SHOULDER INSTABILITY
focused on constraining the joint through soft-tissue reconstruction,
which often has distorted anatomy instead of anatomically repairing the
primary lesion of an injured capsule or labrum. Foremost examples of
these reconstructive techniques include transfer of the subscapularis
(Magnuson-Stack), imbrication of the subscapularis and capsule
(Putti-Platt), and transfer of the coracoid process and conjoined
tendon (Bristow-Latarjet). As surgeons have developed a better
understanding of the functional anatomy of the shoulder, treatment of
shoulder instability has relied on anatomic restoration.
30% glenohumeral contact at any one angle, stereophotogrammetric
studies show close congruency between the articular surfaces of the
glenoid cavity and the humeral head (148).
Notwithstanding a flat radiographic appearance of the glenoid, the
varying cartilage thickness on its surface allows a close
concavity–convexity match to the humeral head, which provides stability
through dynamic contraction of the rotator cuff. It has been termed the
concavity-compression mechanism of stability and is described in further detail below (88,89).
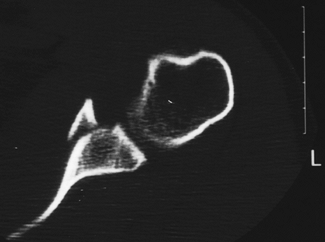
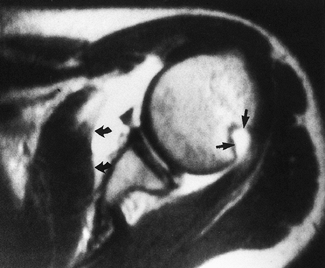
These conditions disrupt the concavity-compression effect by decreasing
the surface area of contact and disrupting the close congruent
fit of articular surfaces (18,55,182).
Similarly, large Hill–Sachs or reverse Hill–Sachs lesions,
posterolateral or anterolateral humeral head impaction fractures
respectively, can affect this articular relationship (Fig. 80.2) (22,131,133,134).
These fractures are created by direct contact between the humeral head
and the glenoid rim during shoulder dislocations. While these lesions
are present in more than 80% of anterior dislocations and 25% of
anterior subluxations, they are rarely a contributing factor to
instability. They become biomechanically relevant to joint stability
when osteoarticular loss involves greater than 30% of the humeral head
surface.
 |
|
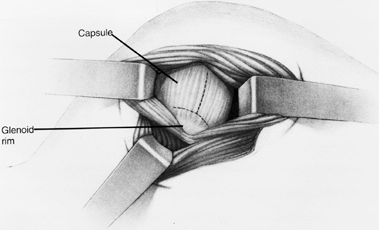
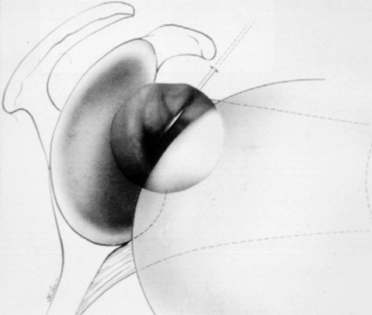
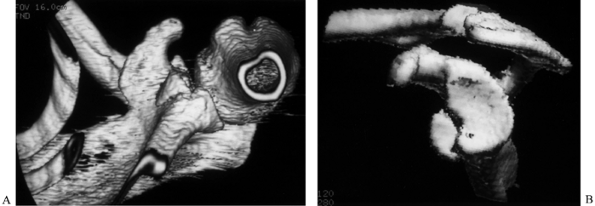
Figure 80.1. Axial CT demonstrates a significant bony Bankart lesion with disruption of the concavity-compression mechanism.
|
 |
|
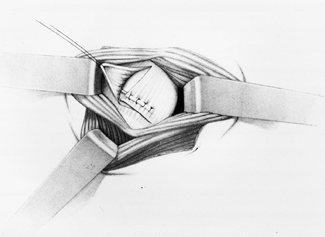
Figure 80.2. Axial MRI with contrast demonstrates anterior capsular stripping (large curved arrows) with an associated Bankart lesion. In addition, a large Hill–Sachs lesion can be seen posteriorly (smaller straight arrows).
|
glenoid cavity and contributes to glenohumeral stability by three
mechanisms:
ligaments and the long head of the biceps brachii (102,158).
glenoid cavity, improving the conforming fit of the humeral head within
the glenoid (47).
implicated as the primary lesion associated with traumatic anterior
shoulder dislocation (186,187).
Because variability in the anatomy of the labrum is considerable, it is
important to distinguish between true labral detachment and a variation
of normal anatomy (31,181).
As a rule, the labrum is often loosely attached to the glenoid rim
above the equator of the glenoid cavity, and in fact there may be
little or no labrum present along the anterosuperior glenoid rim. This
anatomic variant has been termed a sublabral foramen (hole) (Fig. 80.3).
 |
|
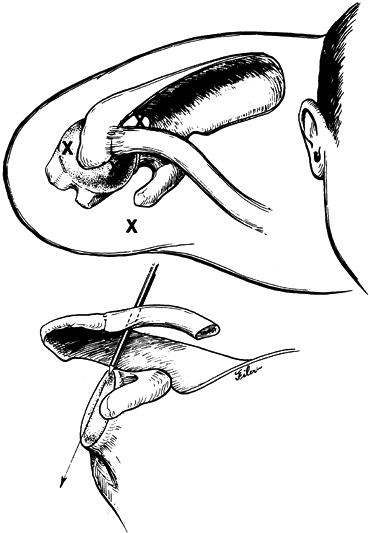
Figure 80.3.
Arthroscopic view through a posterior portal demonstrates an anatomic variant of the anterior glenoid labrum referred to as a sublabral hole. This should not be confused with a true Bankart lesion or a superior labrum anterior posterior (SLAP) lesion. (From Warner JJP, Warren RF. Arthroscopic Bankart Repair Using a Cannulated Absorbable Fixation Device. Oper Tech Orthop 1991;1:192, with permission.) |
attached to the glenoid rim and is actually a fibrocartilaginous
transition zone to the glenohumeral ligaments. It functionally deepens
the glenoid fossa, thus enhancing the concavity-compression mechanism
of stability. Detachment of the glenoid labrum below the equator of the
glenoid represents a functional disruption of the origin of the
inferior glenohumeral ligament (IGHL), as well as a decrease in the
concavity of the glenoid cavity.
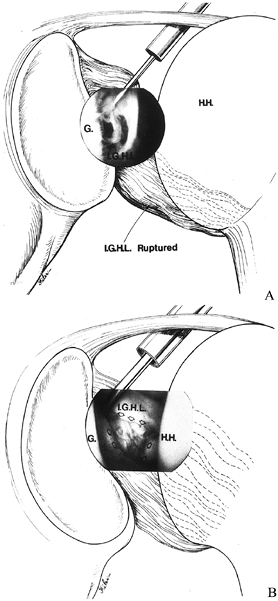
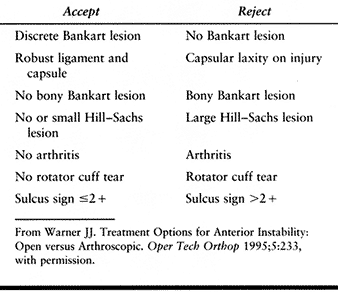
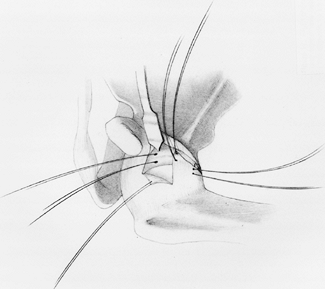
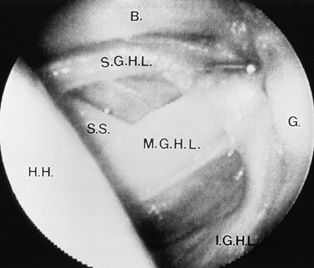
characterized by collagenous thickenings of varying development in its
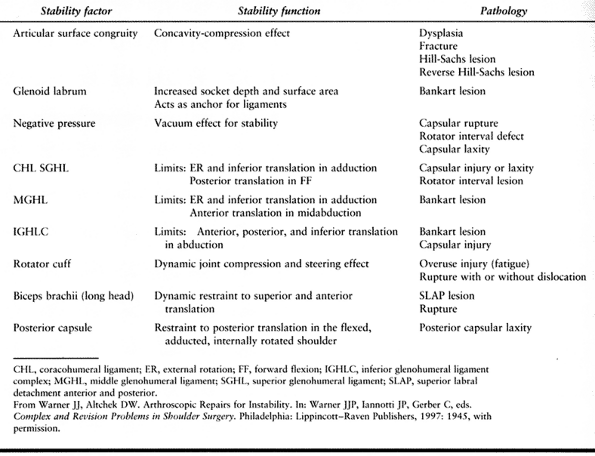
anterior portion (Fig. 80.4) (11,13). These thick bands are called the glenohumeral ligaments due to their location along the glenoid rim. Table 80.1
shows the specific functional role of each ligament and the resulting
pathology when each is injured. These ligaments and their interposed
capsule are normally lax when the shoulder is positioned in the mid
range of rotation. The rotator cuff muscles and long head of the biceps
tendon (dynamic stabilizers) create the important concavity-compression
effect (described below) that maintains stability (116,126,172).
 |
|
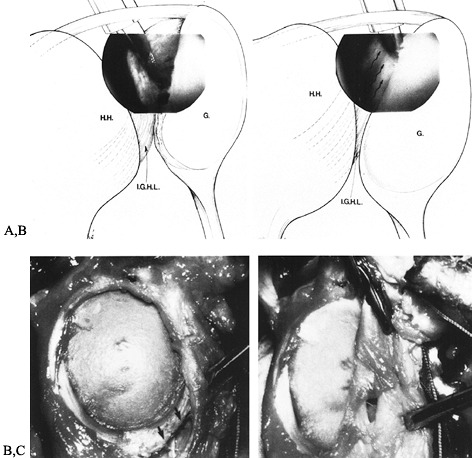
Figure 80.4. Arthroscopic view demonstrates normal anterior capsular ligamentous anatomy as viewed through a posterior arthroscopic portal (H.H., humeral head; G, glenoid; B, biceps tendon; S.G.H.L., superior glenohumeral ligament; S.S., subscapularis; M.G.H.L., middle glenohumeral ligament; I.G.H.L.,
inferior glenohumeral ligament). (From Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing Mechanisms Preventing Anterior Dislocation of the Glenohumeral Joint. J Bone Joint Surg [Am] 1981;63:1209, with permission.) |
 |
|
Table 80.1. Glenohumeral Stability
|
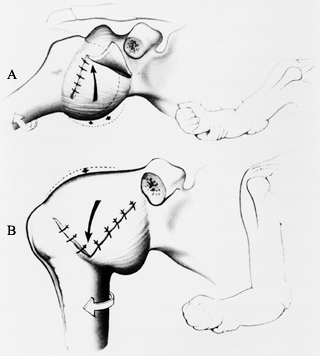
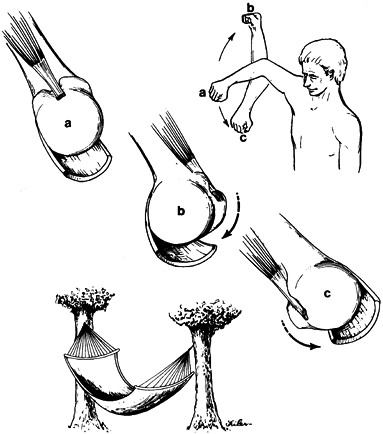
glenohumeral ligaments function in a reciprocal fashion, acting as
checkreins to prevent excessive humeral head translation at the
extremes of motion (37,113,114 and 115,160). O’ Brien et al. (113,114)
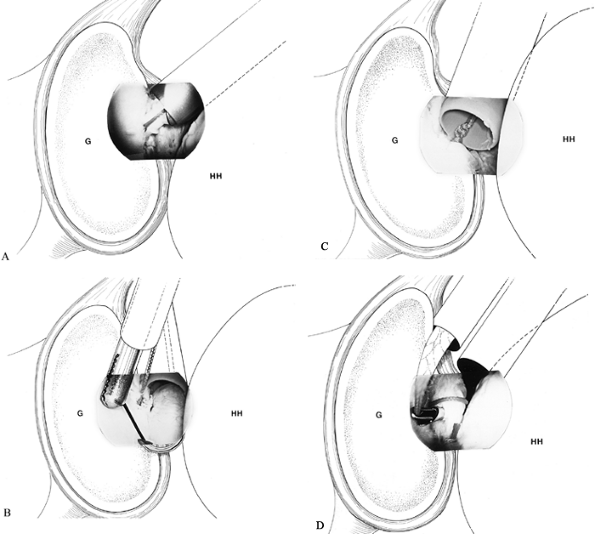
compared the IGHL to a hammock; its anterior and posterior bands should
tighten at terminal external rotation with the arm abducted 90° (Fig. 80.5).
In addition to their action as static restraints to excessive
translation and rotation, the capsuloligamentous structures may also
have a proprioceptive role (85,173).
It has been postulated that stretch and motion receptors within the
glenohumeral capsule and ligaments relay proprioceptive feedback to the
dynamic muscle stabilizers, thus acting as an afferent feedback loop to
modulate muscle activity about this joint during active motion.
 |
|
Figure 80.5. The IGHL controls glenohumeral instability in a manner analogous to a hammock. A: With the arm in 90° of abduction, the IGHL supports the humeral head inferiorly. B: With external rotation, the anterior band of the ligament prevents anterior translation of the humeral head. C:
The posterior band functions in a similar fashion with internal rotation to prevent posterior translation of the humeral head. (From Warner JJP, Caborn DN. Overview of Shoulder Instability. Crit Rev Phys Rehabil Med 1992;4:145, with permission.) |
anatomy is essential for surgeons who seek to reestablish anatomy in an
unstable shoulder (171). Procedures that repair
the soft tissues while the joint is positioned in the mid range of
motion shorten the capsuloligamentous complex. As a result, the joint
may be captured, preventing full external rotation, an outcome
associated with the development of early arthritis (59,61).
joint is the presence of negative (less than atmospheric)
intraarticular pressure. This condition results from high osmotic
pressure in the interstitial tissue, which draws water from the joint (94).
Any force that tends to displace the humeral head away from the glenoid
increases this vacuum effect resisting further humeral head
displacement. This effect is clinically relevant when the arm is
hanging at the side and the muscles of the shoulder are relaxed (19,53,82,169).
Conditions that disrupt this vacuum effect include capsular rupture,
intraarticular fracture, developmental or acquired capsular defects
(i.e., rotator interval lesion or capsular rupture), or a large,
capacious capsule (45,169).
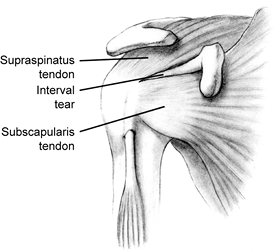
This region of the capsule is a triangular space whose base is located
near the coracoid process and its apex near the biceps sulcus (Fig. 80.6).
The interval is bordered superiorly by the anterior margin of the
supraspinatus tendon and inferiorly by the superior border of the
subscapularis tendon. The area is completely bridged by capsule and
supplemented by the coracohumeral and the superior glenohumeral
ligaments. A deficiency
of
these ligaments and communication of the joint with the subdeltoid
space lead to a significant sulcus sign (inferior laxity) (described
later).
 |
|
Figure 80.6.
Anatomy of the rotator interval. Injury to this region is associated with an increased sulcus sign with the arm at the side that does not decrease with full external rotation. (From Zarins B. Bankart Repair for Anterior Shoulder Instability. Tech Orthop 1989;3:23, with permission.) |
consisting of the teres minor, infraspinatus, supraspinatus, and
subscapularis muscles. These muscles encircle the glenohumeral joint,
and their insertion sites are broadly intermeshed with the underlying
joint capsule (29,32,34).
These intrinsic muscles have relatively short lever arms and pass close
to the axis of rotation of the joint. As a result, they act more as
primary stabilizers than as primary movers of the glenohumeral joint.
The net effect of contraction of the rotator cuff muscles is to create
a compressive load across the glenohumeral joint. This load steers the
humeral head into the glenoid fossa, creating the concavity-compression
mechanism (Fig. 80.7) (14,17,71,88,125,135,161).
 |
|
Figure 80.7. The dynamic stability provided by the rotator cuff muscles produces a concavity-compression mechanism.
|
macrotrauma that exceeds the ultimate failure strength of the
tendon(s). Alternatively, injury can be the result of repetitive
submaximal loads that cumulatively disrupt the tendon fibers. Each
scenario can be associated with actual shoulder instability. In
individuals older than 40 years, the tensile properties of the rotator
cuff tendons tend to deteriorate more rapidly than those of the
glenohumeral capsule and ligaments. As a result, patients in this age
group have a high incidence of rotator cuff tears associated with a
traumatic shoulder dislocation (108,147).
subject the shoulder to repetitive forces that cause gradual injury to
the rotator cuff. For example, subtle degrees of shoulder subluxation
may occur with repetitive motions such as in swimming. The
capsuloligamentous tissues may stretch, and the joint may become more
lax. An overload of the rotator cuff muscles can occur. The active
(eccentric) contraction of the rotator cuff, which decelerates the
humeral head during the swimming stroke or throwing motion, has been
associated with rotator cuff injury (20).
Contraction markedly limits anterior and superior translation of the
glenohumeral joint, increases torsional rigidity of the joint, and
decreases strain in the IGHL. Clinical experience based on arthroscopic
observations has demonstrated a correlation between shoulder
instability and the presence of the superior labral anterior posterior
(SLAP) lesion (145,172). This injury pattern represents a detachment of the origin of the long head of the biceps.
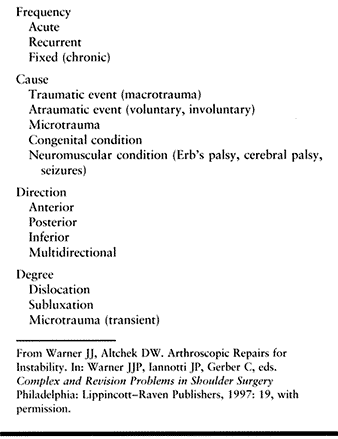
the Hospital for Special Surgery. The system categorizes patients with
shoulder instability on the basis of four criteria: frequency, cause,
direction, and degree (Table 80.2) (33,142,187).
 |
|
Table 80.2. Shoulder Instability Classification
|
the previous 24 hours. The number of recurrences (frequency of instability)
is also critical in this classification scheme, as it contributes to
the level of damage to anatomic structures. This characteristic is
extremely important when taken into consideration along with the degree
and cause of the instability. This component of the history is critical
in determining the appropriate treatment.
traumatic, microtraumatic, and atraumatic groups but also includes
congenital and neuromuscular causes. The atraumatic group includes
patients who exhibit a voluntary component. In this classification,
these patients can be further subdivided into group I: voluntary instability, which is arm-position-dependent and usually posterior; and group II:
voluntary instability exhibited by an ability to selectively contract
muscles, causing a dislocation. While patients in group I can
voluntarily demonstrate their instability, they choose to avoid
dangerous arm positions. This condition subsequently affects activities
of daily living (142). Conversely, patients in
group II tend to have an underlying psychiatric problem, using their
instability as a means to control their environment (132).
also important in determining appropriate treatment options.
Dislocation refers to complete dissociation of the articular surfaces
of the humeral head and glenoid cavity. Subluxation describes increased
humeral head translation within the glenoid cavity. Initial open
procedures focused on the treatment of true glenohumeral dislocation.
Arthroscopic evaluation has heightened the awareness of subtle labral,
articular, and ligamentous damage that occurs because of unrecognized,
recurrent episodes of subluxation (7,22,24,68,112).
has been a critical component of most classification systems.
Traditionally, there was an assumption that 95% of shoulder instability
was anterior (25). It has become increasingly
apparent, however, that many athletes with ligamentous laxity have
instability that is primarily posterior in nature (48,49,156,178).
These patients suffer recurrent posterior subluxation and have a
history of posterior shoulder pain rather than complaints of frank
instability. This category of patients is more prevalent than
previously recognized but should be distinguished from the rare true
posterior dislocation that results from an acute traumatic event (16,110).
a series of 40 patients with 41 locked posterior shoulder dislocations.
The initial physician missed the diagnosis in the majority of cases
reviewed. In this series, the causes of posterior dislocation were
motor vehicle accidents, seizures, alcohol-related injuries, or
electroshock therapy. Recurrent anterior subluxation may also manifest
as pain rather than instability. Repetitive, high-energy, overhead
activities can cause progressive attenuation of the capsular,
ligamentous, and labral structures (2,78,159).
As these static stabilizers fail and the dynamic stabilizers weaken,
anterior subluxation occurs, leading to impingement symptoms.
Recognition of the underlying problem is critical in obtaining a
successful surgical outcome.
A patient’s age, occupation, employment status, activity level, hand
dominance, and other medical problems are helpful in classifying the
nature of the instability. Certain circumstances, such as work-related
injuries or those with associated litigation, might affect patients’
perceptions of their disabilities as well as their expectations for
recovery and compliance with treatment (180).
This symptom is likely associated with a traumatic subluxation of the
joint and the presence of a Bankart lesion. Another example is a
patient who gives a
history
of having had a seizure and then awakening with the sensation of the
joint “out of place.” This situation suggests a posterior dislocation
as the result of unchecked internal rotation forces overcoming the
weaker external rotators of the shoulder.
which activities cause the pain? Question athletes as to the type of
sport, the position played, and the duration, frequency, and level of
involvement. For example, throwers, swimmers, or tennis players may
develop excessive capsular laxity as a result of subjecting their
shoulders to repetitive microtrauma (83,125).
The result is recurrent shoulder subluxation, which can create a sense
of “looseness” or “slipping” with activity. In addition, as previously
stated, secondary “nonoutlet” impingement can occur as anterior
instability decreases the subacromial space, causing pain with overhead
activities. Further, these same subluxations can create damage to the
superior labral area, creating a SLAP lesion. Posterior subluxation has
also been documented in athletes who require repetitive arm motion in
front of the body, such as offensive-line football players and
volleyball, softball, and baseball players (48,156,178). Throwing sports in particular lead to complaints of posterior
shoulder pain during the follow-through phase, which has been
associated with posterior subluxation and resultant microtrauma to the
posterior capsulolabral complex.
abnormal motion patterns and atrophy, palpation to localize painful
areas, assessment of both active and passive range of motion,
measurement of strength of the rotator cuff muscles, neurovascular
evaluation, and finally provocative maneuvers for instability. Examine
the opposite shoulder for comparison.
scapulothoracic substitution for glenohumeral motion, scapular winging,
and other abnormal motion patterns. Atrophy of the spinatus muscles may
indicate a longstanding associated rotator cuff tear or injury to the
suprascapular nerve. Similarly, atrophy of the deltoid may indicate an
axillary nerve injury.
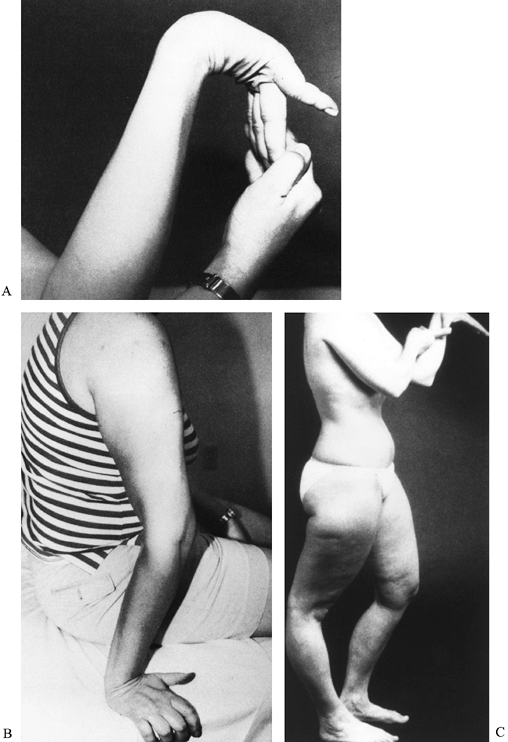
laxity, including the ability to hyperextend the elbows more than 10°,
apply the thumb to the forearm, hyperextend the metacarpophalangeal
joints more than 90°, or touch the palm of each hand to the floor while
keeping the knees extended (Fig. 80.8). While
there is no direct relationship between generalized ligamentous laxity
and shoulder instability, there is some association between hyperlaxity
and glenohumeral capsular development.
 |
|
Figure 80.8. Systemic laxity. A: Wrist and metacarpophalangeal joint hyperextension. B: Elbow joint hyperextension. (A and B from Warner JJP. Shoulder. In: Miller MD, Cooper DE, Warner JJP, eds. Review of Sports Medicine and Arthroscopy. Philadelphia: WB Saunders, 1995:125, with permission.) C:
Knee hyperextension and thumb-to-forearm hyperflexibility. (From Gerber C. Observations on the Classification of Instability. In: Warner JJP, Iannotti JP, Gerber C, eds. Complex and Revision Problems in Shoulder Surgery. Philadelphia: Lippincott–Raven Publishers, 1997:16, with permission.) |
Before attempting any reduction maneuvers, perform a careful
neurovascular examination to rule out brachial plexus and, more
specifically, axillary nerve injuries (38,57,152).
The latter condition may sometimes escape detection, as decreased
sensation over the lateral deltoid is not always present with an injury
to this nerve. In older (>60 years) individuals or younger ones who
have sustained a severe trauma, be aware of the possibility of an
associated fracture of the humerus (62). Proper radiographic imaging is particularly important before attempting closed reduction in such cases.
acute shoulder dislocation. Perform all maneuvers as a gradual and
gentle technique with appropriate analgesia to ensure muscle
relaxation. Intravenous analgesia and intraarticular injection of a
regional anesthetic are both successful, appropriate methods of
anesthesia. A method of gentle traction in line with the arm using
countertraction is usually successful.
unrecognized chronic (fixed) dislocation. The dislocation is most often
posterior, although it may be anterior, and typically occurs in
patients who are poor historians because of either alcohol use or
dementia (64). In a patient with a fixed
posterior subluxation, there is limitation of external rotation
compared with the opposite shoulder. In addition, there is flattening
of the anterior aspect of the shoulder with an associated prominence of
the coracoid process and possibly some prominence and rounding of the
posterior aspect of the shoulder. The application of excessive force in
attempting a closed reduction in such a patient risks neurovascular
injury or fracture.
orthopaedic surgeon in the office setting. They may have had a
documented episode of instability or an injury with pain but no true
sense of shoulder instability. After a careful neurovascular
examination, it is important to assess active and passive range of
motion. A discrepancy between active and passive motion may indicate
either an associated rotator cuff tear or a nerve injury.
tear in the setting of shoulder instability, a condition that is
frequently missed (51,165).
Patients with such tears have passively increased external rotation
with the arm adducted at the side, as well as associated apprehension
in this position. Strength assessment is also important. Significant
external rotation weakness may indicate a rotator cuff tear.
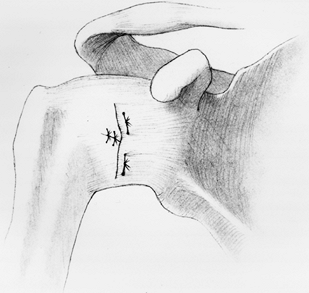
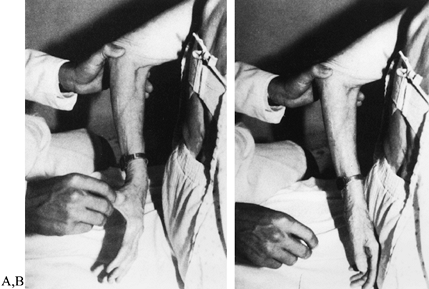
subscapularis tear. In this situation, the patient has an associated
lift-off sign (Fig. 80.9). If the patient lacks
adequate internal rotation to perform this test, perform the
belly-press maneuver instead to determine the patient’s ability to pull
the forearm in a posterior direction toward the mid abdomen while
maintaining the flexed elbow anterior
to
this point. If the elbow remains posterior to the anterior aspect of
the mid abdomen, there is likely a subscapularis tendon tear.
 |
|
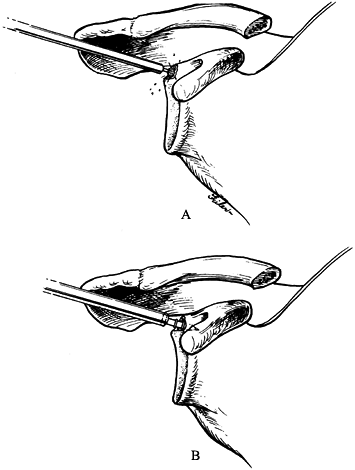
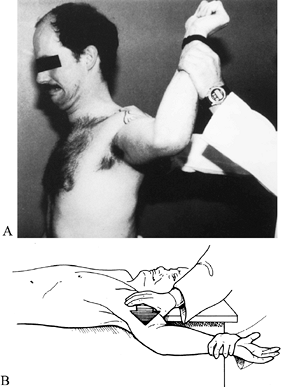
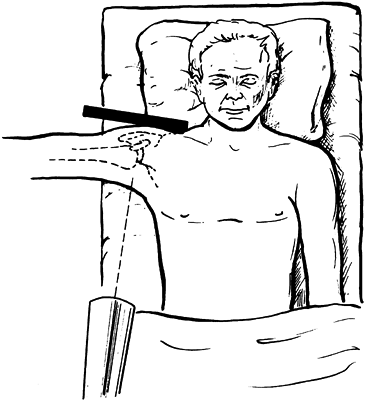
Figure 80.9. Lift-off sign. A: With the arm internally rotated, assess the patient’s ability to hold the arm off the lumbar region. B:
An inability to perform this function is clinically consistent with a subscapularis rupture. If the patient lacks sufficient internal rotation to perform this test, perform the belly-press maneuver. (From Warner JJP. Shoulder. In: Miller MD, Cooper DE, Warner JJP, eds. Review of Sports Medicine and Arthroscopy. Philadelphia: WB Saunders, 1995:156, with permission.) |
described to assess symptomatic humeral head translation and the
direction of this movement. Neer and Foster (107)
originally described the apprehension test for anterior instability.
With the patient seated or standing, place the symptomatic shoulder
into a position of 90° of abduction and maximum external rotation. Then
move the arm so that it is posterior to the plane of the scapula, and
apply an anterior force to the humeral head. The patient’s withdrawing
from the examiner or complaining about a sense of shoulder instability
demonstrates apprehension (Fig. 80.10A).
 |
|
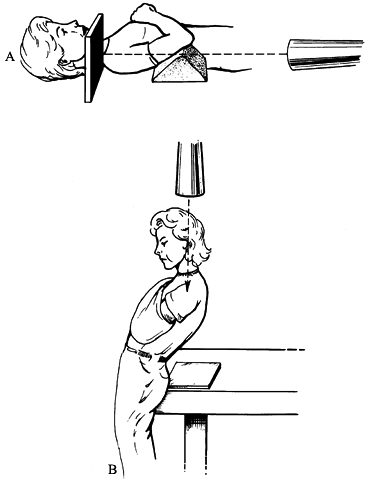
Figure 80.10. Apprehension test. A:
In a patient with suspected anterior instability, abduct the arm 90° and maximally externally rotate it with posterior pressure on the humeral head. The patient should express demonstrable anxiety over a possible dislocation.B: The relocation maneuver is performed with the patient supine and the arm in the same compromised position. (From Warner JJP. Shoulder. In: Miller MD, Cooper DE, Warner JJP, eds. Review of Sports Medicine and Arthroscopy. Philadelphia: WB Saunders, 1995:128, with permission.) |
and may in fact be present with other conditions such as arthritis or
rotator cuff disease. Kvitne and Jobe (83)
proposed a modification of this maneuver to increase its specificity
for anterior instability. Place the patient in a supine position, and
perform the apprehension test as described above. Ask whether the
patient has a sense of instability or simply pain. Place posterior
pressure on the humerus, and ask whether this pressure relieves the
sense of apprehension or pain (Fig. 80.10B).
This “relocation maneuver” increases the specificity of the diagnosis
of instability if the patient reports decreased apprehension. If this
maneuver simply reduces pain, it is not diagnostic of instability and
may be associated with a variety of other diagnoses, including a SLAP
lesion or impingement syndrome (150).
modification to this test increases both its sensitivity and
specificity for the diagnosis of anterior shoulder subluxation. Perform
the apprehension and relocation tests as described above. If the
patient reports pain and not true apprehension, inject the subacromial
space with 10 ml of lidocaine 1% (Xylocaine). After 10 minutes, repeat
the examination. If the pain is due to rotator cuff disease, the
injection will eliminate it. If, however, the pain is due to labral
injury, it will persist after a subacromial injection (166).
to develop the anterior and posterior drawer test to assess the
shoulder for excessive translation compared with the contralateral
side. Others have found merit in this method of examination and have
developed grading scales for the degree of shoulder laxity (3,30,65).
These tests may offer some insight into the degree and direction of
instability. If one assesses laxity of the shoulder in an office
setting, it is important to determine whether translation of the
humeral head is greater on the painful side and whether this
translation causes symptoms (49). We have found
laxity assessment by drawer testing to be of limited value in the
office setting because patients tend to guard the painful shoulder.
Instead, this method is used during examination under anesthesia to
confirm the suspected degree and direction of shoulder instability.
proposed a grading scale for translation of the humeral head on the
glenoid. Instability is graded on a scale of 0–3+ for all three
directions. For anterior and posterior drawer testing, a grade of 0
represents no humeral head translation, while movement of the humeral
head up to but not over the glenoid rim represents 1+ instability.
Translation of the humeral head over the glenoid rim with an associated
spontaneous reduction with relief of pressure represents
2+ instability. Frank dislocation and locking of the humeral head over the glenoid rim is graded as 3+ instability.
office or in the operative setting, it is important to bear in mind
that the position of the arm determines the degree of tension in the
glenohumeral ligaments. With the arm at the side in adduction, the IGHL
is relatively lax, and anterior and posterior drawer testing may be of
limited value. In abduction, the IGHL comes underneath the humeral head
and forms a hammock that passively limits anterior, posterior, and
inferior translation (113,114).
Perform anterior drawer testing with the shoulder positioned in
abduction in the plane of the scapula. Maintain the arm in the neutral
rotation while using one hand to place an axial load along the humerus
and the other hand to apply an anterior or posterior force to the
humerus (Fig. 80.11). Often you can feel the
humeral head move back into the glenoid rather than out of the glenoid
during this maneuver. The patient may note a painful click with such a
maneuver. In our experience, this test is particularly helpful in
identifying posterior instability.
 |
|
Figure 80.11.
Anterior drawer test. With the arm in abduction and neutral rotation, apply an anterior force to the posterior aspect of the humerus to assess anterior humeral head stability. Perform the posterior drawer test with the arm in adduction, forward flexion, and internal rotation. Then apply a posterior force to the arm to assess posterior stability. (From Warner JJP. Shoulder. In: Miller MD, Cooper DE, Warner JJP, eds. Review of Sports Medicine and Arthroscopy. Philadelphia: WB Saunders, 1995:138, with permission.) |
examiner to elicit posterior apprehension. Perform this modification by
placing the patient’s arm in 90° of forward flexion and adduction while
applying an axial load down the shaft of the humerus. Pain and a
palpable shift and click suggest posterior labral injury and
instability.
With the patient seated, load the abducted shoulder axially into the
glenoid with one hand, and with your other hand, palpate the posterior
aspect of the shoulder. Then bring the arm into horizontal adduction
anterior to the plane of the scapula; the humeral head may sublux
posteriorly. Then bring the humerus posterior to the plane of the
scapula; the humeral head may suddenly reduce into the glenoid. A
palpable shift and pain accompany a positive test.
originally described it as the hallmark of inferior and
multidirectional instability (MDI). Unfortunately, a common
misconception has been that a large sulcus sign that is asymptomatic,
thus indicating inherent joint laxity, is a positive finding. The key
point is that this maneuver should be associated with pain and should
reproduce the patient’s symptoms to be clinically relevant as a finding
of inferior instability.
 |
|
Figure 80.12.
Sulcus sign. Assess inferior displacement of the greater tuberosity from the undersurface of the acromion. (From Gerber C. Observations on the Classification of Instability. In: Warner JJP, Iannotti JP, Gerber C, eds. Complex and Revision Problems in Shoulder Surgery. Philadelphia: Lippincott–Raven Publishers, 1997:22, with permission.) |
adducted at the side. Rotation of the shoulder is very important in
assessing the degree of inferior instability. First, with the arm in
the neutral rotation, pull the humerus inferiorly, and estimate the
amount of separation between the acromion and the humeral head. Grade
it on a 0–3+ scale (3): A separation of 1 cm is
a 1+ sulcus sign, 2 cm is a 2+ sulcus sign, and 3 cm is a 3+ sulcus
sign. Anatomically, a sulcus sign greater than 2+ indicates a capacious
capsule and specific laxity of the anterosuperior capsular region
(rotator interval).
repeat the sulcus sign test. If the sulcus sign remains greater than 2+
with the arm in external rotation, there is a marked deficiency of the
superior capsule, and a large rotator interval defect in the capsule is
likely. This is the result of damage to the superior and middle
glenohumeral ligaments, as well as the coracohumeral ligament. With
this information before surgical repair, you then know that surgical
reconstruction of this region with a capsular shift must be a component
of the operation (60).
in 1990, several examination techniques have evolved to diagnose this
pathology. Andrews reported increased pain in patients during full
shoulder flexion and abduction, with noticeable catching and popping.
Snyder reported pain in patients during resisted shoulder flexion with
elbow extension and forearm supination (biceps tension test).
compression–rotation test. With the patient supine, abduct the shoulder
90°, with the elbow flexed 90°. Apply a compression force to the
humerus to trap the torn labrum (in the same manner as McMurray’s test
for the knee is performed). O’ Brien et al. (114)
suggested a maneuver that they believed is accurate for determining
superior labral injuries. Place the patient’s shoulder in 90° of
forward flexion and then adduct it across the body. Ask the patient to
flex the arm further against resistance when the shoulder is first
internally rotated and then externally rotated. If pain occurs when the
shoulder is rotated internally but not when it is rotated externally,
the test is positive. Unfortunately, this test does not distinguish
between acromioclavicular joint disease and a superior labral tear. We
have found this test more useful than the other methods described above.
acute dislocation or suspected subluxation is a true anteroposterior
(AP) view and an axillary view. These images will allow accurate
determination of the position of the humeral head relative to the
glenoid. A true AP radiograph is obtained by angling the x-ray beam 45°
relative to the sagittal plane of the body (Fig. 80.13). A scapular Y or transcapular view can also give useful information about the position of the humeral head (Fig. 80.14), but it is not as accurate as an axillary view (Fig. 80.15).
If a standard axillary view cannot be obtained, a Velpeau axillary view
without removing the patient’s arm from the sling will suffice (Fig. 80.16).
 |
|
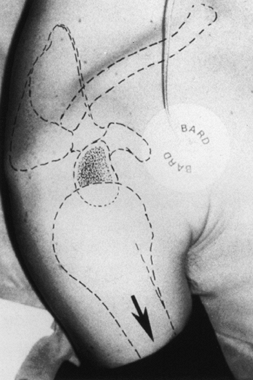
Figure 80.13.
A routine AP shoulder radiograph shows overlap of the anterior and the posterior glenoid rims. A true AP radiograph demonstrates superimposition of the anterior and the posterior glenoid rims, producing an excellent view of the glenohumeral joint. (From Warner JJP, Caborn DN. Overview of Shoulder Instability. Crit Rev Phys Rehabil Med 1992;4:145, with permission.) |
 |
|
Figure 80.14.
Transcapular or Y view of the glenohumeral joint allows assessment of the humeral head location in relation to the glenoid cavity. (From Warner JJP, Caborn DN. Overview of Shoulder Instability. Crit Rev Phys Rehabil Med 1992;4:145, with permission.) |
 |
|
Figure 80.15.
Axillary view represents the “gold standard” in radiographic assessment of location of the humeral head relative to the glenoid cavity. (From Warner JJP, Caborn DN. Overview of Shoulder Instability. Crit Rev Phys Rehabil Med 1992;4:145, with permission.) |
 |
|
Figure 80.16. Two common techniques used when a standard axillary view is difficult to obtain include the trauma axillary lateral (A) and the Velpeau axillary view (B). (From Warner JJP, Caborn DN. Overview of Shoulder Instability. Crit Rev Phys Rehabil Med 1992;4:145, with permission.)
|
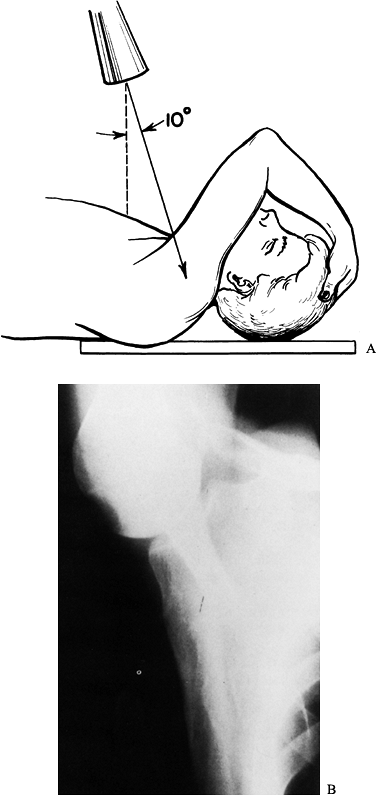
with the arm in internal rotation may demonstrate a Hill–Sachs lesion.
A Stryker notch view is a special view that will also demonstrate a
Hill–Sachs lesion (Fig. 80.17) (43,121).
 |
|
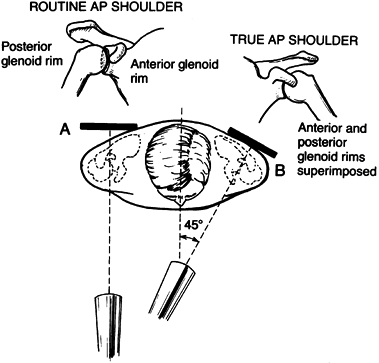
Figure 80.17. A: Arm position for obtaining the Stryker notch view. B:
This view can demonstrate a Hill–Sachs fracture on the posterior humeral head surface. (From Warner JJP, Caborn DN. Overview of Shoulder Instability. Crit Rev Phys Rehabil Med 1992;4:145, with permission.) |
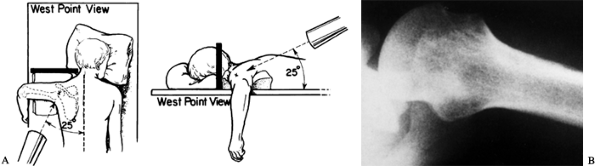
patient suspected of having had an episode of instability. Take the
image with the patient prone so that the anterior glenoid is shown in
profile without an overlying acromial shadow (Fig. 80.18).
 |
|
Figure 80.18. A: Positioning for the Westpoint axillary view. B:
This view allows visualization of the anteroinferior glenoid rim. (From Warner JJP, Caborn DN. Overview of Shoulder Instability. Crit Rev Phys Rehabil Med 1992;4:145, with permission.) |
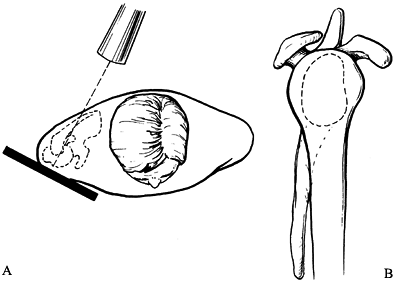
and architecture of the joint or confirmation of the presence of a
Bankart lesion is required. Computed tomography (CT) demonstrates bony
injuries or abnormalities including glenoid hypoplasia, congenital
version anomalies, acquired version abnormalities from erosion, and
glenoid rim fractures (Fig. 80.1 and Fig. 80.19). In addition, it allows measurement of the size of a humeral head defect (Hill–Sachs lesion) in cases of chronic instability (55). When combined with intraarticular dye, CT arthrography also demonstrates a Bankart lesion and articular erosion.
 |
|
Figure 80.19. A: Three-dimensional CT reconstruction of a glenoid rim fracture. B: The same fracture after computerized removal of the humeral head.
|
gadolinium has gained great favor, although unfortunately it is often
used as a screening tool in the evaluation of patients. Its role should
instead be to confirm the presence of lesions that may need surgical
management. It is accurate in the detection of labral pathology (Fig. 80.20) (27,56).
Recent advances in MRI technology such as high-resolution fast-spin and
gradient-echo imaging make these methods particularly appealing for
detecting anterior and superior labral injuries (26).
 |
|
Figure 80.20. A,B: MR arthrogram demonstrates anterior glenohumeral stripping with an associated Bankart lesion.
|
examination under anesthesia (EUA) can confirm or deny the preoperative
impression (30,154).
During EUA, muscle guarding is eliminated, and an accurate assessment
of joint laxity is possible. As previously described, it is essential
that laxity not be confused with instability; thus, it is important to
compare the symptomatic shoulder with the asymptomatic side.
Individuals who have had a previous dislocation will likely have a 2+
or 3+ anterior drawer test result (as described above) for the
symptomatic shoulder compared with a 1+ – 2+ finding in the
asymptomatic shoulder.
necessarily exclude instability because a Bankart lesion may be present
without marked laxity on examination in a patient who has a history of
subluxation (149,171).
Furthermore, in very large individuals, the soft-tissue envelope of the
shoulder may be so large that accurate determination of a centimeter of
translation of the humeral head on the glenoid may not be possible.
both of which are typically associated with MDI. If an individual is
found to have a sulcus sign of more than 2+ and if this persists when
an inferior drawer is applied with the arm in external rotation, there
will be a large rotator interval defect, as well as marked anterior and
inferior capsular laxity. In our hands, this is treated by a modified
capsular shift, along with repair of a Bankart lesion if one is found
to be present (60). Although other surgeons
have used arthroscopic techniques in the treatment of this combination
of problems, we generally treat only pure Bankart lesions with an
arthroscopic repair technique (99,136,159).
when anterior instability is suspected. It is usually in a patient with
congenital laxity who has had a traumatic injury. We usually treat this
condition with an open capsular shift method of repair.
of the anterior and inferior glenohumeral structures by virtue of the
applied traction, but it does not allow the surgeon to easily
manipulate the shoulder through a full range of motion. Moreover, it
can limit access to the anterior glenoid with crowding of the
instrumentation and cannulas on the drapes and body. In addition, if
there is a need to convert to an open procedure, it is usually
necessary to reposition (and therefore reprepare and redrape) the
patient. As stated previously, there is a risk of transient neuropraxia
due to traction (81).
provides unrestricted access to the entire shoulder and allows free
movement of the arm in all planes. In addition, visualization is
possible in a more anatomic orientation. These criteria are essential
if a diagnostic arthroscopy is to be performed that inherently requires
an assessment of the anatomy of the glenohumeral ligaments. Further, it
permits simple conversion from an arthroscopic to an open procedure. In
addition, patients tolerate the use of an interscalene block without
the need for supplemental general anesthesia, in contrast to patients
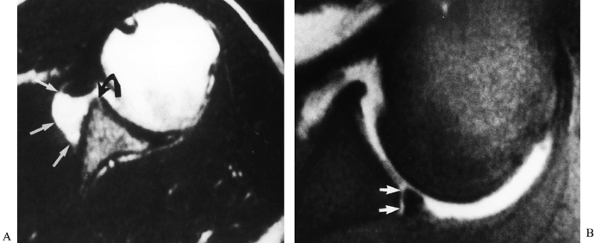
in the lateral decubitus position. Table 80.3 compares the beach-chair position with the lateral decubitus position.
 |
|
Table 80.3. Advantages and Disadvantages of Lateral versus Beach-chair Arthroscopy
|
-
If general anesthesia is used, it is
important to secure the endotracheal tube to the side of the mouth
opposite the injured shoulder. After anesthesia has been obtained,
place the patient into the seated position, and perform an EUA. There
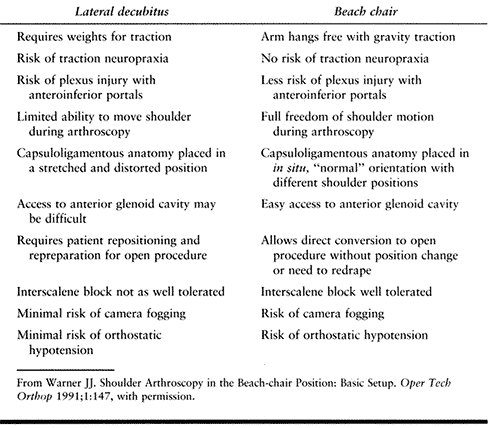
are special beach-chair attachments that can be fitted to the table (Fig. 80.21) (163).
If such a device is not available, place a long beanbag beneath the
patient. In this setting, the table is fully flexed, apex down, at the
patient’s waist; the knees are then flexed downward approximately 45°
with a footplate at the end of the table to prevent the patient from
sliding down the table. Finally, the head of the table is elevated
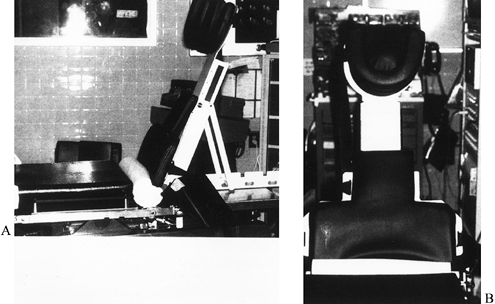
approximately 70° from the horizontal.![]() Figure 80.21. Lateral (A) and anterior (B)
Figure 80.21. Lateral (A) and anterior (B)
views of the beach-chair attachment used for shoulder arthroscopy.
(From Warner JJP. Shoulder Arthroscopy in the Beach-chair Position:
Basic Setup. Oper Tech Orthop 1991;1:147, with permission.) -
Then harden the beanbag, leaving the
entire medial border of the scapula free posteriorly for sterile
preparation and draping. Obtain this same position with the use of a
beach-chair attachment (Fig. 80.22). Place the
uninjured arm on a well padded arm board or a stand that is positioned
at the appropriate height to avoid undue pressure on the neck and
shoulder. Shave the axilla, and prepare and drape the arm from the hand
to the medial border of the scapula posteriorly.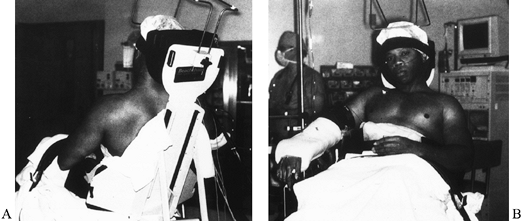 Figure 80.22. Standard patient position for shoulder arthroscopy in the beach-chair position. A: The head is elevated 70° with the medial border of the scapula free and the entire shoulder free posteriorly. B:
Figure 80.22. Standard patient position for shoulder arthroscopy in the beach-chair position. A: The head is elevated 70° with the medial border of the scapula free and the entire shoulder free posteriorly. B:
Anteriorly, the entire shoulder is free, with the uninjured forearm in
a padded stand and the shoulder resting at a comfortable level. (From
Warner JJP. Shoulder Arthroscopy in the Beach-chair Position: Basic
Setup. Oper Tech Orthop 1991;1:147, with permission.) -
Angle the table so that the feet are away
from the operative side to allow better visualization of the television
monitor positioned on the opposite side of the table from the surgeon.
Place a padded sterile stand for instrumentation at knee level on the
opposite side of the table. Pass the tubing and arthroscopic equipment
underneath the arm and across the patient’s chest and then curve them
forward over the shoulder. Use a clamp to secure the tubing in place;
remove all instruments and tubing from beneath the arm and place them
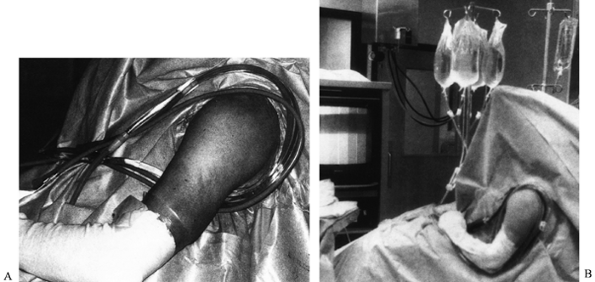
securely on the padded stand (Fig. 80.23).![]() Figure 80.23. A: Appropriate length of the arthroscopy tubing is established by bringing the tubing under the arm and over the shoulder. B:
Figure 80.23. A: Appropriate length of the arthroscopy tubing is established by bringing the tubing under the arm and over the shoulder. B:
Position the table and patient at an oblique angle from the monitor for
better visualization. Note the padded Mayo stand for instrumentation.
(From Warner JJP. Shoulder Arthroscopy in the Beach-chair Position:
Basic Setup. Oper Tech Orthop 1991;1:147, with permission.) -
Adding 1 ampule of epinephrine to each 3-l bag of irrigating solution limits bleeding. Commercially available
P.2156P.2157P.2158P.2159
fluid pressure pumps may be used, although we have had excellent
visualization using simple gravity feed with elevation of two 3-l bags
to a height of at least 7–8 ft (2 m).
-
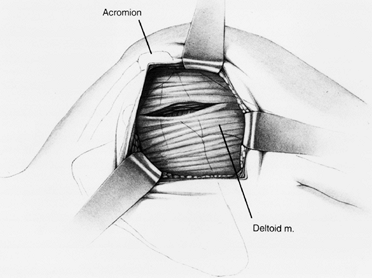
Place the standard posterior portal for arthroscopy 1–2 cm inferior and medial to the posterolateral tip of the acromion (Fig. 80.24) (5,6,23,79,80,172).
Its location can be confirmed by grasping the humeral head and applying
an anterior drawer test. We usually place an 18-gauge spinal needle at
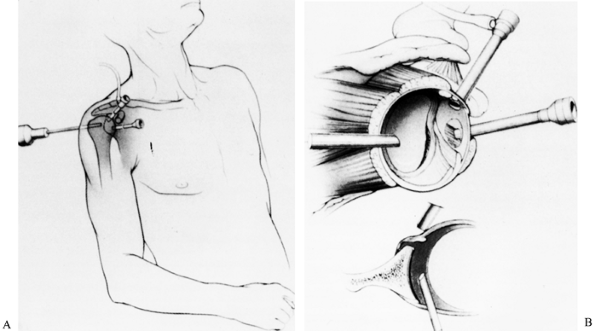
this location to confirm orientation for insertion of the arthroscope.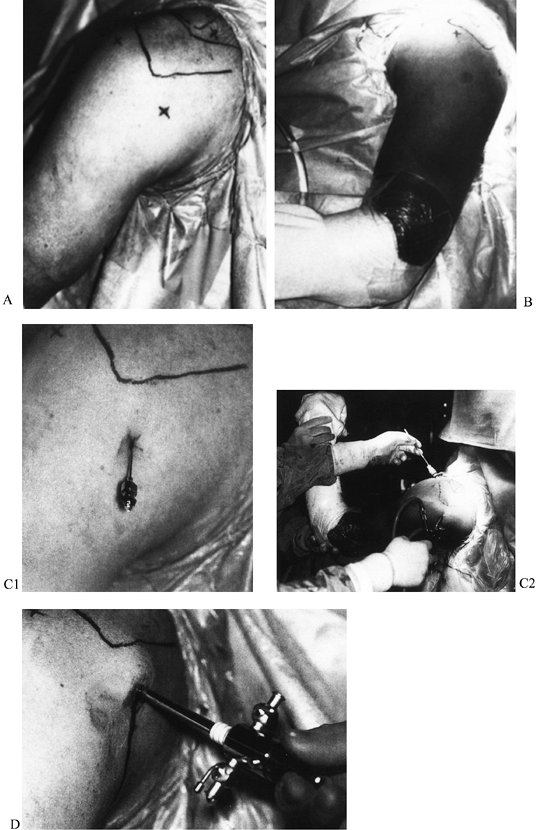 Figure 80.24. Posterior (A) and lateral (B) views of the lateral, posterior, and superior arthroscopic portals. A superior portal is rarely used. C:
Figure 80.24. Posterior (A) and lateral (B) views of the lateral, posterior, and superior arthroscopic portals. A superior portal is rarely used. C:
Insert a spinal needle into the glenohumeral joint posteriorly by
aiming toward the coracoid process, and use it to insufflate the joint
with normal saline. D: Insert an
arthroscopic sheath and blunt trocar into the joint through a posterior
incision in the same direction as the spinal needle. (From Warner JJP.
Shoulder Arthroscopy in the Beach-chair Position: Basic Setup. Oper Tech Orthop 1991;1:147, with permission.) -
Then insufflate the joint with sterile
saline. This step increases hydrostatic pressure in the joint and moves
the humeral head away from the glenoid. It decreases the likelihood of
articular cartilage damage during introduction of the arthroscope into
the joint. Further, reflux of saline out of an open port confirms
proper positioning in the joint. -
An anterosuperior portal is the primary working portal (Fig. 80.24A, Fig. 80.24C).
Locate it by viewing with the arthroscope in the posterior portal and
then placing an 18-gauge spinal needle into the joint just underneath
the long head of the biceps tendon through the rotator interval. This
portal is usually quite vertical in orientation. We make an effort to
place it as superiorly as possible in the rotator interval to avoid
crowding with the anteroinferior portal, which will be used for
placement of the arthroscopic instruments (Fig. 80.25). We usually place a 6 mm cannula in this portal location.![]() Figure 80.25. A: Standard anterosuperior and anteroinferior arthroscopic portals. B:
Figure 80.25. A: Standard anterosuperior and anteroinferior arthroscopic portals. B:
The anterosuperior portal enters the joint just below the biceps
tendon, while the anteroinferior portal enters the joint just above the
subscapularis tendon. Accurate placement of each portal is performed
with the assistance of a spinal needle and an outside-in technique.
(From Warner JJP, Warren RF. Arthroscopic Bankart Repair Using a
Cannulated, Absorbable Fixation Device. Oper Tech Orthop 1991;1:192, with permission.) -
Once these two portals have been
established, perform a review of the joint. A careful inspection begins
with the biceps tendon and its origin and continues over the rotator
cuff and posterior humeral head. Then inspect the glenoid rim (anterior
and posterior) and glenohumeral ligaments (Fig. 80.26). In patients with a presumptive
P.2160P.2161
diagnosis of instability, look specifically for a Bankart lesion,
capsular rupture, capsular laxity, a SLAP lesion, rotator cuff tear
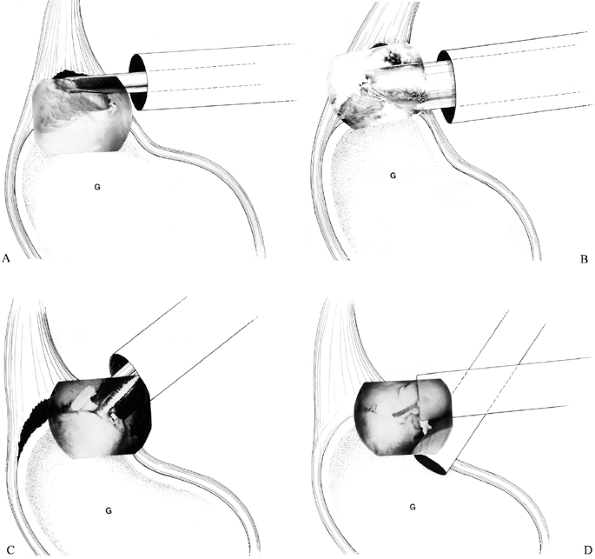
(partial or full), a Hill–Sachs lesion, or chondral injuries.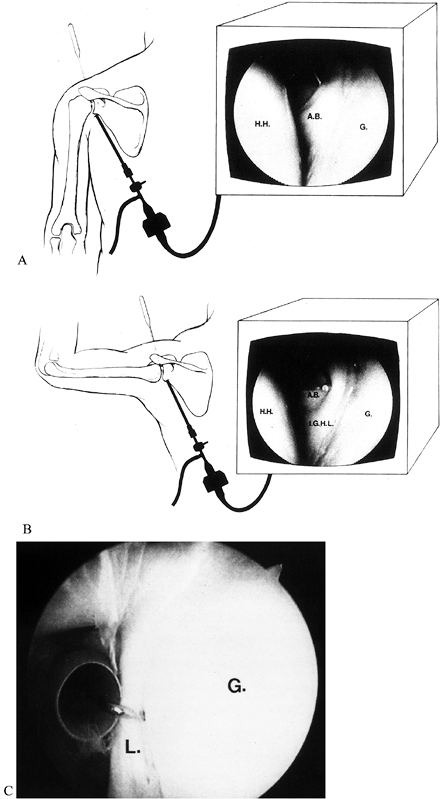 Figure 80.26. A: The anterior band of the IGHL is visualized posteriorly and probed anteriorly with the arm in an adducted position. B: External rotation and abduction of the arm to 90° should increase tension in the ligament, producing a hammock-like effect. C:
Figure 80.26. A: The anterior band of the IGHL is visualized posteriorly and probed anteriorly with the arm in an adducted position. B: External rotation and abduction of the arm to 90° should increase tension in the ligament, producing a hammock-like effect. C:
Probe analysis of the anterior labrum through the anterosuperior
portal. (From Warner JJP. Shoulder Arthroscopy in the Beach-chair
Position: Basic Setup. Oper Tech Orthop 1991;1:147, with permission.) -
SLAP lesions are typically type II in nature and are amenable to repair with current arthroscopic techniques (20,44,172,184).
In patients younger than 45 years, rotator cuff tears are typically
partial-thickness undersurface lesions of the supraspinatus tendon and
are treatable through gentle debridement and correction of the
underlying instability (156). Larger tears are associated with dislocations in patients older than 40 years (109).
Pay careful attention to the presence of a subscapularis tendon injury
in patients older than 40. These injuries usually require formal open
repair. Significant glenoid erosion, a large Hill–Sachs lesion, or
frank posttraumatic arthritis signifies longstanding instability with
associated capsular laxity or, in the worst scenario, dislocation
arthropathy. -
The drive-through sign is a nonspecific,
though somewhat helpful, finding for capsular laxity, described by
Warren and associates (118,166,178).
This finding is positive if you can sweep the arthroscope with little
resistance from anterior to inferior into the axillary pouch. -
A modification of the drive-through sign that we have found more specific is termed the arthroscopic drawer test (166).
View through the posterior portal with the patient’s shoulder abducted.
With the arm in abduction and external rotation, apply an anterior
drawer. If the humeral head moves over the glenoid rim when the arm is
in this position, there is significant capsular laxity (Fig. 80.27).
The arthroscope may then be placed through the anterosuperior cannula,
and both anterior and posterior drawer tests can be performed (Fig. 80.28).![]() Figure 80.27. Arthroscopic anterior drawer maneuver for assessing the grade of instability.
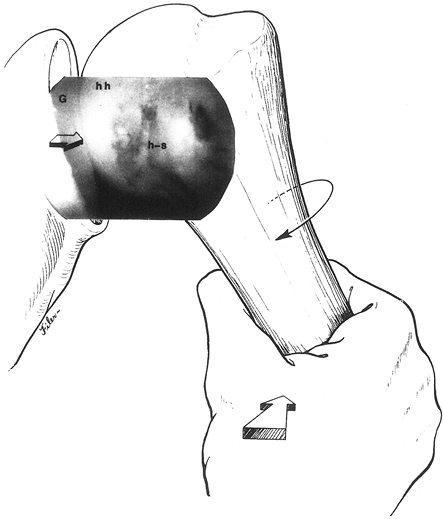
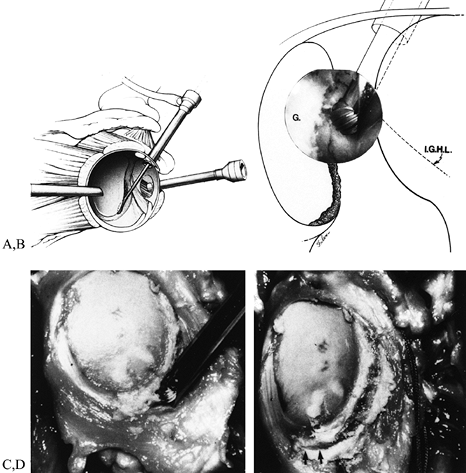
Figure 80.27. Arthroscopic anterior drawer maneuver for assessing the grade of instability.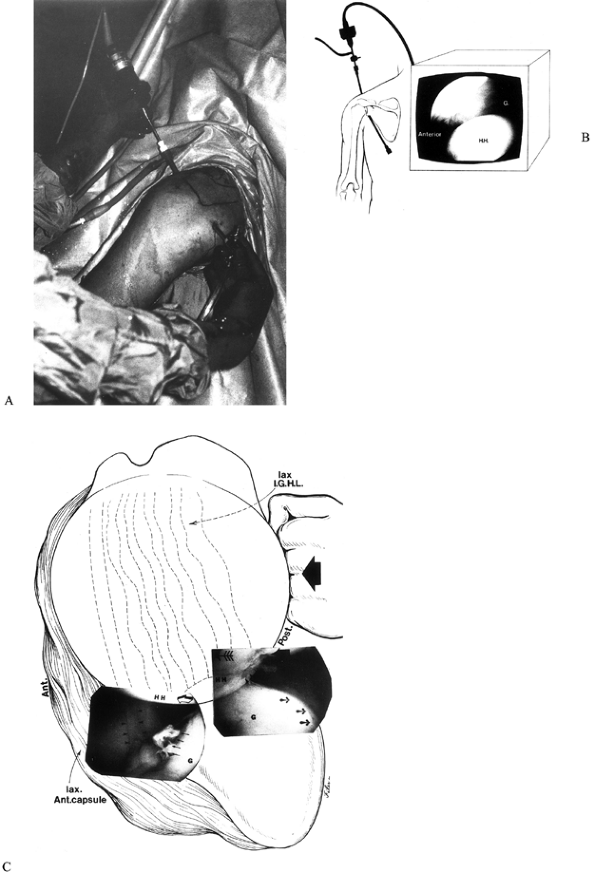 Figure 80.28. A:
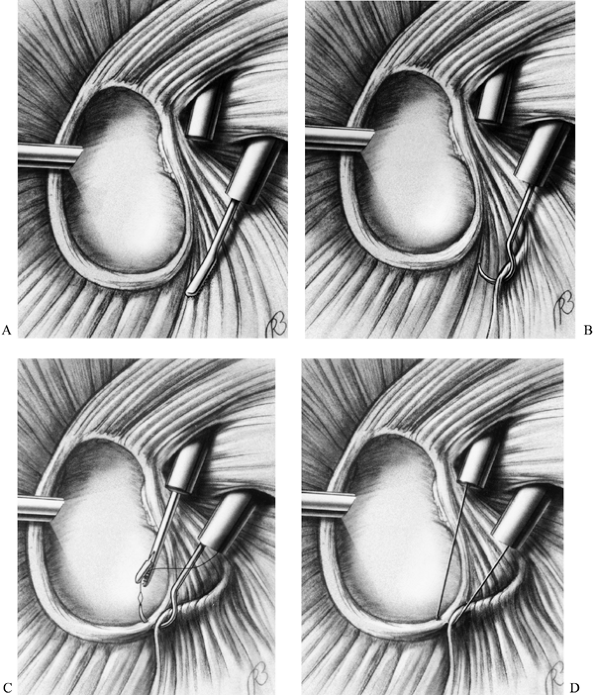
Figure 80.28. A:
Arthroscopic visualization can be performed anteriorly and is an
excellent means of evaluating the anterior glenoid rim and labrum. B: View the humeral head from an anterosuperior perspective. C: Viewing through this same portal, apply an anterior drawer test (broad arrow), and assess the degree of humeral head (HH) instability. Notice the thin, lax anterior band (thin arrows) of the IGHL
and the associated Hill–Sachs lesion (posterior humeral head). (From
Swenson TM, Warner JJP. Arthroscopic Shoulder Stabilization: Overview
of Indications, Technique, and Efficacy. Clin Sports Med 1995;14:841, with permission.) -
The examination should also focus on the quality and development of the glenohumeral ligaments (Fig. 80.29).
There is typically great variation among the three glenohumeral
ligaments. This development has been characterized on the basis of a
0–3+ scale (118). Zero represents absence of
the ligament, while 1+ means that the ligament is thin and lax in
nature or one-third the size of the biceps tendon. If the ligament is
thick and robust in nature or one-half the size of the biceps tendon,
it is graded as 2+, while 3+ means that the ligament is two-thirds the
size of the biceps tendon or greater (168). We
have found that individuals with marked laxity on drawer testing tend
to have small or damaged glenohumeral ligaments compared with those who
do not have marked laxity on drawer testing (Fig. 80.30) (170).
We believe that thicker, more robust–appearing glenohumeral ligaments
indicate a patient who is ideally suited for arthroscopic repair of a
Bankart lesion. Optimal selection criteria for an arthroscopic versus
an open stabilization procedure are provided in Table 80.4.![]() Figure 80.30. Assess the degree of injury to the ligamentous structures, as well. A: A ruptured IGHL is visualized and probed. B: Debridement is performed for better visualization. (From Warner JJP. Arthroscopic Bankart Repair. In: Bigliani LU, ed. Shoulder Instability. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1996:47, with permission.)
Figure 80.30. Assess the degree of injury to the ligamentous structures, as well. A: A ruptured IGHL is visualized and probed. B: Debridement is performed for better visualization. (From Warner JJP. Arthroscopic Bankart Repair. In: Bigliani LU, ed. Shoulder Instability. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1996:47, with permission.)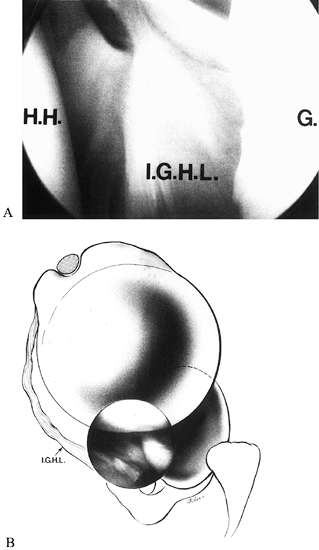 Figure 80.29.
Figure 80.29.
It is important to assess the size and quality of the IGHL. Compare its
size to the biceps tendon, which has a consistent diameter and
presence. A: Thin, mobile IGHL. B:
An anterior view further demonstrates the laxity associated with this
ligament. (From Warner JJP, Altchek DW. Arthroscopic Repairs for
Instability. In: Warner JJP, Iannotti JP, Gerber C, eds. Complex and Revision Problems in Shoulder Surgery. Philadelphia: Lippincott–Raven Publishers, 1997:26, with permission.)![]() Table 80.4. Patient Selection Criteria for Arthroscopic versus Open Shoulder Stabilization Procedures
Table 80.4. Patient Selection Criteria for Arthroscopic versus Open Shoulder Stabilization Procedures -
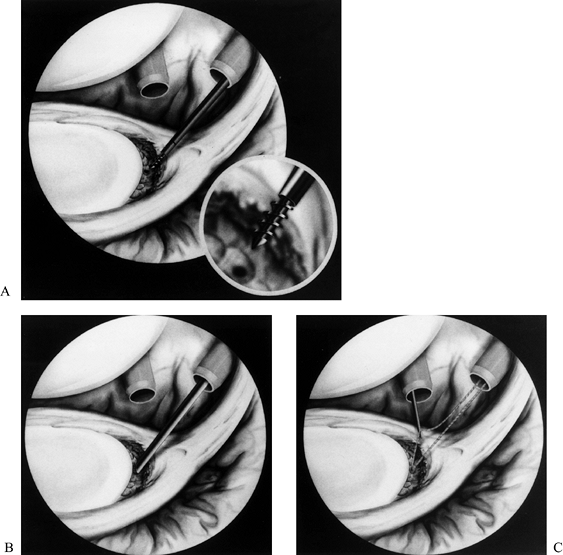
If the patient is deemed to be a suitable
candidate for arthroscopic Bankart repair, an anteroinferior portal
will be required for the placement of anchors and for knot-tying.
Locate this portal with the patient’s arm adducted at the side. Place
it approximately 1 cm inferior and lateral to the coracoid process(Fig. 80.25). With the arm is in this position, thereis little risk of injury to the musculocutaneous nerve(5,6). -
Place a spinal needle from outside into
the joint; its orientation should be just over the upper border of the
subscapularis tendon. Because the arm is adducted, this tendon falls
inferior to the equator of the glenoid, and access to the 4- to 5-o’
clock position along the glenoid rim is possible. Remove the needle,
and create the portal using a #11 blade. Place an 8 mm disposable
cannula with a flow-restricting diaphragm in this portal to allow room
for passage of the appropriate instrumentation (Fig. 80.31).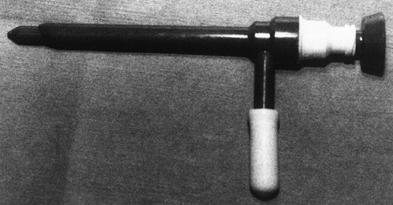 Figure 80.31.
Figure 80.31.
This disposable cannula with a diaphragm maintains joint distention and
contains an additional inflow–outflow portal. (From Warner JJP.
Shoulder Arthroscopy in the Beach-chair Position: Basic Setup. Oper Tech Orthop 1991;1:147, with permission.)
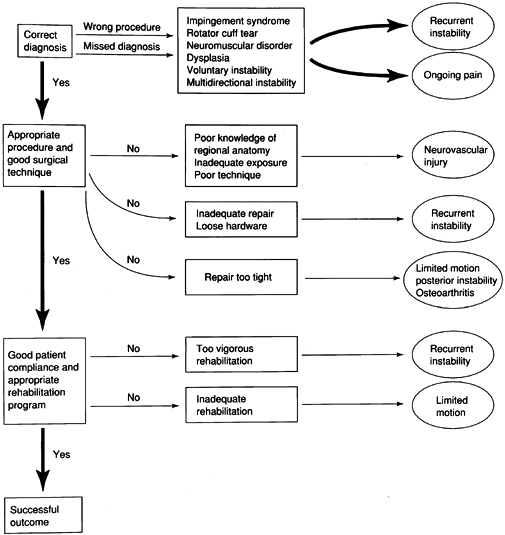
there are many errant courses that result in ineffective treatment. A
patient or a physician can make these errors. A successful outcome
begins with an accurate diagnosis followed by the specific treatment
required for that particular patient.
 |
|
Figure 80.32.
Successful treatment requires a correct preoperative diagnosis and performance of an appropriate procedure with excellent technique followed by a good postoperative rehabilitation protocol. An error at any step will result in a poor clinical outcome. (From Warner JJP. Overview: Avoiding Pitfalls and Managing Complications and Failures of Instability Surgery. In: Warner JJP, Iannotti JP, Gerber C, eds. Complex and Revision Problems in Shoulder Surgery. Philadelphia: Lippincott–Raven Publishers, 1997:7, with permission.) |
instability demonstrate a high rate of recurrence with nonoperative
treatment (21). Rowe and Sakellarides (133)
reported a recurrence rate of 58% in 398 patients with 53% follow-up.
They noted a strong correlation between patient age and recurrence,
with an incidence of recurrence of 94% in patients younger than 20
years, 79% in patients between 20 and 40 years, and 14% in patients
older than 40 years. Subsequent studies verified this trend (62,69,103). A large Scandinavian study suggested that recurrence was less common in young males. Hovelius et al. (70)
reported on 10-year follow-up of 245 patients with 247 primary
dislocations. Recurrent dislocation requiring surgery occurred in 34%
of 99 shoulders in the 12–22-year age range, 28% of 57 shoulders in the
23–29-year age range, and 9% of 91 shoulders in the 30–40-year age
range. Recurrence rates are even higher in the pediatric age group.
Marans et al. (93) reported one or more recurrent episodes of dislocation in all of the children in their study.
in 1948 that immobilization in full internal rotation for 4 weeks
produced complete stability, others have not reported such successful
outcomes. In fact, the success of immobilization has been variable.
Rowe and Sakellarides (133) reported that immobilization for 3 weeks decreased the recurrence rate. Henry and Genung (67) reported no significant improvement with immobilization. Aronen and Regan (6b)
found a reduction in the recurrence rate to 25% if first-time
dislocations were treated with isometric, isotonic, and isokinetic
exercises (7). Burkhead and Rockwood (21)
prescribed a shoulder exercise program for patients with a traumatic or
atraumatic etiology. In the traumatic subluxation group, 16% responded
favorably to a rehabilitation program, while 87% of the atraumatic
subluxation group without psychological problems demonstrated a
good-to-excellent outcome. Hovelius et al. (70) reported that the type and duration of initial treatment had no effect on the rate of recurrence.
determining recurrence of instability after a traumatic injury are age
and activity level. The following discussion considers surgical options
in this category of patients.
originally described five variations in labral anatomy; more recently,
however, Detrisac (personal communication) changed the categories to
two basic types. Type A labra were attached centrally and peripherally
at the inferior, posterior, and anterior regions, but superiorly they
were detached centrally and peripherally. In contrast, type B labra
were attached centrally and peripherally along the entire labrum.
performed shoulder dissections, modified this description. They
described an inferior labrum that consistently was triangular in shape
and attached centrally and peripherally. A similar shape was
demonstrated in the posterior labrum, although occasionally the
undersurface of this area was not attached. The superior region once
again showed consistent attachment peripherally, with a central portion
that was free in varying degrees. The anterior labrum was attached at
both the central and peripheral regions, appearing as a thickened band
of capsule that was clearly distinguishable on histologic and gross
assessment.
Flap tears are usually found in the anterosuperior, anteroinferior, or
inferior labrum (146), associated with
subluxation or frank dislocation. Other labral tears that have been
described include bucket-handle and incomplete split tears, which have
not necessarily been associated with instability, if located superiorly
(120). Degenerative tears are labral lesions that coexist with degenerative joint disease.
later reports demonstrated a clear relationship between instability and
labral pathology. In each study, despite early favorable results at 1-
and 2-year follow-up, there was significant deterioration in clinical
outcome. The authors in each article concluded that athletes whose
sports involve overhead activity should be treated as if there is some
underlying laxity or instability. Mere debridement of the labral
pathology cannot be expected to be successful.
Center further strengthened these recommendations (35).
The majority of these patients had SLAP lesions, while the remainder
had either anteroinferior or posterior labral lesions. While no patient
had a history of dislocation or clinically evident instability
preoperatively, EUA revealed instability in 70% of patients with SLAP
lesions and in all of the other patients.
versus 30% of the anteroinferior group had excellent results from
debridement. These results deteriorated with time to 63% and 25% in
each respective group at 2-year follow-up. The authors concluded that
instability was frequently present in patients with labral pathology,
and debridement would provide only short-term relief in this patient
population. On the basis of these studies it is difficult to recommend
labral debridement for most patients.
reported the association in athletes between throwing and injuries to
the anterosuperior glenoid labrum and the insertion of the long head of
the biceps brachii. These injuries were believed attributable to the
large deceleration forces applied by the biceps muscle at the insertion
point. Two studies further implicated the long head of the biceps in
contributing to anterior and superior shoulder stability during
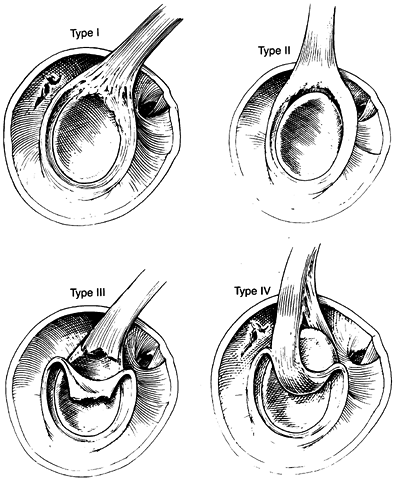
abduction and external rotation (126,174). In 1990, Snyder et al. (145)
retrospectively reviewed 700 patients who underwent shoulder
arthroscopy and described four specific types of pathologic
abnormalities in this area: the SLAP lesions (Fig. 80.33). A description of each type of SLAP lesion and the recommended treatment is provided in Table 80.5.
 |
|
Figure 80.33. The four types of SLAP lesions (Table 80.5).
(From Snyder SJ, Wuh HCK. Arthroscopic Evaluation and Treatment of the Rotator Cuff Superior Labrum Anterior Posterior Lesion. Oper Tech Orthop 1991;1:212, with permission.) |
 |
|
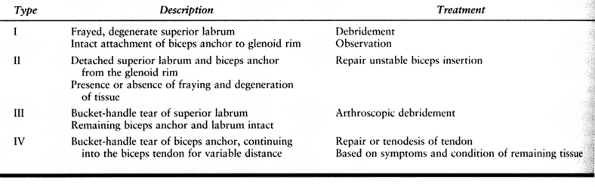
Table 80.5. SLAP Lesion Types and Appropriate Treatments
|
These studies demonstrated a relative avascularity at the superior and
anterosuperior regions compared with the posterior and inferior
regions, and this may be one reason for the degeneration that occurs in
this area. A retrospective review by Snyder et al. (144)
involving 2,375 arthroscopic shoulder procedures over 8 years found
SLAP lesions in 140 (6%) patients. Most lesions were classified as
either type II (55%) or type I (21%) lesions. Only 28% had isolated
superior
labral
pathology, 22% had associated Bankart lesions, and the remainder had
associated rotator cuff pathology. Another review of 712 patients
revealed that 17% had type I lesions, while 11.8% had other significant
labral pathology (91).
The authors had difficulty classifying the remaining pathology
according to the criteria described by Snyder, but once again there was
a high association between labral lesions and subtle instability or
laxity on EUA.
superior-labral and biceps-insertion pathology has led to the
development of several arthroscopic repair techniques. In 1991, Yoneda
et al. (184) described the use of an
arthroscopic staple (Instrument Makar Inc., Okemos, MI) designed by
Lanny Johnson. The patient population consisted of 10 young athletes
(involved in overhead sports) with type II SLAP lesions. The standard
lateral decubitus position was used, and the joint was visualized
through the standard posterior portal. An anterosuperior portal was
used for instrumentation.
and stapling of the SLAP area. One staple (5.5 mm diameter) was used in
each case. Patients were immobilized for 2–3 weeks; range of motion was
then initiated, followed by strengthening exercises at 6 weeks. Because
of concerns over staple migration and irritation, all staples were
removed at an average of 3.9 months. On second-look arthroscopy,
complete healing had occurred in four patients, with full continuity
with the glenoid surface. The remaining repairs were deemed stable
despite incomplete healing. More important, 80% of patients were found
to have good-to-excellent results.
A transglenoid approach, originally developed for Bankart lesions and
popularized by Caspari, has been applied to the SLAP lesion (24,44).
-
With the patient in the lateral decubitus
position, use standard posterior and superior portals for visualization
and inflow. Establish a third anterior portal with a spinal needle;
this portal will be used for instrumentation. -
Use a Caspari suture punch (Concept Inc.,
Largo, FL) through the anterior portal to place four to seven 2-0
polydioxanone (PDS) sutures from posterior to anterior along the
labrum–biceps tendon complex. Place an additional one to two 0-PDS
sutures into the biceps tendon, as well, to reinforce the repair. -
Make a transglenoid drill hole (1-o’
clock position for right shoulders or 11-o’ clock position for left
shoulders), using a Beath needle placed through the anterior portal
approximately 3–5 mm medial to the articular surface and exiting in the
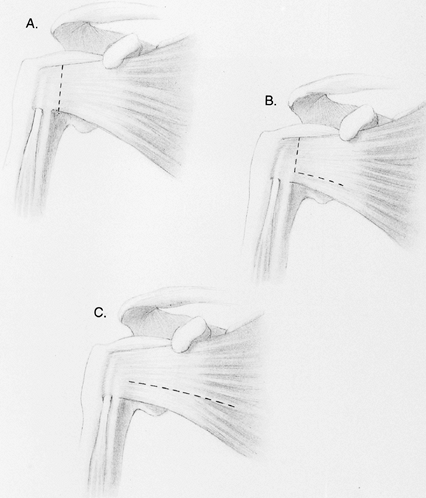
infraspinatus fossa posteriorly (Fig. 80.34A, Fig. 80.34B). Then pass all previously placed sutures through the glenoid neck, using the Beath needle (Fig. 80.34C). Tie the sutures through a small posterior incision over the infraspinatus fascia (Fig. 80.34D). Immobilize the patient for 1–2 weeks, and protect the shoulder in a sling for an additional 3–4 weeks. Field and Savoie (44) reported excellent results in 80% of the patients in whom they used this technique.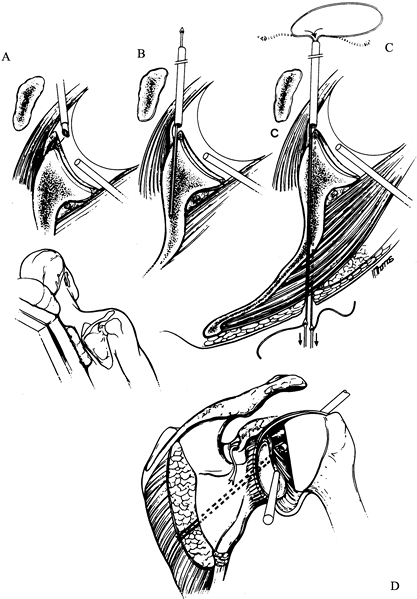 Figure 80.34. Arthroscopic repair of a SLAP lesion using a transglenoid suture technique. A: Prepare the glenoid rim. B: Drill transglenoidally with a Beath needle. C:
Figure 80.34. Arthroscopic repair of a SLAP lesion using a transglenoid suture technique. A: Prepare the glenoid rim. B: Drill transglenoidally with a Beath needle. C:
Pass the suture that is subsequently tied over the infraspinatus
fascia. (From Altchek DW, Warren RF, Skyhar MJ. Shoulder Arthroscopy.
In: Rockwood CA Jr, Matsen FA III, eds. The Shoulder. Philadelphia: WB Saunders, 1990:275, with permission.)
because it requires a separate posterior incision to tie the sutures.
Tying over the infraspinatus muscle may lead to gaps at the repair site
if muscle atrophy occurs. Further, the elastic nature of PDS suture
makes it
prone to gap 5–10 mm at the repair site (52). In addition, during transosseous pin placement, there is a risk of injury to the suprascapular nerve or one of its branches (140).
The standard posterior, anterosuperior, and anteroinferior portals as
previously described are used with this technique. Wichman and Snyder (180) described the more inferior portal as the anterior mid-glenoid portal.
-
Place disposable cannulas with
flow-restricting diaphragms into each anterior portal. For type II
lesions, first use a shaver to debride the fibrous membrane over the
glenoid neck. Then use a 4.0 mm ball-shaped burr to decorticate and
create a notch beneath the SLAP region, avoiding the articular
cartilage. SCOI recommends the use of the Revo screw system (Linvatec,
Inc. Largo, FL), in which nonabsorbable suture is placed through the
eyelet of the screw before implantation. Insert the Revo punch through
the anterosuperior cannula at a 45° angle, impact it with a mallet, and
remove it. Then place the screw with the attached braided,
nonabsorbable suture (Fig. 80.35A, Fig. 80.35B).![]() Figure 80.35. SLAP lesion repair. A: Place a suture anchor into the prepared glenoid rim, using the anterosuperior arthroscopic portal. B: Firmly seat the anchor in the bone. C:
Figure 80.35. SLAP lesion repair. A: Place a suture anchor into the prepared glenoid rim, using the anterosuperior arthroscopic portal. B: Firmly seat the anchor in the bone. C:
Pass one limb of the suture through the anteroinferior portal. (From
Cheng JC, Karzel RP. Superior Labrum Anterior Posterior Lesions of the
Shoulder: Operative Techniques of Management. Oper Tech Sports Med 1997;5:249, with permission.) -
Apply tension to the suture through the
cannula to assess the stability of the anchor. Then use a hook or
grasper to retrieve one limb of the suture through the anteroinferior
cannula (Fig. 80.35C). Place a crescent-shaped
suture passer through the anterosuperior portal, and use it to pass a
Shuttle Relay (Linvatec, Inc., Largo, FL) through the anterior superior
labrum–biceps complex
P.2169
(Fig. 80.36A). The Shuttle Relay contains a central loop through which suture can be placed and then pulled back through the tissue.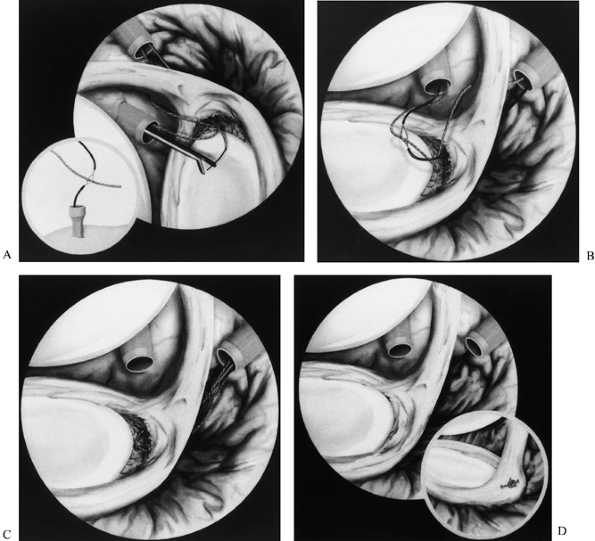 Figure 80.36. SLAP lesion repair. A:
Figure 80.36. SLAP lesion repair. A:
Place a cannulated hook and Shuttle Relay through the SLAP lesion. Then
expose the latter externally through the anteroinferior portal. Pass
the suture through the eyelet portion of the Shuttle Relay. B: Pull the suture in a retrograde fashion through the SLAP lesion and the anterosuperior cannula. C: Repeat the process for the other limb. D:
Tie the suture arthroscopically, creating a horizontal configuration.
(From Cheng JC, Karzel RP. Superior Labrum Anterior Posterior Lesions
of the Shoulder: Operative Techniques of Management. Oper Tech Sports Med 1997;5:249, with permission.) -
Pass the Shuttle Relay through the
anteroinferior portal with a grasper, and expose the loop externally.
Pass the limb of nonabsorbable suture in the anteroinferior portal
through the loop of the relay. Then pass the suture through the tissue
by applying tension on the other end of the Shuttle Relay still exposed
through the anterosuperior portal (Fig. 80.36B).
Thus, the relay and attached suture are pulled back through the tissue
and out the anterosuperior cannula in a retrograde fashion. -
Repeat the process for the other limb of
the suture, creating a horizontal mattress repair. Place a probe
through the anteroinferior portal to reduce the entire complex, and use
an arthroscopic knot pusher to tie the suture in place (Fig. 80.36C, Fig. 80.36D). -
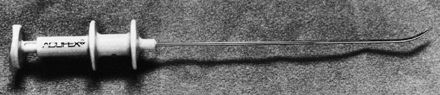
An alternative to the Shuttle Relay is a suture-transport system (Smith and Nephew, Andover, MA) (Fig. 80.37). These instruments contain a sharp tip that is passed through the anterosuperior portal and directly through the tissue (Fig. 80.38A).
The surgeon deploys two small metal arms and grasps one limb of the
suture, pulling it back through the tissue and out the cannula (Fig. 80.38B). The process is repeated, and the sutures are tied in horizontal fashion.![]() Figure 80.37.
Figure 80.37.
Suture-transport system (Acufex). (From Cheng JC, Karzel RP. Superior
Labrum Anterior Posterior Lesions of the Shoulder: Operative Techniques
of Management. Oper Tech Sports Med 1997;5:249, with permission.)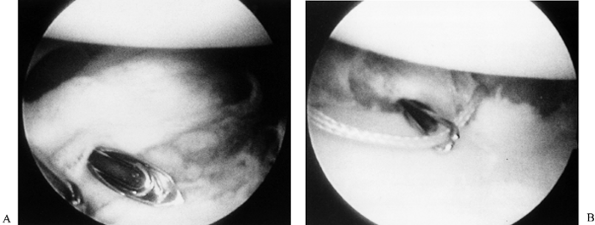 Figure 80.38. SLAP lesion repair. A: Pass the transport system through the labral tissue. B:
Figure 80.38. SLAP lesion repair. A: Pass the transport system through the labral tissue. B:
Deploy the central arms, and grasp the suture; then pass the suture
back through the tissue, and tie it for an effective repair. (From
Cheng JC, Karzel RP. Superior Labrum Anterior Posterior Lesions of the
Shoulder: Operative Techniques of Management. Oper Tech Sports Med 1997;5:249, with permission.) -
In type IV lesions, for tears involving
less than 30% of the torn biceps tendon, perform debridement and
complete repair as for type II lesions. With greater involvement,
perform a primary biceps tenodesis in elderly patients or a suture
repair of the biceps tendon and labrum in younger patients.
Good-to-excellent results with this technique have been reported in 74%
of patients after long-term follow-up (153).
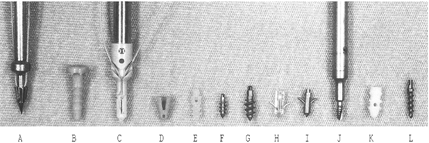
Many surgeons prefer to use metal anchors for postoperative
radiographic visualization in the event that an anchor dislodges from
the bone, which is a potential risk with this technique. If an anchor
loosens, the device must be removed because an intraarticular loose
body could lead to cartilage damage. In addition, there are potentially
grave complications from migration of a foreign object to the lung,
subclavian artery, or spinal canal (90,96,98,111,138).
 |
|
Figure 80.39. Some suture anchors currently on the market. A: Arthrotek Harpoon Suture Anchor, Warsaw, IN. B: Acufex Suretac II, Andover, MA. C: Innovasive Devices Roc, Marlborough, MA. D: Acufex Tag Wedge, Andover, MA. E: Linvatec Bio-Anchor, Largo, FL. F: Linvatec Mini-Revo, Largo, FL. G: Linvatec Revo, Largo, FL. H: Mitek Stealth, Westwood, MA. I: Mitek G-II Anchor, Westwood, MA. J: Zimmer Statak. K: Acufex Tag Rd II, Andover, MA. L: Arthrex Fastak, Naples, FL. (From Elrod B. Arthroscopic Reconstruction of Traumatic Anterior Instability. Oper Tech Sports Med 1997;5:215, with permission.)
|
developed. However, because they degrade, they raise concerns about the
stability of the repair. Studies have focused on initial pullout
strengths and degradation of the entire anchor (8,9,97). As most absorbable materi-als lose their strength in 4–6 weeks, there are also concerns
over the degradation at the eyelet (20).
This technique also requires secure intraarticular knot-tying with a
certain level of experience before actual use in the operating room.
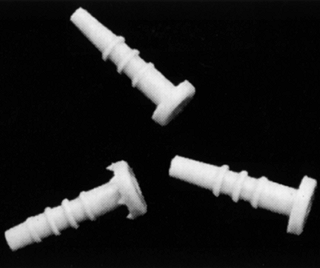
(Smith and Nephew, Andover, MA) to overcome some of the problems
inherent in suture anchors (151,177).
This implant is an absorbable, cannulated device composed of a
synthetic copolymer (polyglyconate). The tack contains ribs for
increased pullout strength (3.2 mm shaft diameter). It has a wide, flat
head (6.5 mm diameter) to adequately hold tissues, and undergoes
hydrolysis, thereby preventing a significant inflammatory response (Fig. 80.40).
The rapid, 4-week bioabsorption profile prevents the possibility of
loose fragments, as might occur with slower absorption profiles, but is
considered long enough for adequate tissue healing. In most
descriptions of procedures employing this implant, the beach-chair
position has been used (117,172).
 |
|
Figure 80.40. Suretac implants.
|
challenge to repair, but they are much more easily repaired through an
arthroscopic than through an open approach because the overlying
acromion makes exposure of the superior glenoid difficult through a
deltopectoral approach. Furthermore, the diagnosis of a SLAP lesion is
essentially an arthroscopic diagnosis.
In the past 2 years, a suture method has been developed. Both methods
have proven efficacious. Theoretically, the suture method gives
stronger immediate repair without any worry about deterioration of the
strength of repair due to resorption of the polyglyconate anchor, as
with the Suretac device.
-
Perform both techniques with the patient
in a beach-chair position. Use an anterosuperior portal with a 6 mm
cannula with a flow-restricting diaphragm entering the joint just
underneath the biceps tendon. Use an accessory anterolateral or
transcuff portal, as well (Fig. 80.41).![]() Figure 80.41.
Figure 80.41.
SLAP lesion repair. The superior portal provides direct access to the
superior labral area, but the surrounding soft tissues prevent adequate
visualization and manipulation of lesion. There is also an increased
possibility of drill slippage with resultant articular cartilage
damage. Use of the lateral portal provides equal access and avoids
these problems. (From Warner JJ, Kann S, Marks P. Arthroscopic Repair
of Combined Bankart and Superior Labral Detachment Anterior and
Posterior Lesions: Technique and Preliminary Results. Arthroscopy 1994;10:383, with permission.) -
Place an 18-gauge spinal needle through
the rotator cuff from just lateral to the acromion to identify this
latter portal. Position the needle so that the most direct angle to the
superior labrum is possible. Then withdraw the spinal needle and use a
#11 blade to make a portal through the rotator cuff while visualizing
from within the joint. Insert another 6 mm cannula into the joint
P.2172
through
the rotator cuff. The defect made in the cuff with this approach has
not led to any significant clinical problems postoperatively. -
Using the anterosuperior portal, clear the superior glenoid rim of soft tissue, using a motorized shaver (Fig. 80.42), and decorticate the juxtaarticular margin with a burr (Fig. 80.43).
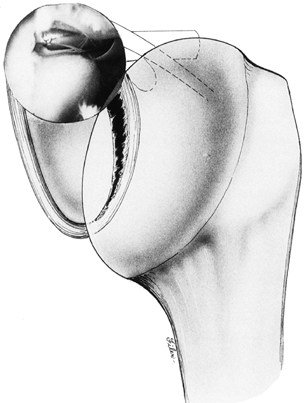 Figure 80.42.
Figure 80.42.
SLAP lesion repair. Arthroscopic debridement of the superior and
anterior labral areas can be performed through the anterosuperior
portal. (From Warner JJ, Kann S, Marks P. Arthroscopic Repair of
Combined Bankart and Superior Labral Detachment Anterior and Posterior
Lesions: Technique and Preliminary Results. Arthroscopy 1994;10:383, with permission.)![]() Figure 80.43. SLAP lesion repair. The lateral portal provides direct access to the superior aspect of the glenoid for preparation (A) for and placement (B)
Figure 80.43. SLAP lesion repair. The lateral portal provides direct access to the superior aspect of the glenoid for preparation (A) for and placement (B)
of the Suretac device. (From Warner JJ, Kann S, Marks P. Arthroscopic
Repair of Combined Bankart and Superior Labral Detachment Anterior and
Posterior Lesions: Technique and Preliminary Results. Arthroscopy 1994;10:383, with permission.) -
Repair the SLAP lesion through the
transcuff portal, using either one Suretac implant placed through the
labrum–biceps tendon complex or two suture anchors placed just anterior
and posterior to the biceps origin. When using the Suretac implant,
place a cannulated drill with protruding guidewire (3 mm) through the
transcuff portal (Fig. 80.44). The wire, which is locked in position, pierces the tissue and is used to bring the complex toward the prepared glenoid neck.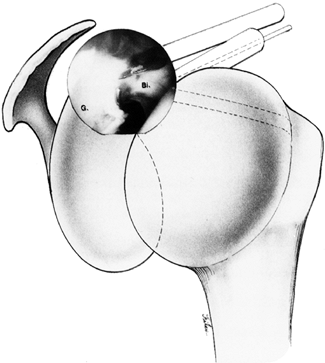 Figure 80.44. Arthroscopic view of a type II SLAP lesion. An anterosuperior portal allows manipulation of the biceps (Bi) and preparation of the glenoid (G),
Figure 80.44. Arthroscopic view of a type II SLAP lesion. An anterosuperior portal allows manipulation of the biceps (Bi) and preparation of the glenoid (G),
while the lateral portal allows placement of the guidewire and drill.
(From Warner JJ, Kann S, Marks P. Arthroscopic Repair of Combined
Bankart and Superior Labral Detachment Anterior and Posterior Lesions:
Technique and Preliminary Results. Arthroscopy 1994;10:383, with permission.) -
Advance the drill to a depth of one
external mark (approximately 1–2 cm), and unlock the wire from the bit.
Tap at its free end to release it from the drill, and remove the drill.
The wire should remain in place, piercing the tissue. Place the tack
over the wire, and tamp it into place with a cannulated pusher.
Technical errors encountered with the Suretac device will be discussed
later in the chapter. Clinical and cadaveric experience have
demonstrated that the accessory anterolateral portal (localized with a
spinal needle) can provide reliable access to the superior glenoid
region (Fig. 80.46).
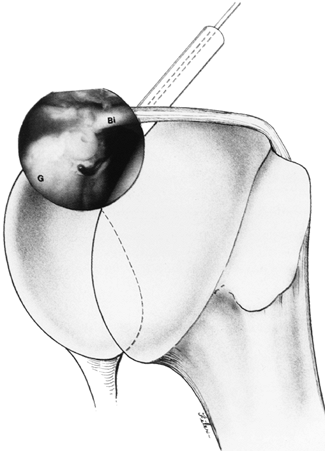 |
|
Figure 80.45.
Arthroscopic stabilization of a type II SLAP lesion with a Suretac implant. (From Warner JJ, Kann S, Marks P. Arthroscopic Repair of Combined Bankart and Superior Labral Detachment Anterior and Posterior Lesions: Technique and Preliminary Results. Arthroscopy 1994;10:383, with permission.) |
 |
|
Figure 80.46.
This cadaveric dissection demonstrates the direct localization of the superior glenoid and SLAP repair from a lateral direction. (From Warner JJ, Kann S, Marks P. Arthroscopic Repair of Combined Bankart and Superior Labral Detachment Anterior and Posterior Lesions: Technique and Preliminary Results. Arthroscopy 1994;10:383, with permission.) |
Initiate gentle passive range-of-motion exercises in a supervised
setting 1 week postoperatively. Advise patients to avoid external
rotation past neutral and forceful abduction greater than 60° for 4
weeks. With this technique,
86%
satisfactory results were obtained at 2-year follow-up. Twelve of 13
athletes were able to return to full overhead function (117).
-
Use the anterosuperior portal for glenoid
preparation and the transcuff portal for implant placement. Assess and
prepare the area beneath the labrum–biceps tendon complex as described
previously (Fig. 80.47A, Fig. 80.47B).
Place suture anchors anterior and posterior to the complex. We have had
experience with the Tag Rd II (Smith and Nephew, Andover, MA) and the
ROC (Innovasive Devices, Inc., Marlborough, MA) suture anchor systems.
As stated previously, there are many suture anchors on the market, each
with its own advantages and disadvantages.![]() Figure 80.47. Slap lesion repair. A: Prepare the superior labral region through the lateral portal, using a shaver. B: Use an arthroscopic burr to create a bleeding surface. C: Place the arthroscopic drill through the lateral portal. D: Implant a suture anchor after drilling has been performed.
Figure 80.47. Slap lesion repair. A: Prepare the superior labral region through the lateral portal, using a shaver. B: Use an arthroscopic burr to create a bleeding surface. C: Place the arthroscopic drill through the lateral portal. D: Implant a suture anchor after drilling has been performed. -
Regardless of the system used, drill the glenoid neck at a 45° angle from the articular surface through the transcuff portal (Fig. 80.47C). Remove the drill, and then tap the preloaded (braided, nonabsorbable material) suture anchor into place (Fig. 80.47D).
Apply firm tension on the suture to assess fixation. Use either a
Shuttle Relay or a suture-transport system to pass one limb of the
suture through the biceps tendon, as previously described, using the
anterosuperior portal (Fig. 80.48A).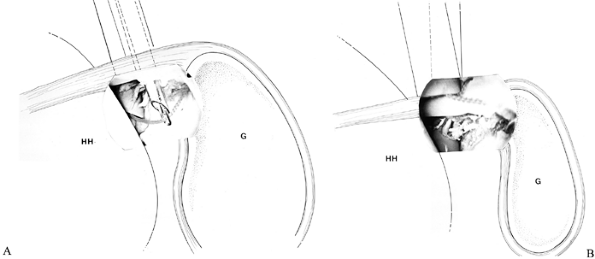 Figure 80.48. Slap lesion repair. A:
Figure 80.48. Slap lesion repair. A:
One arthroscopic knot has been tied anteriorly. Use a suture-transport
system to pass an additional suture through the posterior portion of
the SLAP lesion, using the lateral portal. -
Using arthroscopic knot-tying technique,
fix the biceps anchor to the glenoid rim with a simple (not horizontal
mattress) suture configuration (Fig. 80.48B).
Assess the repair for stability at this point, and, if deemed
necessary, place another suture anchor either anterior or posterior to
the initial suture anchor for additional fixation. -
Use the same postoperative protocol as for the Suretac repair.
satisfying, although longer follow-up will be required to determine its
true clinical efficacy.
repairs were adapted from techniques for arthroscopic repair of Bankart
lesions. Arthroscopic shoulder stabilization was initially attempted
with an arthroscopic staple (79).
Unfortunately, this technique was associated with a high recurrence
rate and an unacceptably high rate of complications related to the
implant (Table 80.6). Complications included
breakage and migration of the staple, as well as articular and
neurovascular injuries from the staple. This technique has largely been
abandoned.
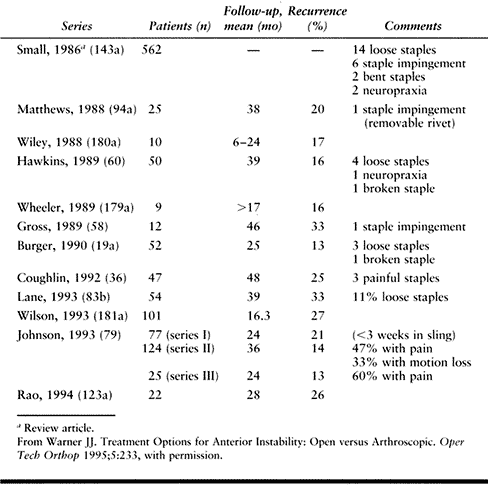 |
|
Table 80.6. Published Complications and Instability Recurrence Rates of the Arthroscopic Staple Technique
|
transosseous suture repair technique that avoided the pitfalls of a
juxtaarticular staple (24a,104,136). This method was based on the open technique developed by Reider and Ingles (166).
In a manner similar to that previously described for SLAP lesion
repairs, a Caspari suture punch is used to place PDS sutures through
the IGHL. These sutures are then loaded onto a special pin with a hole
at one end (Beath pin) and passed through a drill hole made at the
anterior glenoid rim so that it exits out of the infraspinatus fossa (Fig. 80.34). These sutures are then separated into two limbs and tied over the infraspinatus fascia.
of repair, results have been good to excellent over intermediate
follow-up (157). Unfortunately, others have
been unable to duplicate the success of these surgeons, and with longer
follow-up, recurrence rates have beenreported in the 20% to 40% range (Table 80.7) (58,127,140,162,165).
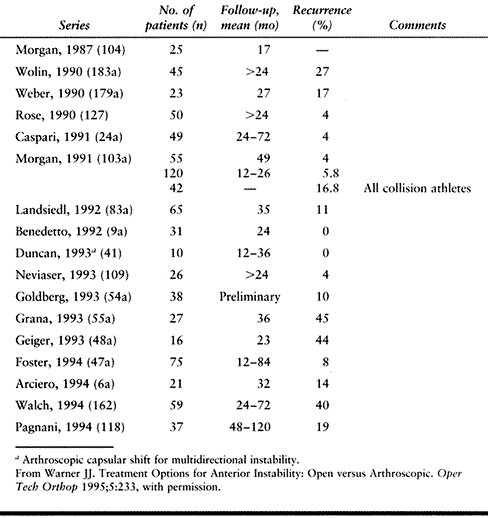 |
|
Table 80.7. Published Instability Recurrence Rates of the Arthroscopic Suture Technique
|
associated with this technique, such as placement of the drill hole too
medially so that the Bankart lesion is not repaired, as well as
suprascapular nerve injury from posterior exit of the pin. Finally, the
need for an additional posterior incision has made this approach less
desirable.
technique was made by Maki (92).
He proposed drilling across the glenoid in a manner similar to the
technique described above; however, a large suture (Mulberry knot) was
tied in the PDS suture so that when it was pulled back it locked on the
posterior cortex of the scapula. Internal knots were then tied over the
anterior capsule and labrum with a special knot pusher and special
knot-tying techniques. Current approaches to arthroscopic Bankart
repair involve the use of suture anchors and internal knots or
absorbable transfixing implants (42,127,183).
methods of repair are continuing to evolve, along with an appreciation
of more specific indications for their use. There are clear-cut
advantages and disadvantages to arthroscopic stabilization procedures (Table 80.8).
Appropriate patient selection is based on a detailed history and
physical examination, imaging studies when indicated, and a careful EUA
and arthroscopic inspection. In addition, other specific factors seem
to be associated with a good result (Table 80.4).
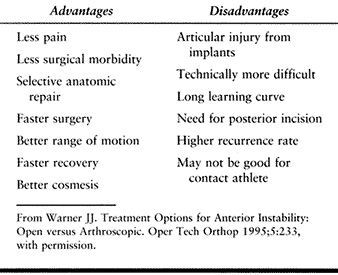 |
|
Table 80.8. Arthroscopic Bankart Repair
|
arthroscopic capsulorrhaphy and thermal capsular shrinkage for patients
with capsular laxity, we feel that the optimal patient for repair is
one who has a discrete Bankart lesion with robust capsuloligamentous
structures without significant capsular injury. In addition, it is
preferable if there is no significant glenoid erosion or a bony Bankart
lesion. While a small Hill–Sachs lesion is not a contraindication to
arthroscopic repair, we believe that a large Hill–Sachs lesion is
associated with recurrent episodes of dislocation and generally
indicates significant capsular laxity. With these criteria, short-term
follow-up studies have demonstrated a significant reduction to
approximately 7% to 10% in postoperative failure rates
(recurrences) after arthroscopic stabilization procedures (84,175,176).
-
Perform arthroscopy with the patient in the beach-chair position.
-
Use three portals for the arthroscopic Bankart repair: the standard posterior, anterosuperior, and anteroinferior portals (Fig. 80.49A).
Accurate portal placement is essential for proper technical execution
of the procedure. The anterosuperior and anteroinferior portals must
diverge so that intraarticular instrument crowding is not a problem.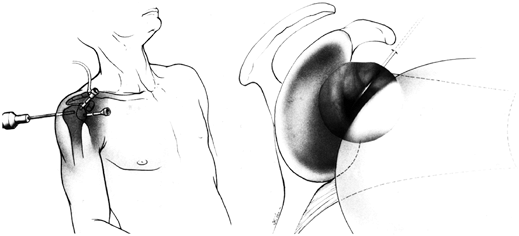 Figure 80.49. Arthroscopic Bankart repair. A: Use anterosuperior and anteroinferior portals for a standard repair. B:
Figure 80.49. Arthroscopic Bankart repair. A: Use anterosuperior and anteroinferior portals for a standard repair. B:
Use a spinal needle to localize the correct position for portal
placement. The location should allow access to the 4- and 5-o’clock
positions along the glenoid rim. This method is referred to as the
outside-in technique. (From Warner JJ, Warren RF. Arthroscopic Bankart
Repair Using a Cannulated, Absorbable Fixation Device. Oper Tech Orthop 1991;1:192, with permission.) -
As previously discussed, place the
anterosuperior portal just anterior and lateral to the
acromioclavicular joint, so that a 6 mm cannula enters the joint
vertically just beneath the biceps tendon. Locate the anteroinferior
portal 1 cm inferior and lateral to the coracoid process, entering the
joint just over the subscapularis tendon. Use a spinal needle before
incising the skin to ensure access to the appropriate region along the
anteroinferior glenoid neck (Fig. 80.49B). It
should correspond to the 4- and 5-o’ clock positions for the right
shoulder and to the 7- and 8-o’ clock positions for the left shoulder.
If this inferior portal is not placed correctly, there will be a
tendency for the drill to slip either medially or inferiorly when you
attempt fixation. Insert a large, 8 mm cannula through this portal to
allow placement of the appropriate instruments. -
As with SLAP lesions, adequately prepare
the glenoid neck to ensure healing of soft tissue to bone, including
the inferior glenoid rim, which usually requires enlargement of the
Bankart lesion (Fig. 80.50A). Gain access to
this region through the anteroinferior portal; use a motorized shaver
and burr to create a bony trough along the anterior glenoid neck that
prevents drill slippage during subsequent portions of the procedure (Fig. 80.50B, Fig. 80.50C and Fig. 80.50D).![]() Figure 80.50. Arthroscopic Bankart repair. A:
Figure 80.50. Arthroscopic Bankart repair. A:
The standard arthroscopic portals are depicted. Place an arthroscopic
rasp through the anterosuperior portal to prepare the glenoid rim.
(From Warner JJ, Warren RF. Arthroscopic Bankart Repair Using a
Cannulated, Absorbable Fixation Device. Oper Tech Orthop Surg 1991;1:192, with permission.) B: An arthroscopic burr has been placed through the anterosuperior portal. C: This cadaveric dissection demonstrates glenoid preparation with the burr. D:
Glenoid preparation has been performed up to the 5-o’clock position.
(From Warner JJ, Miller MD, Marks P. Arthroscopic Bankart Repair with
the Suretac Device. Part II. Experimental Observations. Arthroscopy 1995;11:14, with permission.) -
Use a 30° arthroscope placed through the posterior and anterosuperior portals to assess the preparation (Fig. 80.51).
P.2179
Alternatively, place a 70° arthroscope through the posterior portal to gain a bird’s-eye view of the anterior glenoid region.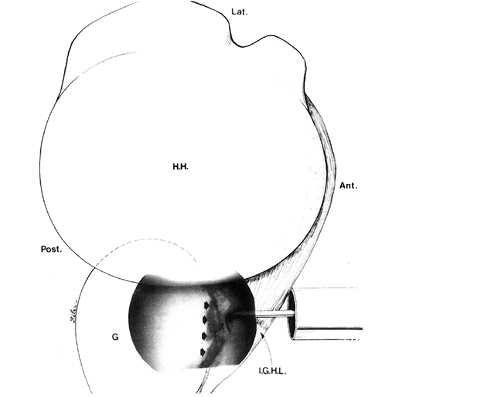 Figure 80.51. Arthroscopic view through the anterosuperior portal demonstrates displacement of the anterior band of the IGHL with a probe. The anterior glenoid rim has been decorticated before arthroscopic repair (arrows). (From Warner JJP, Altchek DW. Arthroscopic Repairs for Instability. In: Warner JJP, Iannotti JP, Gerber C, eds. Complex and Revision Problems in Shoulder Surgery. Philadelphia: Lippincott–Raven Publishers, 1997:34, with permission.)
Figure 80.51. Arthroscopic view through the anterosuperior portal demonstrates displacement of the anterior band of the IGHL with a probe. The anterior glenoid rim has been decorticated before arthroscopic repair (arrows). (From Warner JJP, Altchek DW. Arthroscopic Repairs for Instability. In: Warner JJP, Iannotti JP, Gerber C, eds. Complex and Revision Problems in Shoulder Surgery. Philadelphia: Lippincott–Raven Publishers, 1997:34, with permission.) -
In chronic instability, the detached capsulolabral complex may adhere by scar medially along the scapula. Neviaser (109) termed this an anterior labral periosteal sleeve avulsion
(ALPSA) injury. It is essential to mobilize this tissue so that it can
be reattached at its anatomic site adjacent to the articular margin of
the glenoid. Use a hooked-tip electrocautery device and a knife–rasp to
subperiosteally elevate the scarred capsulolabral tissue (Fig. 80.52A).![]() Figure 80.52. Arthroscopic Bankart repair. A: Place an arthroscopic instrument through the anterosuperior portal and grasp the anterior band of the IGHL (H.H., humeral head; G., glenoid). B: Pull the IGHL in a posterosuperior direction, using an arthroscopic grasper. C: This cadaveric dissection demonstrates a persistent Bankart lesion after inadequate mobilization of the IGHL. (arrows). D:
Figure 80.52. Arthroscopic Bankart repair. A: Place an arthroscopic instrument through the anterosuperior portal and grasp the anterior band of the IGHL (H.H., humeral head; G., glenoid). B: Pull the IGHL in a posterosuperior direction, using an arthroscopic grasper. C: This cadaveric dissection demonstrates a persistent Bankart lesion after inadequate mobilization of the IGHL. (arrows). D:
Appropriate superior shift of the anterior band of the IGHL avoids this
problem by bringing the soft tissues firmly against the anteroinferior
glenoid rim. (From Warner JJ, Miller MD, Marks P. Arthroscopic Bankart
Repair with the Suretac Device. Part II. Experimental Observations. Arthroscopy 1995;11:14, with permission.) -
Place an arthroscopic grasper through the
anterosuperior portal, and use it to pull the tissue into the
appropriate position before repair with the Suretac implant (Fig. 80.52B, Fig. 80.52C and Fig. 80.52D). Place this device, using the same technique described previously for SLAP lesion repairs. -
Postoperatively, protect patients in a
sling and swathe for 4 weeks. Allow them to shower, but they should
avoid external rotation; advise them to maintain the arm internally
rotated when it is out of the sling. Allow elbow motion, as well as
activities of daily living, which generally involve limited forward
flexion. After 4 weeks, allow active-assisted stretching and
strengthening exercises. Allow swimming and throwing at 4 months and
contact sports at 6 months.
device, we recently increased our use of suture anchors along the
anterior glenohumeral rim in patients with labral pathology and
associated capsular laxity or stretch.
-
With the patient in the beach-chair
position, create posterior, anterosuperior, and anteroinferior portals
as previously described. Once again, it is important to maintain
adequate distance between the two anterior portals to avoid instrument
crowding. A spinal needle is helpful in localizing the more inferior
portal (Fig. 80.53A). The anteroinferior portal
contains a large, 8.0 mm cannula to allow placement of the drill and
suture hook during the procedure.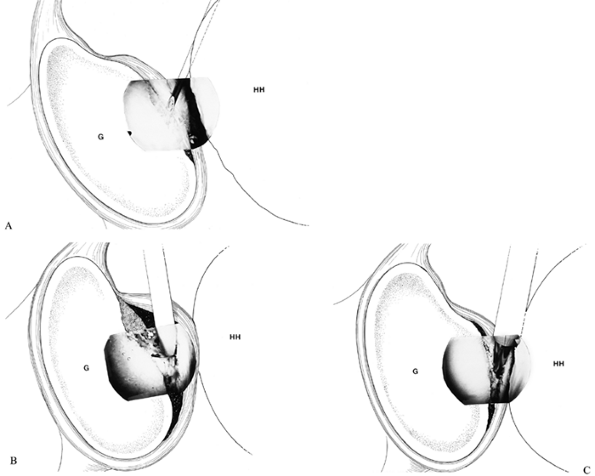 Figure 80.53. Arthroscopic Bankart repair. A: Use a spinal needle to localize the appropriate portal location. B: Use arthroscopic electrocautery to mobilize the anterior band of the IGHL and prepare the anterior glenoid rim. C: Use an arthroscopic burr to create a bleeding surface to promote postoperative healing.
Figure 80.53. Arthroscopic Bankart repair. A: Use a spinal needle to localize the appropriate portal location. B: Use arthroscopic electrocautery to mobilize the anterior band of the IGHL and prepare the anterior glenoid rim. C: Use an arthroscopic burr to create a bleeding surface to promote postoperative healing. -
Prepare the glenoid rim through the same anterior portals, making sure to effectively mobilize the anterior
P.2180P.2181
capsulolabral tissue (Fig. 80.53B).
As previously described, create a trough with the burr to prevent the
drill from slipping and possibly damaging the articular cartilage (Fig. 80.53C). -
This suture anchor system requires
predrilling before anchor placement. Drilling is performed through the
anteroinferior portal. The system contains a drill guide, which
maintains appropriate orientation and drill hole location. Remove the
drill and keep the guide in place. Tap the suture anchor loaded with
braided suture into place (Fig. 80.54A). Apply tension to the suture ends to test the fixation.![]() Figure 80.54. Arthroscopic Bankart repair. A:
Figure 80.54. Arthroscopic Bankart repair. A:
Impact a suture anchor loaded with a nonabsorbable, braided suture into
the anterior glenoid rim through the anteroinferior portal. B:
Use a cannulated hook to pass the Shuttle Relay through the IGHL, and
then pull it through the anterosuperior portal, using an arthroscopic
grasper. C: Use the Shuttle Relay to pass
the suture in the anterosuperior portal through the IGHL, which is then
tied arthroscopically with half-hitch knots. D: Alternatively, use a suture-transport system to pass the suture through the soft tissue. -
Perform the remaining portion of the
procedure, using a suture hook and Shuttle Relay system or a
suture-transport system as previously mentioned. If the Shuttle Relay
is to be used, pass one limb of the suture through the anterosuperior
portal with a grasper. Pass a suture hook loaded with a Shuttle Relay
through the anteroinferior capsule and IGHL. Take care to avoid tearing
the tissue while grasping enough tissue to adequately reduce joint
volume. If using the Shuttle Relay, advance it through the suture hook
and pull it through the anterosuperior cannula with a grasper (Fig. 80.54B). Remove the suture hook while maintaining tension on the
P.2182
Shuttle Relay; then load the eyelet of the Shuttle Relay with the
previously passed suture, and pull this suture in a retrograde fashion
back through the tissue and the anteroinferior cannula. -
Leave the second limb of suture free,
rather than passing it through the tissue. This technique pulls the
tissue to the glenoid rim, and bunches it together to recreate the
“chock block” effect of the labrum. Then tie the suture with an
arthroscopic knot pusher (Fig. 80.54C). In the
case illustrated, a half-hitch technique was used to secure the tissue,
essentially tying the suture with alternating half-knots. There are
other knot-tying techniques (i.e., Tennessee slider) that allow
immediate locking of the stitch by pulling the post. These knots have
the benefit of being lower profile. -
Alternatively, if using a
suture-transport system, pass the device through the anteroinferior
portal and tissue. Grasp one limb of the suture still in the
anteroinferior portal, and pull the device and suture in retrograde
fashion back through the tissue and cannula (Fig. 80.54D). Then use an arthroscopic knot pusher, and tie the nonabsorbable suture.
Further, there are also problems that can arise with use of suture.
These problems and the most appropriate methods of avoiding and solving
them are presented in Table 80.9 and Table 80.10.
|
Table 80.9. Suretac Technical Errors
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||
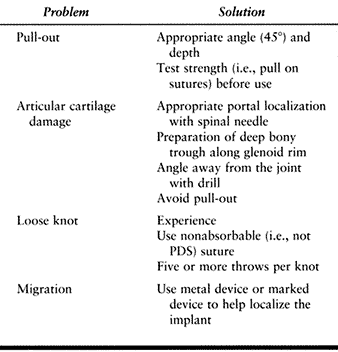 |
|
Table 80.10. Suture Anchor Technical Errors
|
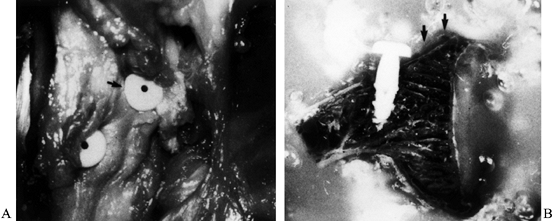 |
|
Figure 80.55. Arthroscopic Bankart repair. A: The Suretac implant has been placed too far medially (arrow) in this cadaveric specimen. B: This coronal dissection demonstrates a medially placed implant. Arrows
demonstrate the correct location for implant placement and a persistent capsulolabral separation that results from medial Suretac placement. (From Warner JJ, Miller MD, Marks P. Arthroscopic Bankart Repair with the Suretac Device. Part II. Experimental Observations. Arthroscopy 1995;11:14, with permission.) |
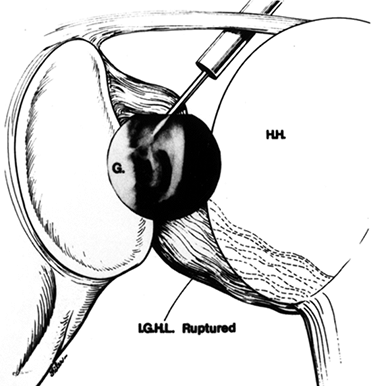 |
|
Figure 80.56. Arthroscopic Bankart repair. A: Arthroscopic view demonstrates a rupture in the anterior band of the IGHL while the arm is in the neutral position. B:
With the arm in abduction, the degree of damage is further demonstrated. Incompetent or damaged ligamentous tissues prohibit adequate arthroscopic shoulder stabilization. (From Warner JJP. Arthroscopic Bankart Repair. In: Bigliani LU, ed. Shoulder Instability. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1996:47, with permission.) |
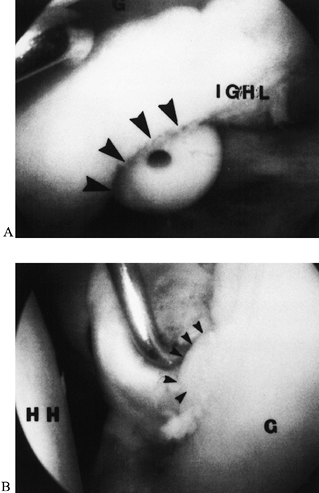 |
|
Figure 80.57. Arthroscopic Bankart repair. A: Arthroscopic view through the anterosuperior portal demonstrates a Suretac implant that has buttonholed (arrows) through the anterior band of the IGHL. B: Viewing through the posterior portal demonstrates limited soft tissue under the head (arrows)
of the device. (From Warner JJP, Altchek DW. Arthroscopic Repairs for Instability. In: Warner JJP, Iannotti JP, Gerber C, eds. Complex and Revision Problems in Shoulder Surgery. Philadelphia: Lippincott–Raven Publishers, 1997:39, with permission.) |
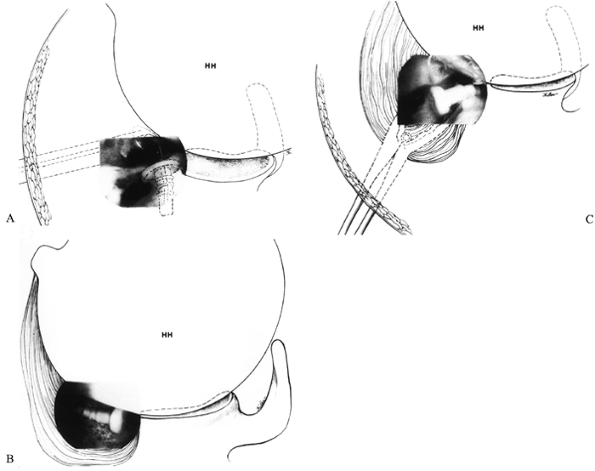 |
|
Figure 80.58. Arthroscopic Bankart repair. A:
Arthroscopic view through the anterosuperior portal demonstrates a bent guidewire and associated implant breakage during attempted repair of a posterior Bankart lesion. B: The Suretac has fallen into the axillary pouch. C: The implant is retrieved from the axillary pouch with the use of an accessory posterior portal (HH, humeral head). (From Warner JJP, Altchek DW. Arthroscopic Repairs for Instability. In: Warner JJP, Iannotti JP, Gerber C, eds. Complex and Revision Problems in Shoulder Surgery. Philadelphia: Lippincott–Raven Publishers, 1997:40, with permission.) |
Allow bathing and elbow–wrist range of motion at 1 week, but external
rotation past neutral should be avoided. Allow passive and
active-assisted range-of-motion exercises and pulley exercises at 4
weeks. Initiate elastic band rotator cuff strengthening exercises at 2
months and weight training at 4 months. Allow noncontact sports at 4
months and contact sports at 6–9 months, depending on the level of
contact.
While results with these methods have been good, they have not been on
par with the results after treatment of traumatic unidirectional
anterior instability; return to overhead athletic activities has been
less certain. Moreover, there is a perception that perioperative
morbidity might be improved with a “less invasive” arthroscopic
technique. For this reason, several surgeons have attempted to develop
arthroscopic methods of capsulorrhaphy to treat patients with MDI.
While some surgeons have reported on their initial experience with
these methods (Eugene Wolf and Steven Snyder, personal communications),
little has been reported in the peer-reviewed literature.
the anterior and inferior capsule with an end-cutting shaver. This
division allowed the inferior capsule to be advanced superiorly.
Sutures were tied with a transglenoid suture technique. This initial
report was a preliminary study of 10 patients who were all found to
have a “satisfactory” shoulder according to the Neer and Foster
criteria. An average Rowe score of 90 was reported, as well.
Modifications of this transglenoid suture capsulorrhaphy have been
developed to address posterior instability (100).
described a technique of capsular plication in a select population with
MDI and no associated labral pathology. All patients underwent a
prolonged course of rehabilitation before surgical intervention, which
allowed serial examinations. Over the weeks, the physicians’ knowledge
of the patient and the underlying disorder increased. Thus, patients
with voluntary instability of a psychological nature could be
identified.
-
This technique is performed in the
lateral decubitus position, using the standard posterior and
anterosuperior portals as described previously. In addition, an
anterior mid-glenoid portal is used corresponding to an area
approximately 3 cm distal and 2 cm lateral to the anterosuperior
portal. This portal is made through an outside-in technique and enters
the joint just over the subscapularis tendon in a manner similar to the
anteroinferior portal previously described. -
Place a large (8.4 mm) cannula into this
portal to provide access for large suture hooks. For anterior
plication, place the arthroscope posteriorly, and abrade the synovium
along the anterior and inferior capsule with a rasp or 4.5 mm
arthroscopic shaver (Fig. 80.59A).
P.2186P.2187P.2188
This abrasion creates bleeding, which will subsequently promote healing.![]() Figure 80.59. Arthroscopic capsular shift. A: Use an arthroscopic rasp to prepare the anterior capsule through the anteroinferior portal. B: Pass a suture hook through the inferior capsule. C:
Figure 80.59. Arthroscopic capsular shift. A: Use an arthroscopic rasp to prepare the anterior capsule through the anteroinferior portal. B: Pass a suture hook through the inferior capsule. C:
The hook allows passage of the Shuttle Relay through the inferior
capsule and labrum, and the relay is then passed through the
anterosuperior portal using an arthroscopic grasper. D:
Use the Shuttle Relay to pass the suture in a retrograde fashion
through the tissue. (From Wichman MT, Snyder SJ. Arthroscopic Capsular
Plication for Multidirectional Instability of the Shoulder. Oper Tech Sports Med 1997;5:238, with permission.) -
Pass a 90° suture hook with a loaded
Shuttle Relay through the anteroinferior cannula and create a pinch
stitch by taking anteroinferior capsule and advancing it superiorly and
medially to the anteroinferior labrum (Fig. 80.59B). A 1-cm-thick fold is produced between the capsule and labrum. -
Deliver the Shuttle Relay through the end of the hook, and pull it through the anterosuperior portal with a grasper (Fig. 80.59C).
Lead the eyelet of the Shuttle Relay with a braided, nonabsorbable
suture, and pull it in a retrograde fashion through the labrum and
capsule and out the anteroinferior portal (Fig. 80.59D). Repeat this process slightly more superiorly to create a horizontal mattress stitch (Fig. 80.60A).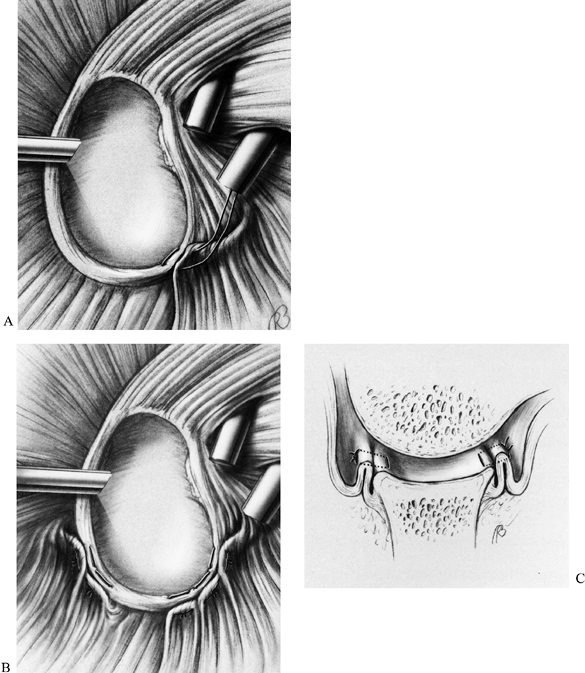 Figure 80.60. Arthroscopic capsular shift. A: Repeat the process for the second limb of the suture to create an effective horizontal stitch. B: The process can be repeated anteriorly, inferiorly, and posteriorly for the patient with MDI. C:
Figure 80.60. Arthroscopic capsular shift. A: Repeat the process for the second limb of the suture to create an effective horizontal stitch. B: The process can be repeated anteriorly, inferiorly, and posteriorly for the patient with MDI. C:
The goal is to decrease the capsular volume and recreate the “chock
block” effect of the labrum. (From Wichman MT, Snyder SJ. Arthroscopic
Capsular Plication for Multidirectional Instability of the Shoulder. Oper Tech Sports Med 1997;5:238, with permission.) -
If posterior plication is anticipated, it
is recommended that the posterior portal be created slightly more
superiorly. Of course, hook and suture placement would be performed
with the arthroscope through the anterosuperior portal in this case.
within 10° of the preoperative level in 92% of patients at a minimum
2-year follow-up. An assessment of postoperative function using the
American Shoulder and Elbow Society instrument revealed an improvement
from a preoperative score of 63 to a postoperative score of 86.2 The
average Rowe score postoperatively was 79.6. Five patients’s conditions
were rated unsatisfactory, with 19 patients having satisfactory
ratings, according to Neer’s criteria. The authors noted a
disproportionately high number of workers’ compensation cases in the
unsatisfactory group. Interestingly, three patients underwent
second-look arthroscopy (two for unrelated procedures) that revealed
significant capsule formation at the site of previous plication and no
adverse synovial reaction to the suture.
to 460 BC when Hippocrates inserted a hot iron into the axilla,
contracting the inferior aspect of the joint. This same concept has
gained recent popularity, but laser and radiofrequency energy sources
are used to produce the heat. The triple-helix structure of collagen
unwinds at 65°C, undergoing a conformational change from a crystalline,
extended state to a randomly coiled, contracted state (denatured) and
producing shrinkage in capsular tissues (106). Current literature has focused on laser technology as a source of the thermal energy. Hayashi et al. (66) demonstrated a dose-dependent effect of nonablative laser energy on capsular tissue properties.
Laser energy at low power—less than 10 watts (1.0 joule per pulse at 10
hertz)—is recommended for laser-assisted capsular shrinkage. There are
several disadvantages to the use of laser energy. First, lasers are
very expensive and require a certain level of expertise and appropriate
certification for use. Further, lasers produce significant power that
can be difficult to control.
alternative energy source that avoids some of the problems inherent in
laser energy. Such devices are less expensive and are relatively easier
to use. The ElectroThermal Arthroscopy system (ORATEC Interventions,
Inc., Menlo Park, CA) integrates a thermocouple into the arthroscopic
handpiece, creating a monopolar system. The current applied to the
tissue at the dull probe tip is minimally invasive while still
accomplishing collagen denaturation (S.P. Arnoczky, personal
communication). This system contrasts with the vapor system from Mitek
Surgical Products, Inc. (Westwood, MA), which represents a bipolar
system without a thermocouple. Both products are radiofrequency systems.
several years as an experimental treatment method. Their obvious appeal
is that they can be used effectively in an outpatient setting. The
procedure does not require a great deal of time or the use of sutures
or implants. Unfortunately, while anecdotal reports concerning these
procedures are appearing, there is currently no peer-reviewed
literature available regarding the effectiveness of this technique.
Nevertheless, thermal capsular shrinkage remains a possible alternative
treatment. Its efficacy will need to be substantiated over the next
5–10 years with well controlled follow-up studies to assess whether
there is a gradual restretching of the tissues with increased use.
the criteria for arthroscopic shoulder stabilization are becoming more
clearly defined. As surgeons continue to improve their ability to
arthroscopically shift the glenohumeral ligaments and repair labral
lesions and as new technologies are developed, the number of patients
who are candidates for open surgical procedures will decrease.
Certainly, the presence of a large Hill–Sachs lesion or a bony Bankart
lesion on radiographic examination is an indication for an open
surgical approach. Likewise, patients without a significant Bankart
lesion by MRI or CT may not be optimal candidates for an arthroscopic
Bankart procedure. Similarly, findings consistent with significant
capsular laxity or stretch, such as an atraumatic history or MDI
findings on physical examination, should direct the surgeon toward open
treatment options. Significant capsular damage, rotator interval
lesions, or rotator cuff tears are also currently better repaired with
open surgical techniques.
to treat anterior glenohumeral instability. TheMagnuson-Stack and
Putti-Platt procedures attempted to realign and tighten the
subscapularis tendon (158,179).
The anterior capsule was also tightened by the latter technique. The du
Toit staple capsulorrhaphy attempted to reattach the capsule and
glenoid (15,143). The Bristow
and other bone block procedures attempted to replace the injured anterior labrum and glenoid (10).
reasonable success rates in decreasing recurrent instability. Long-term
follow-up studies continued to reveal low recurrence rates, but
techniques that used metal staples or screws revealed high rates of
hardware-related problems. Zuckerman and Matsen (188)
retrospectively reviewed 37 patients who had previously been treated
with a modified Bristow procedure, a staple capsulorrhaphy, or a
modified Magnuson-Stack procedure. The hardware migrated or loosened in
24 shoulders and broke in three patients. Thirty-four patients required
a second operation to remove the hardware. At reoperation, 41%
demonstrated significant injury to the articular surface. Other studies
have reported similar rates of hardware-related complications (59,185).
Further, because of failure to correct the underlying anatomic problem,
many patients had significant loss of external rotation or frank
internal rotation contractures and subsequent glenohumeral arthritis (61).
the presumed anatomic abnormality, Rowe and colleagues popularized the
Bankart procedure for anterior unidirectional instability (130,131,133,134).
-
This technique uses a standard
deltopectoral approach. Classically, the subscapularis tendon is
incised vertically at its lateral insertion and sharply dissected
medially from the anterior capsule (Fig. 80.61A).
Several alternatives for subscapularis dissection have been developed
that purportedly gave equal exposure of the anterior capsule (Fig. 80.61B, Fig. 80.61C) (77,96).![]() Figure 80.61. Bankart procedure for anterior unidirectional instability. A: Perform a standard lateral subscapularis dissection 1 cm from its insertion onto the lesser tuberosity. B: An L-shaped dissection avoids the anterior circumflex humeral vessels but prevents complete access to the inferior capsule. C:
Figure 80.61. Bankart procedure for anterior unidirectional instability. A: Perform a standard lateral subscapularis dissection 1 cm from its insertion onto the lesser tuberosity. B: An L-shaped dissection avoids the anterior circumflex humeral vessels but prevents complete access to the inferior capsule. C:
Alternatively, the subscapularis muscle can be horizontally split,
which avoids the need for later repair of the tendon. (From Zarins B.
Bankart Repair for Anterior Shoulder Instability. Tech Orthop 1989;3:23, with permission.) -
Make a vertical capsulotomy approximately 0.5 cm lateral to the glenoid rim with the arm in complete external rotation (Fig. 80.62).
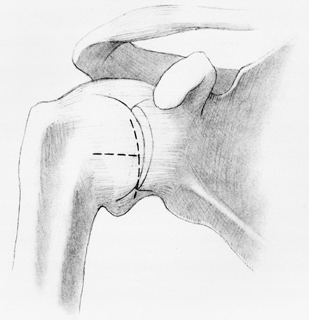 Figure 80.62.
Figure 80.62.
Bankart procedure for anterior unidirectional instability. A medially
based capsulotomy can be converted to a T-shaped capsulotomy that
allows improved mobilization of the inferior axillary pouch in patients
with increased anteroinferior instability. (From Zarins B. Bankart
Repair for Anterior Shoulder Instability. Tech Orthop 1989;3:23, with permission.) -
With complete muscle relaxation, insert a
humeral head retractor and inspect the glenoid for evidence of a
Bankart lesion. If a Bankart lesion is present, repair the lateral
capsular flap to the glenoid neck. -
Prepare this area with a curet to expose bleeding bone,
P.2191
and drill three holes; one at the 2-o’ clock, one at the 4-o’ clock,
and one at the 6-o’ clock positions for right shoulders (10-, 8-, and
6-o’ clock positions for left shoulders) as demonstrated in Figure 80.63.![]() Figure 80.63.
Figure 80.63.
Bankart procedure for anterior unidirectional instability. Make drill
holes along the glenoid rim at the 1-, 3-, and 5-o’clock positions for
right shoulders. (From Zarins B. Bankart Repair for Anterior Shoulder
Instability. Tech Orthop 1989;3:23, with permission.) -
Pass sutures through the holes and the lateral capsular flap with a Mayo needle (Fig. 80.64A).
Tie the flap down to the glenoid rim, and pass these same sutures
through the small medial capsular flap, reinforcing the repair (Fig. 80.65).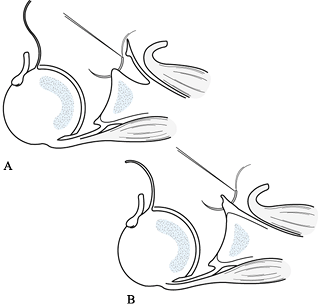 Figure 80.64. Bankart procedure for anterior unidirectional instability. A: Pass the suture through drill holes in the glenoid rim. B:
Figure 80.64. Bankart procedure for anterior unidirectional instability. A: Pass the suture through drill holes in the glenoid rim. B:
Alternatively, if there is no significant Bankart lesion, the suture
can be placed directly through the anterior labrum. (From Zarins B.
Bankart Repair for Anterior Shoulder Instability. Tech Orthop 1989;3:23, with permission.)![]() Figure 80.65.
Figure 80.65.
Bankart procedure for anterior unidirectional instability. Pull the
inferior capsular flap superiorly to the glenoid rim first. Arm
position is critical during this portion of the procedure and
determines final postoperative motion. Increasing abduction and
external rotation will improve final postoperative motion. (From Zarins
B. Bankart Repair for Anterior Shoulder Instability. Tech Orthop 1989;3:23, with permission.) -
If no Bankart lesion is found on inspection, merely place sutures through the labrum rather than drill holes (Fig. 80.64B).
-
With the production of multiple suture
anchors, many surgeons have modified the procedure, using these
implants along the glenoid rim (87). Despite
reports of good success with these devices, there remains a risk of
technical failure and resultant instability or articular cartilage
damage.
reported good-to-excellent results in 96.5% of patients, with a 3.5%
recurrence rate, using this procedure. A loss of terminal external
rotation, however, was noted in many patients. Further, only 33% of
throwing athletes with involvement of the dominant arm were able to
return to their original level of competition. Rosenberg et al. (128) demonstrated a
statistical relationship between late degenerative changes and
restriction of external rotation in 90° of arm abduction. These reports
led others to modify the operative techniques to address these
problems. In addition, the increased association between repeated
subluxations or dislocations and subsequent capsuloligamentous injury
has shifted attention toward correction of the associated capsular
laxity.
developed to treat underlying anteroinferior capsular laxity with an
associated Bankart lesion (3).
-
Expose the anterior capsule as previously
described. In addition to the vertical capsulotomy at the glenoid
margin, create a transverse limb at the mid portion of the capsule (Fig. 80.62). -
If a Bankart lesion is visualized,
prepare the glenoid neck as previously described. If there is no
lesion, pass sutures through the labrum rather than through drill holes. -
Position the arm in 40° of external
rotation and 45° of abduction. Then pull the inferior flap superiorly
and medially to the upper rim to allow 40° external rotation (Fig. 80.66),
reduce the inferior redundancy, and simultaneously correct for a
Bankart lesion, if present. Pull the superior flap inferiorly and
medially to reinforce the inferior flap (Fig. 80.67).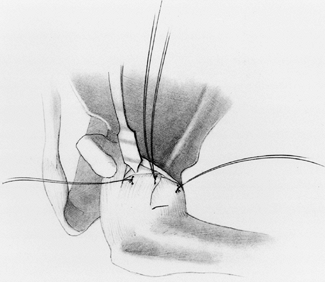 Figure 80.66.
Figure 80.66.
T-plasty modification of the Bankart procedure. Pull the superior
capsular flap inferiorly with the arm in slight abduction and external
rotation. (From Zarins B. Bankart Repair for Anterior Shoulder
Instability. Tech Orthop 1989;3:23, with permission.)![]() Figure 80.67.
Figure 80.67.
T-plasty modification of the Bankart procedure. Pull the medial flap
over the lateral flap to supplement the repair. (From Zarins B. Bankart
Repair for Anterior Shoulder Instability. Tech Orthop 1989;3:23, with permission.)
their experience with this procedure involving 42 shoulders in 40
athletes. Postoperatively, 20 shoulders had external rotation in
adduction that was symmetric to the opposite side. The remaining22
shoulders, however, demonstrated a loss of 5° to 25° external rotation
(average, 10°). Despite 95% excellent results with this procedure,
throwing athletes in this study continued to report a decrease in
maximum ball speed on throwing.
similar operation but used a horizontal split in the subscapularis
muscle to expose the anterior capsule. This method avoids the risk of
postoperative subscapularis tendon disruption (59).
Intraoperatively, they made sure no tension was present along the
suture line until 90° of abduction and 45° of external rotation was
reached. Patients were then splinted in 90° of abduction, 45° of
external rotation, and 30° of forward flexion. With this technique,
they reported excellent results in 68% of a group of overhand athletes.
Despite these efforts, six patients had a loss of 10° to 20° external
rotation. An assessment of the 12 skilled pitchers in this study
revealed that 50% returned to their former level of competition for at
least one season.
to obtain full terminal rotation postoperatively with this repair
technique; further, full external rotation is necessary for high-level
pitchers to obtain peak throwing velocity. In Neer and Foster’s (107)
classic article on MDI, the inferior capsular shift was introduced.
Like the modified Bankart procedures described above, this technique
involved a T-shaped capsulotomy, but the vertical cut was made
laterally along the humeral neck and a horizontal cut was made between
the middle glenohumeral ligament (MGHL) and the IGHL. If a rotator
interval defect was noted, it was repaired and then the same horizontal
cut created.
involuntary inferior and multidirectional instability. If a patient had
an associated Bankart lesion, however, it was repaired with the use of
an inside-out suture technique at the glenoid rim. A shallow trough was
made laterally along the humeral neck. Neer and Foster recommended
holding the arm in 10° external rotation while suturing the inferior
flap to the stump of the subscapularis tendon and to the remaining cuff
of capsule along the humeral neck. The superior flap containing the
MGHL was then sutured over the inferior flap to reinforce the repair.
The tension on the inferior flap was selected to reduce the inferior
and posterior capsular laxity. The lateral capsulotomy, as opposed to
the medial approach, has a greater ability to reduce capsular volume
because the capsular circumference is largest laterally.
a series of inferior capsular shift procedures performed in 68
shoulders in 63 athletic individuals. On the basis of Neer and Foster’s
experience and the concept that anterior instability in the athlete
represents a spectrum of pathology, they performed an inferior capsular
shift in all cases. The inferior capsule was mobilized and shifted on
the basis of the degree of inferior laxity demonstrated by EUA in each
individual. Initially, the shoulders were repaired with the arm in 20°
of abduction and 10° of external rotation. However, as it was noticed
that only 50% of the overhead athletes involved in throwing had
excellent results, abduction and external rotation were increased by
10° at the time of repair. Despite modifications in technique and
postoperative mobilization, only 5 of 10 overhead athletes returned to
their same level of competitiveness. Only two of six varsity or
professional overhead athletes were able to return to the same level of
sporting activity.
based on the clinical observation that a spectrum of labral and
capsuloligamentous pathology exists, as well as on experimental
observations concerning the role of the glenohumeral ligaments (171).
instability may have a Bankart lesion, while others may have capsular
injury without labral pathology. It is generally believed that some
capsuloligamentous damage is created with each episode of instability.
As a result, it becomes difficult to categorize patients purely on the
basis of history or physical examination. An operative repair should be
able to address all intraarticular pathology adequately.
superior glenohumeral ligament and the MGHL function as a static
barrier to anteroinferior humeral head translation with the arm in
adduction and external rotation (37,160).
Similar studies demonstrate that the IGHL serves as a static restraint
to translation with progressive increases in abduction and external
rotation (113,114 and 115).
As a result, in the technique that follows, each capsular flap is
sutured with the arm in the position that maintains greatest tension on
ligamentous structures being repaired, contributing, it is hoped, to
overall postoperative motion.
previously, and the degree of capsular laxity is used to determine the
amount the inferior capsule that should be mobilized.
-
Place the patient in a semisitting
position resting on a long bean bag. Contour the bag along the medial
scapular border, allowing the injured shoulder and arm to hang over the
edge of the table. First, mold and solidify the bag, and then pull the
entire construct over the edge of the table. A McConnell Shoulder
Holder (McConnell, Inc., Greenville, TX) allows proper positioning of
the arm. Use a standard deltopectoral approach, with the incision
maintained low in the axillary fold for better cosmesis. Place a
self-retaining retractor into the interval.
P.2194
Make
a small transverse incision, if needed, in the conjoined tendon just
distal to the coracoid tip to increase medial exposure. Maintain manual
retraction along the conjoined tendon to avoid a neuropraxic injury to
the musculocutaneous nerve. Resect the coracoacromial ligament to
better expose the superior capsule and evaluate the rotator interval. -
Isolate the anterior circumflex humeral
vessels, and suture-ligate them at the inferior aspect of the
subscapularis muscle. Use needle-tip electrocautery to dissect the
subscapularis muscle from lateral to medial off the anterior capsule in
the coronal plane. Palpate the axillary nerve; then visualize and
isolate it with a vessel loop to avoid injuring it during surgery. -
If no significant rotator interval lesion
is noted, create a T-shaped capsulotomy with the horizontal cut between
the MGHL and the IGHL, ending at the equator of the glenoid. Make the
vertical component of the capsulotomy just medial to the lateral
insertion of the capsule into the humeral neck. At this point, consider
the degree of capsular laxity demonstrated during the EUA. The position
of the vertical capsulotomy may range from 6 o’ clock to 8 o’ clock
along the humeral neck, depending on the degree of inferior laxity. If
there is significant inferior laxity, choose the latter position. Carry
the vertical component up to the supraspinatus tendon superiorly. With
maximal muscle relaxation, place a humeral head retractor into the
joint, and visualize the anterior labral region.
scapular neck, and place a three-prong retractor medially along the
scapular neck for exposure. Then decorticate the glenoid surface, using
a small osteotome. Place suture anchors (Acufex Microsurgical, Inc.,
Mansfield, MA) loaded with a #1 nonabsorbable suture into the 2-, 4-,
and 6-o’ clock positions for right shoulders or corresponding positions
for left shoulders. Then place sutures through the capsule from the
inside-out, and tie them over the capsule in a horizontal mattress
fashion to repair the Bankart lesion (Fig. 80.68).
Take care to repair the capsule without any shortening in a medial
direction. No shifting of the capsule is performed at this point, as an
anatomic repair of the Bankart lesion is the goal.
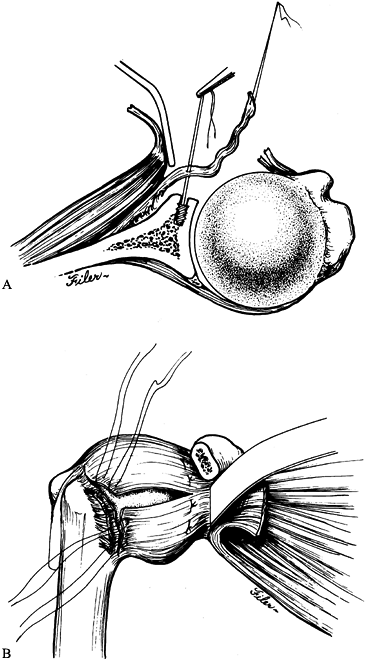 |
|
Figure 80.68. Open selective capsular shift. A:
After a lateral capsulotomy, mobilize the capsule laterally from its scarred position along the glenoid rim. Place a suture anchor along the rim, and pull each limb of the suture through the capsule. B: Typically, three suture anchors are placed and tied in horizontal fashion. An additional horizontal capsulotomy creates superior and inferior flaps. (From Warner JJP, Johnson D, Miller MD, Caborn DN. Technique for Selecting Capsular Tightness in Repair of Anteroinferior Shoulder Instability. J Shoulder Elbow Surg 1995;352, with permission.) |
-
Remove the humeral head retractor, and
place the shoulder into 60° to 80° of abduction, 45° to 60° of external
rotation, and 10° of forward flexion. Pull the inferior capsular flap
superiorly and laterally, and suture it to the cuff of capsular tissue
at the humeral neck (Fig. 80.69A). Adjust
abduction and external rotation on the basis of the individual’s needs.
Thus, if the operation involves the dominant arm of a throwing athlete,
position the arm in 80° of abduction and 60° of external rotation. Use
lower degrees if treatment involves a nondominant arm or an athlete
involved in a sport with limited overhead activity.![]() Figure 80.69. Open selective capsular shift. A:
Figure 80.69. Open selective capsular shift. A:
Tie the inferior flap to the superolateral capsular tissue with the arm
in 40° of abduction and between 45° and 80° of external rotation. The
amount of rotation depends on the postoperative expectations of the
patient. B: Tie the superior flap to the
inferolateral tissue with the arm in neutral to 10° of abduction and
45° to 60° of external rotation. (From Warner JJP, Johnson D, Miller
MD, Caborn DN. Technique for Selecting Capsular Tightness in Repair of
Anteroinferior Shoulder Instability. J Shoulder Elbow Surg 1995;352, with permission.)
the arm in 0° of adduction and 45° of external rotation. The superior
capsular flap is then sutured inferiorly and laterally over the other
flap (Fig. 80.69B). Place sutures, which were previously placed through the inferior flap,
through the superior flap to create a pants-over-vest closure.
are associated with increased inferior laxity in adduction, into the
capsulotomy. This method is in contrast to repairing the defect as Neer
and Foster recommend. The rotator interval becomes part of the
horizontal cut to create an upside-down L-shaped capsulotomy (Fig. 80.70A, Fig. 80.70B).
Suture the inferior capsular flap as previously described, but apply
tension to the remaining superior capsule by repairing the horizontal
portion of the inferior flap over the superior flap with the arm in 0°
of adduction and 45° of external rotation (Fig. 80.70C, Fig. 80.70D).
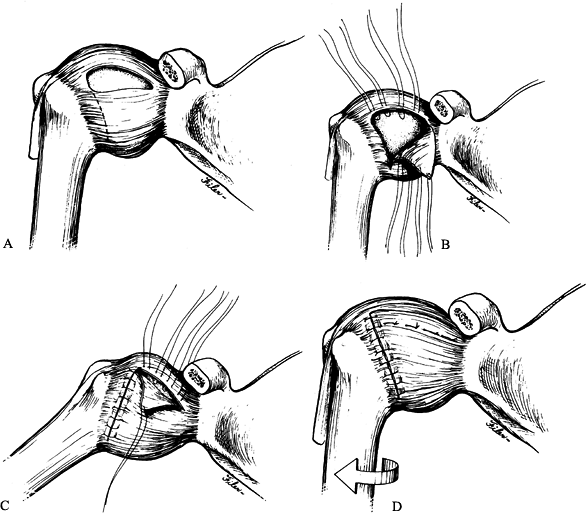 |
|
Figure 80.70. Open selective capsular shift. A:
A rotator interval lesion is demonstrated in associated with increased inferior laxity in neutral abduction that does not stabilize with increasing external rotation. B: Incorporate this capsular defect, if present, into the capsulotomy, creating an inverted L-shaped capsulotomy. C: Mobilize the tissue superiorly, and tie it to the lateral capsular tissue with the arm in abduction and external rotation. D: Subsequently, repair the rotator interval lesion with the arm in neutral abduction and external rotation. (From Warner JJP, Johnson D, Miller MD, Caborn DN. Technique for Selecting Capsular Tightness in Repair of Anteroinferior Shoulder Instability. J Shoulder Elbow Surg 1995;352, with permission.) |
possible in the scapular plane. Further, in this position, 60° of
external rotation should be possible before tension is noted along the
suture lines. With the arm in 0° of adduction, external rotation to 45°
should be possible with minimal tension along the repair. Typically, an
intraoperative drawer test is performed, and with the arm in 45° of
abduction and neutral rotation, anterior and posterior drawer tests
should not be greater than 1+. The shoulder should further stabilize
with increased abduction and external rotation, with the drawer tests
decreasing to zero. The inferior drawer test should be 0–1+ with the
arm at the side. If so, the subscapularis tendon is repaired
anatomically.
swathe for 3–4 weeks, allowing the patient to perform limited abduction
for axillary care and dressing. During this period, allow the patient
to flex and extend the elbow. Then remove the sling and institute
unlimited active-assisted range-of-motion exercises, as well as
isometric strengthening for external rotation, flexion, extension, and
abduction of the arm. Caution the patient to avoid internal rotation
for 6 weeks to prevent stress on the subscapularis repair.
elastic bands, and at 4 months allow the patient to swim, throw a ball,
or hit gentle ground strokes in tennis. At 6 months, release the
patient to more forceful throwing or swinging. Do not allow the patient
to return to contact sports until 8 months after the operative
procedure.
Yet there is increasing evidence that a higher prevalence of posterior
subluxation exists, especially in overhead athletes, than previously
recognized (50,123,156).
Operative procedures that have treated posterior instability have been
less successful than anterior procedures at preventing recurrent
instability.
procedures, it is important in primary and revision cases to attempt an
adequate course of nonoperative management. Focus rehabilitation on
strengthening the dynamic muscle stabilizers to correct for the
deficient posterior static stabilizers. Specifically, exercises should
focus on strengthening the rotator cuff and deltoid and scapular
muscles. Further, the patient and the therapist should be educated to
avoid forward flexion, adduction, and internal rotation, as these
positions place increased stress on the posterior structures. If this
process fails to alleviate symptoms or episodes of instability, it is
important to focus on patient goals, as the outcome of surgical
treatment may be unsatisfactory to the patient.
capsulorrhaphy and posterior transfer of the long head of the biceps
brachii in nine shoulders and reported no recurrences. Mowery et al. (105)
reported on the use of a posterior bone block in five patients with
recurrent posterior dislocations. Four of the five cases were rated as
excellent at a minimum 2.5-year follow-up. However, closer evaluation
revealed that one patient underwent screw removal, and one of the bone
grafts was deemed osteoporotic at 3 years. Further, in the fifth case
that was rated as good, the patient required a manipulation under
anesthesia for limited motion and subsequently suffered from anterior
instability.
the uncommon nature of posterior instability and confusion in the
literature in differentiating subluxations from dislocations led to a
poor understanding of this entity. In the same article, they
retrospectively reviewed 50 shoulders in 35 patients treated for
recurrent posterior instability. Only 11 patients had had a primary
traumatic event before the onset of instability. Forty-one of the
affected shoulders demonstrated voluntary, positional instability that
affected activities of daily living. Thirteen of 26 shoulders that
underwent surgical reconstruction (17 posterior
glenoid osteotomies, six reverse Putti-Platt procedures, and three
biceps tendon transfers) developed recurrent instability. The authors
also noted that the posterior glenoid osteotomy was associated with
osteoarthritis.
presented a series of 24 patients with posterior subluxation who were
divided into two groups. Members of the first group, who had less
severe
symptoms, were treated with physical therapy and had a 63% success
rate. Group II consisted of individuals who either failed physical
therapy or had more severe symptoms. They were treated with a posterior
capsulorrhaphy with or without a posterior bone block. In this group,
91% suffered no additional episodes of instability. However, 70% of the
athletes in both groups participated in sports at a diminished level.
on their experience using a posterior staple capsulorrhaphy technique.
Twenty athletes were treated for recurrent posterior subluxation, with
eight of them also suffering from concomitant anterior instability. In
this series, six patients suffered from recurrent posterior
instability, while an additional three patients had moderate to severe
pain. Significant complications that were a direct result of the
procedure developed in five patients. They concluded that this
technique was not an acceptable treatment option for posterior
instability.
reported on their experience using a posterior suture capsulorrhaphy
technique that avoided the complications associated with staples or
bone blocks.
-
This technique, which was very similar to that described by Fronek et al. (48),
used a posterior saber incision starting at the acromion and
terminating in the posterior axillary fold. Split the deltoid muscle in
line with its fibers approximately 2–3 cm medial to the posterolateral
corner of the acromion for 5–6 cm, with care to avoid injury to the
axillary nerve, which enters the muscle distal to the teres minor
muscle. -
Develop the interval between the
infraspinatus and teres minor muscles, and expose the underlying
capsule. Make a T-shaped capsulotomy with the horizontal component at
the glenoid rim. -
Transfer the inferior flap superiorly and
medially. Secure it to the glenoid rim with #1 nonabsorbable suture
placed through the labrum, if it is intact. -
If there is significant labral pathology,
expose the glenoid rim, and prepare it as previously described for
anterior repairs. Suture the capsular flap through bone holes, or
secure it with suture anchors. Once again, the superior flap is sutured
over the inferior flap to reinforce the repair. Position the arm in
neutral rotation during the repair.
repair with infraspinatus advancement or bone blocks. Researchers
reported a 40% failure rate in 40 athletes who were followed
adequately, attributing the failures to ligamentous laxity or
unrecognized MDI. Importantly, they also noted worsening results as the
athletes’ competitive level increased and concluded that high-level
athletes should be informed preoperatively of a possible poor outcome.
A cadaveric and clinical investigation was undertaken to study an
infraspinatus muscle-splitting approach to the posterior capsule.
Dissection of 20 cadavers revealed that the suprascapular nerve entered
the infraspinous fossa at the spinoglenoid notch as a single trunk, 22
mm medial to the glenoid rim. The infraspinatus muscle was bipennate in
all specimens, with the tendinous interval an average of 14 mm inferior
to the scapular spine. Limiting dissection in this interval to 1.5 cm
medial to the posterior glenoid rim prevented damage to any
suprascapular nerve branches. The researchers performed this approach
in four patients and reported excellent exposure of the posterior
capsule, labrum, and glenoid, thus avoiding tendon detachment.
Electrodiagnostic testing revealed no significant denervation in these
patients.
a posterior capsular shift procedure in their classic article on the
treatment of MDI. This technique has many features that are similar to
their previously described anterior capsular shift.
-
Make a 10 cm incision either horizontally
at the level of the scapular spine or vertically just medial to the
posterolateral corner of the acromion. The latter incision creates a
more cosmetic postoperative scar. -
Detach the deltoid from the posterolateral aspect of the acromion and from the lateral 9.0 cm of the scapular spine.
-
Split the deltoid muscle for
approximately 3.0 cm inferiorly, exposing the infraspinatus muscle and
tendon. This muscle–tendon unit is split obliquely, creating a
superficial tendinous flap later used to reinforce the capsule.
Mobilize the remaining infraspinatus muscle medially to expose the
underlying capsule. -
Make a T-shaped capsulotomy with the
horizontal component created laterally along the humeral neck. The
authors noted that the arm should be progressively internally rotated
during mobilization of the inferior capsular flap to protect the
axillary nerve. -
Then place a humeral head retractor into
the joint and visualize the labrum; if there is labral pathology
extending beyond the inferior glenoid rim into the anterior aspect of
the joint, a separate anterior incision is recommended to address the
Bankart lesion. Posterior labral pathology is incorporated into the
capsular shift as previously described for the anterior procedure. Once
again, this is performed before advancement of the flaps. -
Position the arm in slight extension and
external rotation during capsular reattachment. Then pull the superior
flap inferiorly and laterally, and suture it to a shallow bony trough
created at the humeral neck. Next, pull the inferior flap superiorly
and laterally, and repair it over the superior flap. The superficial
portion of the infraspinatus tendon is used to augment the posterior
P.2198
capsular
repair. The deep portion of the infraspinatus muscle is then repaired
to its origin to prevent postoperative weakness. Carefully reattach the
deltoid muscle.
extends from the wrist to the mid-arm level and around the waist. Keep
the arm in neutral flexion and extension and 10° of external rotation
for 6 weeks. Begin isometric deltoid and rotator cuff exercises at 8
weeks, and add progressive resistive exercises at 12 weeks. Using this
technique in 25 shoulders, Bigliani et al. (11) reported good-to-excellent results in 88%. This assessment was based on stability, pain, range of motion, and activity level.
place the patient into the lateral decubitus position with the injured
side up. Place an axillary roll, and pad all potential pressure points
on the downside. Inflate the bean bag, and contour it anteriorly and
posteriorly. Prepare and drape the injured arm and hemithorax in
sterile fashion. Apply a McConnell Shoulder Holder to the table
opposite the surgeon, and use it to maintain appropriate arm position
during the operation.
-
Create a vertical incision in line with
the posterior axillary fold, and carry it over the posterior acromial
edge. Employ sharp dissection through the subcutaneous tissue down to
the deltoid fascia. Raise subcutaneous flaps medially and laterally. -
Palpate the glenohumeral joint, and split the deltoid muscle in line with its fibers at this level (Fig. 80.71).
If necessary, further elevate the deltoid subperiosteally off the
acromion to the posterolateral corner of the acromion. This latter step
is usually required for large, muscular patients.![]() Figure 80.71.
Figure 80.71.
Open posterior shoulder stabilization procedure. Make a standard split
in the posterior deltoid muscle in line with the muscular fibers at the
level of the glenohumeral joint. In muscular patients, decreased
visualization may require periosteal elevation of the deltoid muscle
from the scapular spine. (From Rowe CR, Yee LB. A Posterior Approach to
the Shoulder. J Bone Joint Surg [Am] 1944;26:580, with permission.) -
Insert a self-retaining shoulder
retractor, and adequately mobilize the subdeltoid plane to expose the
underlying infraspinatus fascia (Fig. 80.72).
Then externally rotate the arm, and split the infraspinatus at the
equator of the glenoid in line with its fibers. Carefully, develop the
plane between this muscle and the underlying capsule (Fig. 80.73).
Take care with this step, as there are frequently adhesions, as well as
a thin redundant capsule. If further visualization of the capsule along
the humeral neck is required, a portion of the infraspinatus tendon
insertion may have to be released. Maintain a cuff of tissue in this
case to permit an anatomic repair later in the procedure.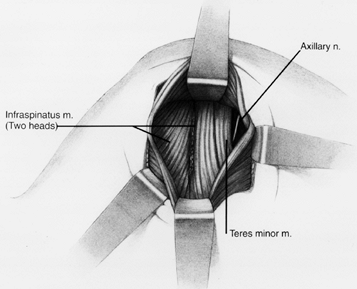 Figure 80.72.
Figure 80.72.
Open posterior shoulder stabilization procedure. Develop the interval
between the two heads of the infraspinatus muscle, which exposes the
underlying capsule. Alternatively, the glenohumeral joint can be
palpated, and the infraspinatus muscle can be split at this level.
(From Rowe CR, Yee LB. A Posterior Approach to the Shoulder. J Bone Joint Surg [Am] 1944;26:580, with permission.)![]() Figure 80.73.
Figure 80.73.
Open posterior shoulder stabilization procedure. Make a medially based
T-shaped capsulotomy. (From Rowe CR, Yee LB. A Posterior Approach to
the Shoulder. J Bone Joint Surg [Am] 1944;26:580, with permission.) -
Place long, thin manual retractors along
the infraspinatus muscle to aid in visualization at this point in the
procedure. Carefully, create a vertical capsulotomy just off the
glenoid margin to dissect inferiorly and allow adequate correction of
the capsular laxity later in the procedure. Make a horizontal cut at
the equator of the glenoid to create a T-type capsulotomy (Fig. 80.74).
If there has been concomitant avulsion of the capsule from the humeral
insertion site, incorporate it into the procedure to create an H-type
capsulotomy.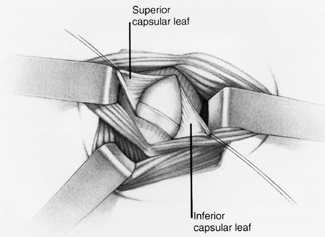 Figure 80.74.
Figure 80.74.
Open posterior shoulder stabilization procedure. Raise capsular flaps
to allow exploration of the posterior labrum. If a true posterior
Bankart lesion is present, repair it, using either a suture anchor
technique or transsosseus drill holes. (From Rowe CR, Yee LB. A
Posterior Approach to the Shoulder. J Bone Joint Surg [Am] 1944;26:580, with permission.) -
Place a spiked retractor medially along
the scapula to allow adequate visualization of the posterior labrum. If
a posterior Bankart lesion exists, repair it at this point. Prepare the
glenoid rim with a motorized burr and rasp to create a bleeding
surface. Place double-loaded (#1 nonabsorbable) suture anchors at the
2- and 4-o’ clock positions for left shoulders and at the 10- and 8-o’
clock
P.2199
positions
for right shoulders. Then repair the capsulolabral tissue with these
sutures placed in standard horizontal mattress fashion. Retain the
suture and attached needles for lateral closure of the capsulotomy. If
no Bankart lesion exists, maintain this area intact, and place sutures
directly through the labral tissue during later repair of the capsule. -
Then mobilize the inferior capsular flap in a superior and medial direction for a T-type capsulotomy (Fig. 80.75)
to reestablish tension in the IGHL. Use the previously placed
nonabsorbable sutures to secure the capsule to the glenoid surface.
Pull the superior flap inferiorly and medially to supplement the thin
capsular tissue. Suture this flap to the glenoid surface, using the
previously placed nonabsorbable sutures, as well as to the underlying
capsule (Fig. 80.76).![]() Figure 80.75.
Figure 80.75.
Open posterior shoulder stabilization procedure. Tie the inferior
capsular flap to the superomedial capsular tissue first to correct the
posteroinferior laxity. (From Rowe CR, Yee LB. A Posterior Approach to
the Shoulder. J Bone Joint Surg [Am] 1944;26:580, with permission.)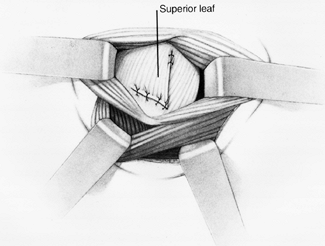 Figure 80.76.
Figure 80.76.
Open posterior shoulder stabilization procedure. Repair the superior
capsular flap to the inferomedial glenoid rim to supplement the repair.
(From Rowe CR, Yee LB. A Posterior Approach to the Shoulder. J Bone Joint Surg [Am] 1944;26:580, with permission.) -
If a lateral capsular avulsion exists and
an H-type capsulotomy has been created, also place suture anchors along
the humeral neck. Repair the medial capsulolabral tissue as previously
described, without significantly shifting the capsule. Once again,
mobilize the inferior capsular flap superiorly and laterally to
reestablish tension along the IGHL. Pull the superior flap inferiorly
as above to supplement the repair. -
Repair the infraspinatus muscle
anatomically to its insertion if it was released previously. Also
repair the horizontal split in a side-to-side fashion. If the deltoid
muscle was subperiosteally dissected from the acromion,
P.2200
reestablish the origin through transosseous drill holes. Complete the repair with nonabsorbable sutures.
with immobilization for 6 weeks. Then initiate active-assisted and
active range-of-motion exercise. Allow light muscle-strengthening
exercises (Theraband, Hygenic Corp., Malaysia) 3 months postoperatively
but no heavy contact sports or significant labor until 6 months after
the operative procedure.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
DW, Warren RF, Skyhar MJ, Ortiz G. T-plasty Modification of the Bankart
Procedure for Multidirectional Instability of the Anterior and Inferior
Types. J Bone Joint Surg [Am] 1991;73:105.
JR, Heckman MM, Guerra JJ. Diagnostic Arthroscopy of the Shoulder. In:
Mcginty JB, Caspari RB, Jackson RW, Poehling GG, eds. Diagnostic Arthroscopy of the Shoulder. Philadelphia: Lippincott–Raven Publishers, 1996:647.
RA, Wheeler JH, Ryan JB, McBride JT. Arthroscopic Bankart Repair versus
Nonoperative Treatment for Acute, Initial Anterior Shoulder
Dislocations. Am J Sports Med 1994;22:589.
FA, Feder SM, Burkhart SS, Ahrens J. The Relationship of Suture Anchor
Failure and Bone Density to Proximal Humerus Location: A Cadaveric
Study. Arthroscopy 1997;13:340.
LU, Kurzweil PR, Schwartzbach CC, et al. Inferior Capsular Shift
Procedure for Anterior-inferior Shoulder Instability in Athletes. Am J Sports Med 1994;22:578.
RB, Soslowsky LJ, Malicky DM, Palmer ML. Posterior Glenohumeral
Subluxation: Active and Passive Stabilization in a Biomechanical Model.
J Bone Joint Surg [Am] 1997;79:433.
BJ, Wubben RC, Carrera GF. Excessive Retroversion of the Glenoid
Cavity: A Cause of Non-traumatic Posterior Instability of the Shoulder.
J Bone Joint Surg [Am] 1986;68:724. [Erratum: J Bone Joint Surg [Am] 1986;68:1128.]
SS, Fox DL. Case Report: Arthroscopic Repair of a Type IV SLAP
Lesion—The Red-on-White Lesion as a Component of Anterior Instability. Arthroscopy 1993;9:488.
VP, Gagliardi JA, Murnane TG, et al. Glenohumeral Ligaments and
Shoulder Capsular Mechanism: Evaluation with MR Arthrography. Radiology 1995;196:27.
VP, Yeager TD, DeBerardino T, et al. Glenoid Labral Tears: Prospective
Evaluation with MRI Imaging, MR Arthrography, and CT Arthrography. AJR 1993;161:1229.
Laat EA, Visser CP, Coene LN, et al. Nerve Lesions in Primary Shoulder
Dislocations and Humeral Neck Fractures: A Prospective Clinical and EMG
Study. J Bone Joint Surg Br 1994;76:381.
R, Savoie FH. Arthroscopic Inferior Capsular Shift for Multidirectional
Instability of the Shoulder: A Preliminary Report. Arthroscopy 1993;9:24.
EL, Ateshian GA, Soslowsky LJ, et al. Computer Simulation of
Glenohumeral and Patellofemoral Subluxation: Estimating Pathological
Articular Contact. Clin Orthop 1994;306:28.
EL, Soslowsky LJ, Ateshian GA, et al. Shoulder Joint Anatomy and the
Effect of Subluxations and Size Mismatch on Patterns of Glenohumeral
Contact. Orthop Trans 1991;15:803.
C, Ganz R. Clinical Assessment of Instability of the Shoulder: With
Special Reference to Anterior and Posterior Drawer Tests. J Bone Joint Surg Br 1984;66:551.
SG, Bruce RA, Yacobucci GN, Torg JS. Arthroscopic Resection of Glenoid
Labral Tears in the Athlete: A Report of 29 Cases. Arthroscopy 1992;8:48.
BJ, Nirschl RP, McConnell JP, Pettrone FA. Arthroscopic Transglenoid
Suture Capsulolabral Repairs: Preliminary Results. Am J Sports Med 1993;21:656.
GI, Rockwood CA Jr. The Terrible Triad: Anterior Dislocation of the
Shoulder Associated with Rupture of the Rotator Cuff and Injury to the
Brachial Plexus. J Shoulder Elbow Surg 1995;4:51.
L, Augustini BG, Fredin H, et al. Primary Anterior Dislocation of the
Shoulder in Young Patients: A Ten-year Prospective Study. J Bone Joint Surg [Am] 1996;78:1677.
E, Berglund LJ, Grabowski JJ, et al. Superior-inferior Stability of the
Shoulder: Role of the Coracohumeral Ligament and the Rotator Interval
Capsule. Mayo Clin Proc 1998;73:508.
FW, Giangarra CE, Kvitne RS, Glousman RE. Anterior Capsulolabral
Reconstruction of the Shoulder in Athletes in Overhand Sports. Am J Sports Med 1991;19:428.
CT, Stephens S, Warren RF, Altchek DW. Arthroscopic Bankart Repair
Using a Degradable Tack: A Follow-up Study Using Optimized Indications.
Clin Orthop 1996;332:132.
JL, Chotel F, Besse JL, et al. Dynamic Anterior Jerk of the Shoulder: A
New Clinical Test for Shoulder Instability: Preliminary Study. Rev Chir Orthop Reparatrice Appar Mot 1994;80:461.
LF, Caspari RB, Savoie FH. The Arthroscopic Treatment of Posterior
Shoulder Instability: Two-year Results of a Multiple Suture Technique. Arthroscopy 1997;13:426.
GS, Foster TE, Trauner K, et al. The Thermal Properties of Bovine Joint
Capsule: The Basic Science of Laser- and Radiofrequency-induced
Capsular Shrinkage. Am J Sports Med 1997;25:670.
CS 2d, Foster CR. Inferior Capsular Shift for Involuntary Inferior and
Multidirectional Instability of the Shoulder: A Preliminary Report. J Bone Joint Surg [Am] 1980;62:897.
Brien SJ, Neves MC, Arnoczky SP, et al. The Anatomy and Histology of
the Inferior Glenohumeral Ligament Complex of the Shoulder. Am J Sports Med 1990;18:449.
Brien SJ, Schwartz RS, Warren RF, Torzilli PA. Capsular Restraints to
Anterior-posterior Motion of the Abducted Shoulder: A Biomechanical
Study. J Shoulder Elbow Surg 1995;4:298.
Connell PW, Nuber GW, Mileski RA, Lautenschlager E. The Contribution of
the Glenohumeral Ligaments to Anterior Stability of the Shoulder Joint.
Am J Sports Med 1990;18:579.
MJ, Deng XH, Warren RF, et al. Role of the Long Head of the Biceps
Brachii in Glenohumeral Stability: A Biomechanical Study in Cadavera. J Shoulder Elbow Surg 1996;5:255.
MJ, Speer KP, Altchek DW, et al. Arthroscopic Fixation of Superior
Labral Lesions Using a Biodegradable Implant: A Preliminary Report. Arthroscopy 1995;11:194.
JP, Tovey JE, Zoppi A, et al. Comparison of Arthroscopic Capsulorrhaphy
for Anterior Shoulder Instability: Stapling versus Suturing. Orthop Trans1994;17:972.
MW, Harner CD, Fu FH. The Role of the Long Head of the Biceps Muscle
and Superior Glenoid Labrum in Anterior Stability of the Shoulder. Am J Sports Med 1994;22:121.
BN, Richmond JC, Levine WN. Long-term Follow-up of Bankart
Reconstruction: Incidence of Late Degenerative Glenohumeral Arthrosis. Am J Sports Med 1995;23:538.
CR, Pierce DS, Clark JG. Voluntary Dislocation of the Shoulder: A
Preliminary Report on a Clinical, Electromyographic, and Psychiatric
Study of Twenty-six Patients. J Bone Joint Surg [Am] 1973;55:445.
CR, Zarins B, Ciullo JV. Recurrent Anterior Dislocation of the Shoulder
after Surgical Repair: Apparent Causes of Failure and Treatment. J Bone Joint Surg [Am] 1984;66:159.
FH, Miller CD, Field LD. Arthroscopic Reconstruction of Traumatic
Anterior Instability of the Shoulder: The Caspari Technique. Arthroscopy 1997;13:201.
BS, Conway J, Jobe FW, et al. Infraspinatus Muscle-splitting Incision
in Posterior Shoulder Surgery: An Anatomic and Electromyographic Study.
Am J Sports Med 1994;22:113.
CL. Soft Tissue Shortening with the Ho:YAG Laser: Experimental Model,
Structural Effects, and Histological and Ultrastructural Analysis.
Presented at the Second Annual Meeting of the Orthopaedic Laser Society
of North America and International Musculoskeletal Laser Society, South
Lake, Tahoe, CA, December, 1995.
DH. Treatment of Primary Anterior Shoulder Dislocation in Patients
Older than 40 Years of Age: Conservative versus Operative. Clin Orthop 1994;304:74.
WB, Snyder SJ, Karzel RP, et al. Long-term Clinical Follow-up of
Isolated SLAP Lesions of the Shoulder. Presented at the Annual Meeting
of the American Academy of Orthopaedic Surgeons, San Francisco, CA,
February, 1997.
SC, Matsen FA. An Approach to the Repair of Avulsion of the
Glenohumeral Ligaments in the Management of Traumatic Anterior
Glenohumeral Instability. J Bone Joint Surg [Am] 1989;71:506.
ME, Caspari RB, Asselmeier MA, et al. Arthroscopic Transglenoid
Multiple Suture Repair: 2- to 8-Year Results in 150 Shoulders. Arthroscopy 1997;13:609.
E, Lippitt S, Matsen FA. Glenohumeral Stability from Concavity
Compression: A Quantitative Analysis. Presented at the Annual Meeting
of the American Shoulder and Elbow Surgeons, Washington, DC, April,
1992.
G, Boileau P, Levigne C, et al. Arthroscopic Stabilization for
Recurrent Anterior Shoulder Dislocation: Results of 59 Cases. Arthroscopy 1995;11:173.
JJ, Johnson D, Miller M, Caborn DN. Technique for Selecting Capsular
Tightness in Repair of Anterior-inferior Shoulder Instability. J Shoulder Elbow Surg 1995;4:352.
JJ, Kann S, Marks P. Arthroscopic Repair of Combined Bankart and
Superior Labral Detachment Anterior and Posterior Lesions: Technique
and Preliminary Results. Arthroscopy 1994;10:383.
JH, Ryan JB, Arciero RA, Molinari RN. Arthroscopic versus Nonoperative
Treatment of Acute Shoulder Dislocations in Young Athletes. Arthroscopy 1989;5:213.
MM, Snyder SJ, Buford D Jr. The Buford Complex—the “Cord-like” Middle
Glenohumeral Ligament and Absent Anterosuperior Labrum Complex: A
Normal Anatomic Capsulolabral Variant. Arthroscopy 1994;10:241.