are worse than those with early anatomic reduction (12). -
Nonunion,
although rare, can occur and is usually symptomatic. On the medial
side, it may be associated with interposition of the posterior tibial
tendon. Nonunion of either malleolus should be managed with internal
fixation and bone grafting. Deep infection as the cause for the
non-union has to always be ruled out with intraoperative cultures,
especially after prior open reduction and internal fixation.
-
generally high-energy injuries from axial loads. They occur as a result
of high speed motor vehicle accidents or falls from a height (24).
-
Diagnosis is
confirmed by radiographs, as for ankle fractures. The history of
high-energy trauma or fall from a significant height should prompt a
thorough examination of the heel, foot, and ankle paying special
attention to swelling and tenderness. If the plain radiographs do not
sufficiently document the fracture pattern, a computed tomographic (CT)
scan is indicated to better delineate the size and location of the bony
fragments. -
Treatment.
Fractures of the joint surface with more than 2 to 3 mm of
displacement, either gapping or impaction, are generally managed by
reduction, fixation, and in some occasions with bone grafting.
Significant swelling of the soft tissues occurs very rapidly with this
type of injuries; therefore, operative management must be emergent or
otherwise delayed for several days or weeks until the swelling
subsides. Plating of an associated fibula fracture, application of an
external fixator across the ankle joint, or a calcaneal pin traction on
a Bohler frame are valid options in the interim to achieve indirect
reduction of the joint fragments and expedite the resolution of the
soft tissue swelling. All those options limit the amount of soft tissue
stripping required in subsequent surgeries which will help to achieve
bony consolidation and to decrease the potential complications. Acute
compartment syndromes are not uncommon with this type of fracture. If
open fasciotomy is performed, then the fibula should be plated to
restore some stability to the fracture. Because of the high incidence
of wound complications and deep infections,
P.380
there
is a trend toward limited fracture exposure, indirect reduction and
fixation of the joint surface with lag screws, and complete definitive
treatment with an external fixator or percutaneous plates. Bone
grafting may not be required if the fracture is not exposed, but it
should be carried out if there is any doubt. -
Complications. Deep infection may require multiple debridements, hardware removal, and muscle-flap (often free) coverage (24).
If the problem is identified early, then the hardware can be generally
left in place. Pilon fractures are associated with a very high rate of
complications, and their management should be left to a specialist
familiar with this type of injury. Frequently, the long-term result is
a stiff, painful, and chronically swollen ankle that at some point may
require an ankle arthrodesis to improve the function and symptoms of
the patient.
-
The history
associated with an Achilles tendon rupture is often diagnostic. The
patient profile is a middle-aged individual occasionally involved in
recreational sports, also known as “the weekend warrior.” Patients with
a different profile are worth evaluating for risk factors (i.e.,
steroid use) because this pathology is fairly unusual in a young
healthy individual. It cannot be emphasized enough that a healthy
tendon will not rupture during exercise. However, unhealthy tendons do
not necessarily cause symptoms. Usually, the patient was running or
jumping when a sudden severe pain was felt behind the ankle, almost as
if it had been struck by something. Patients will describe the episode
as being “…kicked by somebody, I turned around, and there was nobody
there…” or being hit by a rock or the opponent’s racquet. Afterwards,
the patient may be able to walk but usually with a significant
difficulty. -
Examination
is most easily accomplished with the patient prone. By inspection and
palpation, the defect in the Achilles tendon can be documented.
Squeezing the calf in this position with an intact Achilles tendon
causes passive plantar flexion to occur; this response is absent with
tendon rupture (Thompson’s test). Even if the plantar flexion is
present but decreased, the diagnosis of Achilles tendon rupture can be
made. Do not be misled by the patient’s ability to plantar-flex the
ankle actively because this can be done with the muscles from the deep
posterior compartment of the lower leg. Neurovascular exam is normally
intact. In case of doubt, depending on the expertise of the radiology
department, an ultrasound will be definitive to demonstrate a gap
within the tendon fibers. If ultrasound is not available, an MRI will
be diagnostic. The treatment guidelines are the same for either a
partial or a complete rupture and are more dependent on the patient’s
profile. -
Treatment
-
Patients with low functional demands may undergo nonoperative treatment.
The foot is held in equinus for 8 weeks in a short-leg cast. It is
extremely important not to force the plantar flexion excessively as the
posterior aspect of the most distal part of the lower leg may develop
skin necrosis from lack of blood supply. This can be easily
demonstrated by the blanching of the skin that takes place with forced
plantar flexion. The acute swelling also decreases the tolerance of the
skin to plantar flexion. The position chosen for immobilization cannot
compromise the posterior skin, and normal color has to be seen along
the posterior aspect of the leg. Ambulation with crutches using an
elevated heel on the shoe for 8 to 12 weeks then follows. Finally,
rehabilitation exercises are begun to increase strength and range of
motion. -
Operative treatment
is often recommended, especially for the young, competitive athlete.
The advantages of open treatment are that the proper strength-length
relationship of the musculotendinous unit is re-established, the
internal repair probably adds extra strength to the ruptured tendon,
and immobilization can be limited. The risk of re-rupture of the tendon
is lower with operative management (25). The
incision should be made to one side of the tendon (not directly
posteriorly) and should not extend distally into the flexor creases
posterior to the ankle; this helps minimize adhesions of the tendon to
the skin. A careful repair of the tendon sheath also limits these
adhesions. The actual type of tendon repair is left to the discretion
of the surgeon; numerous
P.381
materials
and patterns of suture repair have been discussed. The plantaris tendon
or the flexor hallucis longus tendon transfer may be used to augment
the repair. Postoperatively, the ankle is kept in a slight equinus
position with a short-leg cast or boot for 8 weeks. Ambulation and
physical therapy are then allowed as tolerated to increase strength and
range of motion.
-
-
Complications.
The rate of complications with either treatment, conservative or
surgical, is similar. The difference is the type of complications which
occur. With conservative treatment, the most common complications
include re-rupture and weakness of the Achilles complex with plantar
flexion. The weakness is more noticeable during the practice of sports
and very rarely during activities of daily living (ADLs). With surgical
treatment, the complications are related to skin dehiscence/necrosis,
neurologic damage, and infection. There is no good data to recommend
either treatment based on the type of complications. The final decision
must be left to the patient once all the information is presented to
him or her in an objective manner.
SG, Noble PC, Chatziioannou SN, et al. The effects of rotation on
radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle Int 2002;23:107–111.
LM, Kolb E, Koller MT, et al. Accuracy of Ottawa ankle rules to exclude
fractures of the ankle and mid-foot: systematic review. BMJ 2003;326(7386):417.
A, Ebraheim NA, Mekhail AO, et al. External rotation—lateral view of
the ankle in the assessment of the posterior malleolus. Foot Ankle Int 1999;20:379–383.
EJ, Csongradi TZ, Bleck EE. Early complications in the operative
treatment of ankle fractures: influence of delay before operation. J Bone Joint Surg (Br) 1991;73:79–82.
S, Nasell H, Bergman B, et al. Functional outcome and quality of life
in patients with type B ankle fractures: a two year follow-up study. J Orthop Trauma 1999;13:363–368.
GD, Renaud E, Dagenais G, et al. Double-blind randomized prospective
study of efficacy of antibiotic prophylaxis for open reduction and
internal fixation of closed ankle fractures. J Orthop Trauma 1994;8:64–66.
B, Weber BG, Simpson LA. The dorsal antiglide plate in the treatment of
Danis-Weber type-B fractures of the distal fibula. Clin Orthop Rel Res 1990;259:204–209.
OM. Osteoarthritis of the ankle after foreign-body reaction to
absorbable pins and screws: a three to nine year follow-up study. J Bone Joint Surg (Br) 1998;80:333–338.
ARA, van der Elst M, Breederveld RS, et al. Surgical treatment of
fracture-dislocations of the ankle joint with biodegradable implants: a
prospective randomized study. J Trauma 1993;34:82–84.