Acromioclavicular Joint Injuries
traumatic injuries that affect the shoulder. Treatment of these
injuries has been controversial and continues to evolve to this day.
Most injuries are related to falls onto the shoulder and to repetitive
use of the shoulder, such as heavy labor and athletics. This chapter
focuses primarily on the traumatic aspects of AC disorders and
describes the anatomy, classification, biomechanics, diagnosis, and
treatment of these injuries.
has been a subject of controversy from the earliest medical writings.
Hippocrates1 (460-377 BC) wrote:
this accident (for as the separated bone protrudes, the top of the
shoulder appears low and hollow), so that they may prepare as if for
dislocation of the shoulder; for I have known many physicians otherwise
not expert at the art who have done much mischief by attempting to
reduce shoulders, thus supposing it as a case of dislocation.
obviously had paid close attention to Hippocrates, because he diagnosed
his own AC dislocation received from wrestling in the palaestra. This
famous physician of the Greco-Roman period treated himself in the
manner of Hippocrates (i.e., tight bandages to hold the projecting
clavicle down while keeping the arm elevated). He abandoned the
treatment after only a few days because it was so uncomfortable. It is
appropriate that one of the earliest reported cases in the literature
was related to sports, because today participation in sports is
certainly one of the most common causes of AC dislocations.
of Aegina (7th century), dislocations of the AC joint have become
better recognized. Their treatment, however, has remained essentially
unchanged. Hippocrates1 stated that
no impediment, small or great, will result from such an injury. He
further stated that there would be a “tumefaction” or deformity, “for
the bone cannot be properly restored to its natural situation.” This
statement apparently was, has been, and will be received by the
orthopaedic community as a challenge. There is probably not another
joint in the body that has been treated in so many different ways as
the AC joint in attempts to “properly restore” it to “its natural
situation.”
changed as our understanding of the nature of the problem and the
biomechanics of the joint has developed. In 1917, Cadenat18 described the transfer of the coracoacromial ligament, which was later popularized by Weaver and Dunn.152
This remains the most commonly used and successful surgical treatment
we have today for many complete AC dislocations. Surgical treatment was
very common in the 1940s to the 1960s for complete dislocations.144
AC joint) according to older classification systems were broken down
into more detailed groupings depending on the position of the clavicle
and the degree of soft tissue injury.121
Now, treatment addresses the specific pathology involved, and many of
the injuries thought to need treatment in the past are successfully
treated with conservative measures. Treatment remains controversial in
many circumstances, as over the years numerous surgical methods have
been described.
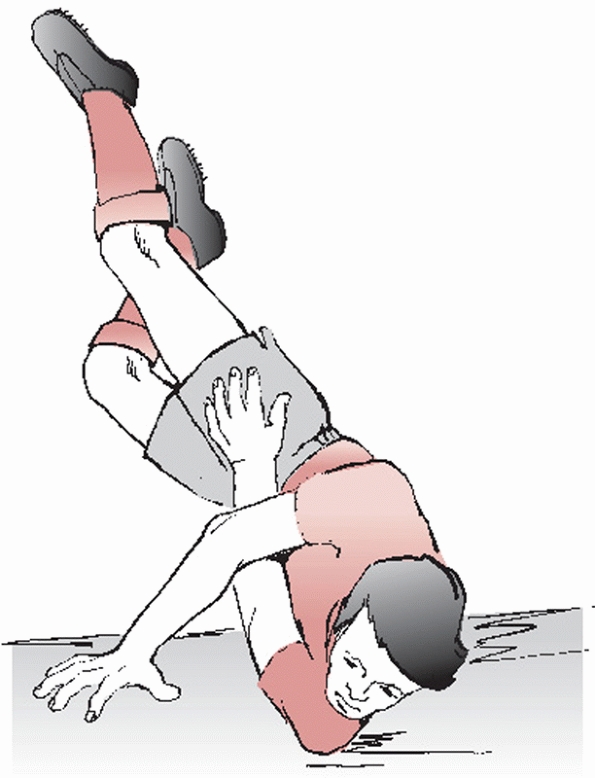
is produced by the patient falling onto the lateral aspect of the
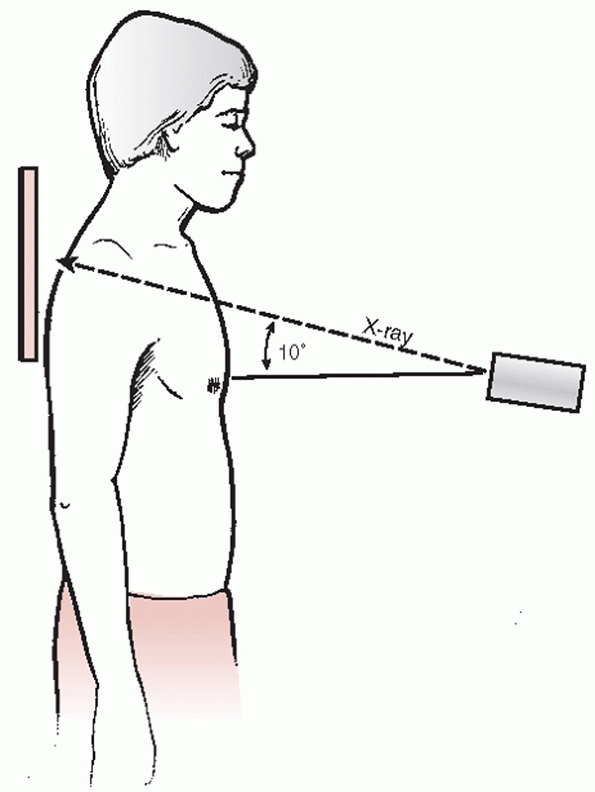
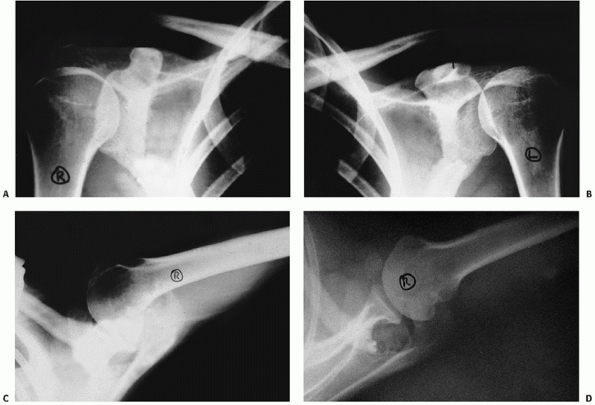
shoulder with the arm in an adducted position (Fig. 39-1). The force drives the acromion downward and medially. Bearn7
showed that downward displacement of the distal clavicle is primarily
resisted through an interlocking of the sternoclavicular ligaments. If
no fracture occurs, the force first sprains the AC ligaments (a mild
sprain), then tears the AC ligaments (a moderate sprain) and stresses
the coracoclavicular ligament, and finally—if the downward force
continues—tears the deltoid and trapezius muscle attachments from the
clavicle and ruptures the coracoclavicular ligaments (a severe AC
sprain, which completes the dislocation). At this point, the upper
extremity has lost its suspensory support from the clavicle and the
scapula displaces inferiorly.
clavicle under the coracoid is thought to be a very severe direct force
onto the superior surface of the distal clavicle, along with abduction
of the arm and retraction of the scapula.97 This type of AC joint dislocation is exceedingly rare.
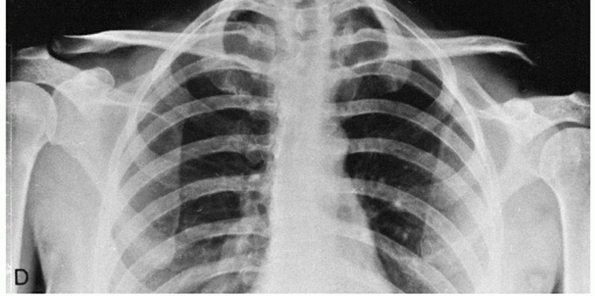
displacement of the clavicle is diagnostic of a complete AC
dislocation. Although there may be a slight upward displacement of the
clavicle by the pull of the trapezius muscle, the characteristic
anatomic feature is actually inferior displacement of the shoulder and
arm. The scapula and attached upper extremity are suspended from the
clavicle primarily by the coracoclavicular ligaments and secondarily
through the AC ligament and the surrounding musculature. Therefore,
when a severe downward force is applied to the point of the shoulder
(assuming the sternoclavicular ligaments do not rupture and the
clavicle does not fracture), the coracoclavicular ligaments rupture.
The suspension system of the scapula and attached upper extremity from
the clavicle is lost. Consequently, the arm displaces inferiorly (Fig. 39-2).
Because the weight of the arm is no longer suspended from the clavicle,
there may be a slight upward pull by the trapezius muscle on the
clavicle. However, the major deformity seen in complete AC dislocation
is a downward displacement of the shoulder.
 |
|
FIGURE 39-1 The most common mechanism of injury is a direct force that occurs from a fall on the point of the shoulder.
|
 |
|
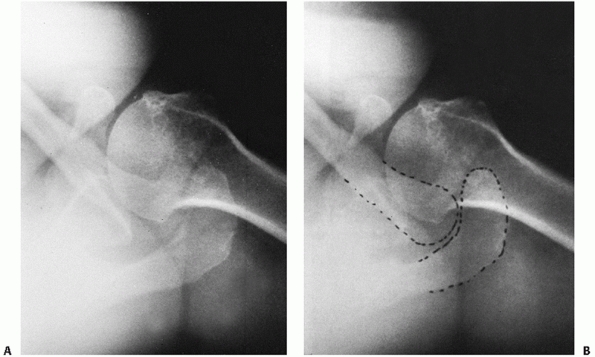
FIGURE 39-2
Anteroposterior radiograph demonstrating a chronic AC joint dislocation on the left upper extremity. Note that the clavicles are in the same position bilaterally, and the left scapula is displaced inferiorly. (From Rockwood CA, Young DC. Disorders of the acromioclavicular joint. In: Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders, 1990:434.) |
about the shoulder. Scapulothoracic dissociations are characterized by
lateral displacement of the scapula, a severe neurovascular injury, and
an injury to bone (either an AC separation, a displaced clavicle
fracture, or a sternoclavicular disruption). Scapulothoracic
dissociations are usually clinically obvious. Injuries associated with
AC separations, however, may be less obvious. The patient not only will
have pain in the shoulder but also will complain of chest pain and pain
in the periscapular and perithoracic region. Clinical examination
demonstrates the AC deformity as well as marked tenderness in the
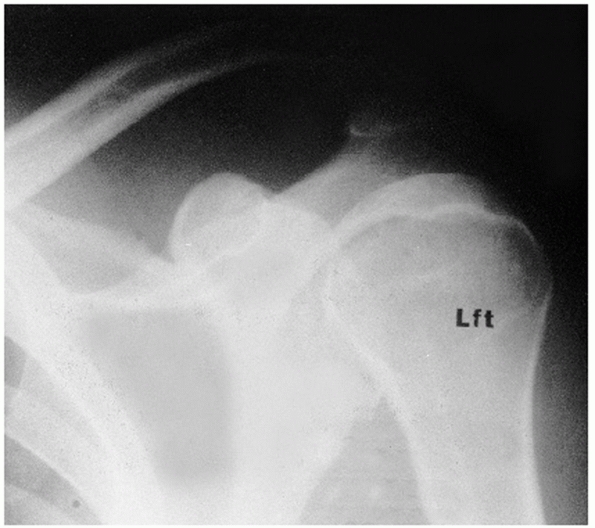
periscapular and perithoracic region. An anteroposterior chest
radiograph demonstrates an increased distance between the medial
scapular border and the midline on the affected side compared with the
unaffected side, as well as perhaps a pleural effusion. Magnetic
resonance imaging of the thorax demonstrates increased signal in the
periscapular and perithoracic muscles in addition to a pleural effusion.
fractures of the clavicle, the acromion process, the coracoid process,
and the sternoclavicular joint. Wurtz and colleagues157
reported 4 patients with a fracture of the middle third of the clavicle
and dislocation of the AC joint. Various treatment methods were used
and achieved good results in all four patients with 1- to 3-year
follow-up. Barber6 reported a
patient with a type IV AC joint injury associated with a contralateral
pneumothorax and an ipsilateral pulmonary contusion.
have reported a patient who developed a brachial plexus neuropraxia 8
years after sustaining a type III AC separation. The patient responded
well to coracoclavicular stabilization. Brachial plexus injuries
associated with AC separations are not common. Sturm and Perry,137 in a review of 59 patients with brachial plexus injuries, identified two patients with AC separations.
demonstrated that bone does indeed form in the coracoclavicular
interval. The calcification can be formed heterotopically around the
area of injury, or it can form a bridge between the coracoid and the
clavicle. Usually, it has no effect on the functional outcome.
injury or may occur in persons who have repeated stress on the
shoulder. Madsen88 reported seven
patients with the rare complication known as posttraumatic osteolysis
of the distal clavicle. He identified eight cases in the literature at
that time (1963), the first of which was reported by Werder in 1950.
Cahill19 reported 46 patients who
were athletes, none of whom had an acute injury, but 45 of whom lifted
weights as part of their training. He used technetium bone scans and a
35-degree cephalic tilt radiographic view to help make the diagnosis.
Several authors have reported this condition in women.92,99,112
and tapering of the distal clavicle. Usually, bony changes do not occur
in the acromion. Changes usually occur only in the injured shoulder. If
changes are noted in both shoulders, then other conditions should be
considered, such as rheumatoid arthritis, hyperparathyroidism, and
scleroderma. The differential diagnosis of a lesion in one shoulder
should include Gorham’s massive osteolysis, gout, and a neoplasm such
as multiple myeloma. Microscopic studies of the distal clavicle have
been reported by Murphy and coworkers104 and Madsen.88 They described demineralization, subchondral cysts, and erosion of the distal clavicle. Griffiths and Glucksman56 performed a biopsy 8 months after injury that showed patches of necrotic and reactive woven bone.
should be obtained detailing the mechanism of injury as well as a
complete discussion of patient symptoms. A complete evaluation of all
injured extremities should be documented including a neurovascular
examination. When AC joint injury is suspected, the patient should be
examined, whenever possible, in the standing or sitting position. The
weight of the arm stresses the AC joint and makes a deformity more
apparent.
tenderness and swelling over the AC joint without palpable displacement
of the joint. Usually there is only minimal pain with arm movements.
Tenderness is not present in the coracoclavicular interspace.
pain is noted at the joint. If the patient is examined shortly after
injury, the outer end of the clavicle may be noted to be slightly
superior to the acromion. Motion of the shoulder produces pain in the
AC joint. With gentle palpation, the lateral end of the clavicle is
unstable in the anterior-posterior direction. If the midclavicle is
grasped and the acromion stabilized, posterior-anterior motion of the
clavicle in the horizontal plane can be detected. There should be
little, if any, instability in the vertical plane. Tenderness is also
noted when the physician palpates anteriorly in the coracoclavicular
interspace.
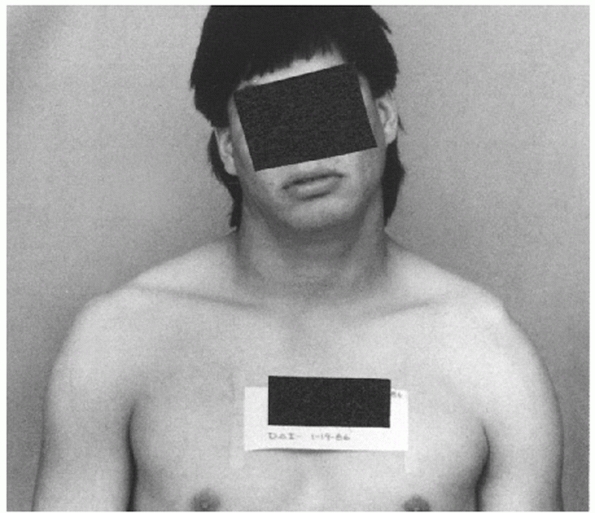
of the AC joint, characteristically presents with the upper extremity
held adducted close to the body and supported in an elevated position
to relieve the pain in the AC joint. The shoulder complex is depressed
when compared with the normal shoulder. The clavicle may be prominent
enough to tent the skin (Fig. 39-3). Moderate pain is the rule, and any motion of the arm, particularly abduction, increases the pain.
coracoclavicular interspace, and along the superior aspect of the
lateral fourth of the clavicle. The entire length of the clavicular
shaft should be palpated to detect an associated clavicle shaft
fracture. The lateral clavicle is unstable in both the horizontal and
vertical
planes.
The key to the diagnosis of a type III injury is that the defect can be
reduced with upward pressure under the elbow. A reducible injury is
differentiated from a type IV or V injury, which cannot be reduced (see
below).
 |
|
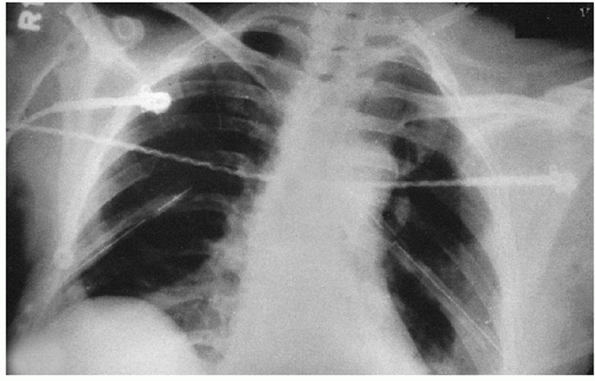
FIGURE 39-3
This patient has a complete type III dislocation of the left AC joint. The left shoulder is drooping, and there is prominence of the left distal clavicle. (From Rockwood CA, Young DC. Disorders of the AC joint. In: Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders, 1990:425.) |
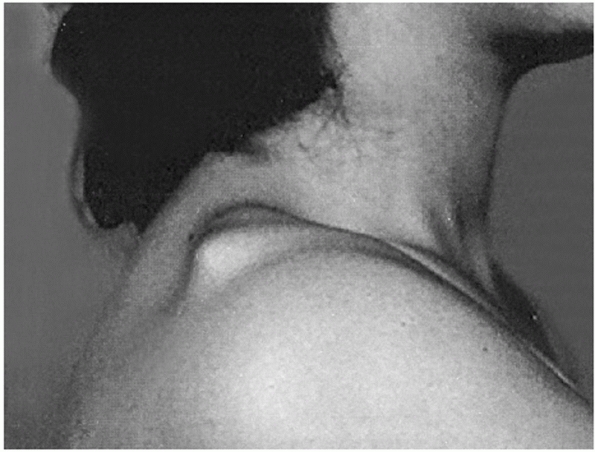
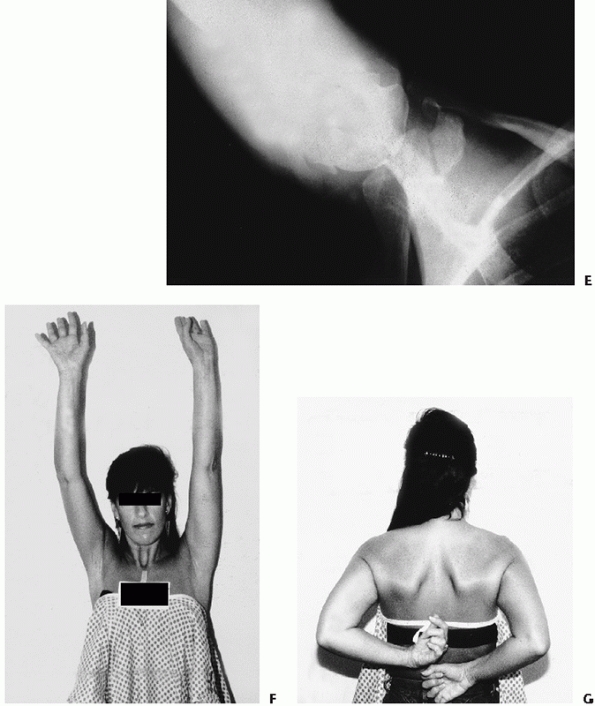
the clinical findings of a type III injury. In addition, examination of
the seated patient from above reveals that the outline of the displaced
clavicle is inclined posteriorly compared with the uninjured shoulder.
The clavicle usually is displaced so severely posteriorly that it
becomes “buttonholed” through the trapezius muscle and tents the
posterior skin (Fig. 39-4). Consequently,
motion of the shoulder is more painful than in a type III injury. The
AC joint cannot be reduced manually in this situation. The
sternoclavicular joint should always be examined for an associated
anterior dislocation.126
 |
|
FIGURE 39-4
Patient with type IV AC joint injury. Note that the distal end of the clavicle is displaced posteriorly back into and through the trapezius muscle. (From Rockwood CA, Young DC. Disorders of the acromioclavicular joint. In: Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders, 1990:446.) |
 |
|
FIGURE 39-5 A photograph of a type V AC joint dislocation demonstrating the superior displacement of the clavicle relative to the shoulder.
|
injury in which the distal end of the clavicle appears to be grossly
superiorly displaced and tenting the skin (Fig. 39-5).
This apparent upward displacement is the result of downward
displacement of the upper extremity. The patient has more pain than
with a type III injury, particularly over the distal half of the
clavicle. This is secondary to the extensive muscle and soft tissue
disruption from the clavicle that occurs with this injury. The distal
clavicle is subcutaneous and cannot be manually reduced. Occasionally,
there is so much inferior displacement of the upper extremity that the
patient will develop symptoms of traction on the brachial plexus.
the shoulder has a flat appearance, as opposed to the rounded contour
of the normal shoulder. With palpation, the acromion is prominent, and
there is a definite inferior stepdown to the superior surface of the
coracoid process. Because of the amount of trauma required to produce a
subcoracoid dislocation of the clavicle, there may be associated
fractures of the clavicle and upper ribs or injury to the upper roots
of the brachial plexus. These associated injuries may produce so much
swelling of the shoulder that the disruption of the AC joint may not
initially be recognized. Vascular injuries secondary to the dislocation
were not present in the patients presented by McPhee,97 Schwarz and Kuderna,130 and Gerber and Rockwood.54 However, all the adult cases reported by McPhee102 and Gerber and Rockwood54 had transient paresthesias before reduction of the dislocation. After reduction, the neurologic deficits resolved.
joint. Radiographs of the AC joint taken using routine shoulder
technique will be overpenetrated (i.e., dark), and small fractures may
be overlooked. Therefore, the x-ray technician must be specifically
requested to take radiographs of the “AC joint” rather than the
“shoulder.”
the patient standing or sitting, with the back against the x-ray
cassette and the arms hanging unsupported at the side. Because of
significant individual variation in AC joint anatomy and because the
coracoclavicular interspace will vary with the angle of the x-ray beam
and with the distance between the beam and the patient, both AC joints
should be imaged simultaneously on one large (14- × 17-inch) cassette.
Large patients with shoulders too broad to be visualized on a single
cassette should have radiographs made with two smaller (10- × 12-inch)
cassettes using identical technique.
the fact that with this projection, the distal clavicle and acromion
are superimposed on the spine of the scapula. Subtle fractures of the
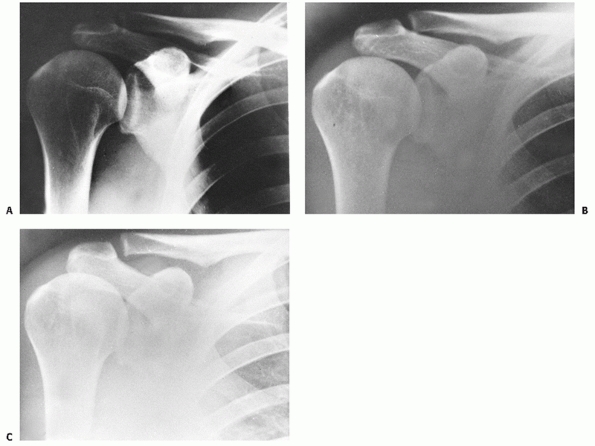
distal clavicle are easily missed. Zanca159
noted this during a review of 1000 radiographs of patients with
shoulder pain. Therefore, he recommended a 10 to 15 degree cephalic
tilt view to project an unobscured image of the joint (Fig. 39-6).
This view is now routinely used in the evaluation of AC joint injuries
and is particularly useful when there is suspicion of a small fracture
or loose body on routine views (Fig. 39-7).
 |
|
FIGURE 39-6
Position of the patient for the Zanca view—a 10- to 15-degree cephalic tilt of the standard view for the AC joint. (From Rockwood CA, Young DC. Disorders of the acromioclavicular joint. In: Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders, 1990:428.) |
plane is not sufficient to classify an AC joint injury. An axillary
lateral view should be taken of the injured shoulder when an AC
dislocation is suspected. The cassette should be placed on the superior
aspect of the shoulder and medial enough to expose as much of the
lateral third of the clavicle as possible. This will reveal any
posterior displacement of the clavicle as well as any small fractures
that may have been missed on the anteroposterior view.
the coracoid process. This injury should be suspected when there is an
AC joint dislocation on the anteroposterior projection, but the
coracoclavicular distance is normal, or equal to that on the opposite,
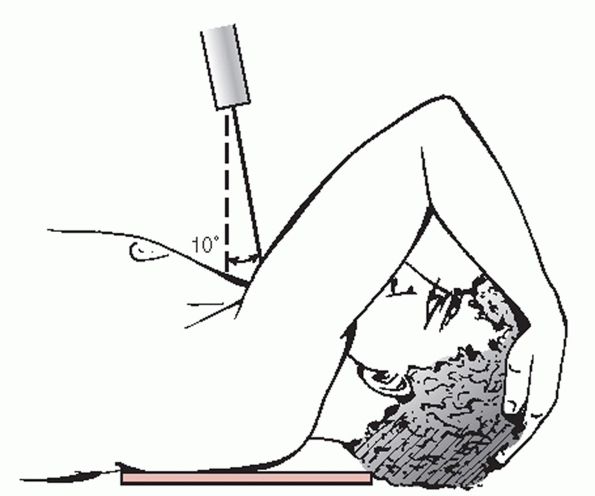
uninvolved side. A Stryker notch view taken appropriately puts the
coracoid in profile and is the best view for evaluating this injury.
This is performed with the patient supine and the arm elevated over the
head with the palm behind the head. The humerus must be parallel to the
longitudinal axis of the body, with the elbow pointed straight toward
the ceiling (Fig. 39-8).
reported the use of ultrasonography in the diagnosis of 22 cases of
type III AC dislocation. Ultrasound examination demonstrated visible
instability of the distal clavicle, incongruity of the joint, hematoma
formation, or visible ligament remnants in all cases. However, in spite
of the advent of such sophisticated imaging modalities as
ultrasonography, computed tomography (CT), and magnetic resonance
imaging, plain radiography continues to be the most readily available,
cost-effective method for routine investigation of injuries to the AC
joint.
joint in the coronal plane may vary significantly from individual to
individual. This should be remembered so that a normal variant is not
mistaken as an injury. In a study of 100 radiographs of normal
shoulders, Urist146 found that
nearly half (49%) of the AC joints were inclined superolateral to
inferomedial, with the articular surface of the clavicle overriding the
acromion; 27% were vertical, and 3% were inclined superomedial to
inferolateral, with the articular surface of the clavicle underriding
the acromion. Another 21% of the joints were incongruent, with the
clavicle lying either superior or inferior to the acromial articular
surface.
measured AC joint width radiographically in 151 normal individuals and
drew several conclusions: the AC joint space normally diminishes with
increasing age, a joint space of 0.5 mm in a patient older than 60
years is conceivably normal, and a joint space of greater than 7 mm in
men and 6 mm in women is pathologic.
significant individual variation. The average distance between the
clavicle and the coracoid process ranges from 1.1 to 1.3 cm.6 An increase in the coracoclavicular distance of 50% over the normal side
signifies a complete AC dislocation.6 Complete dislocation has been seen with as little as a 25% increase in the coracoclavicular distance.
 |
|
FIGURE 39-7 An explanation of why the AC joint is poorly visualized on routine shoulder x-rays. A.
This routine anteroposterior view of the shoulder shows the glenohumeral joint well. However, the AC joint is too dark to interpret, because that area of the anatomy has been overpenetrated by the x-ray technique. B. When the exposure usually used to take the shoulder radiographs is decreased by two thirds, the AC joint is well visualized. However, the inferior corner of the AC joint is superimposed on the acromion process. C. Tilting the tube 15 degrees upward provides a clear view of the AC joint. |
 |
|
FIGURE 39-8
Technique for taking the Stryker notch view to demonstrate fractures of the base of the coracoid. The patient is supine with a cassette placed posterior to the shoulder. The humerus is flexed approximately 120 degrees so the patient’s hand can be placed on top of the head. The x-ray beam is directed 10 degrees superior. (From Rockwood CA, Young DC. Disorders of the acromioclavicular joint. In: Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders, 1990:433.) |
the AC joint are normal, except for mild soft tissue swelling, as
compared with the uninjured shoulder. There is no widening, no
separation, and no deformity.
the clavicle may be slightly elevated. The AC joint, when compared with
the normal side, may appear to be widened. The widening probably is the
result of a slight medial rotation of the scapula and slight posterior
displacement of the clavicle by the pull of the trapezius muscle. The
coracoclavicular space of the injured shoulder is the same as that of
the normal shoulder.
dislocations, the joint is totally displaced. The lateral end of the
clavicle is displaced completely above the superior border of the
acromion and the coracoclavicular interspace is significantly (25% to
100%) greater than in the normal shoulder (Fig. 39-9). Fractures may be noted involving the distal clavicle or the acromion process.
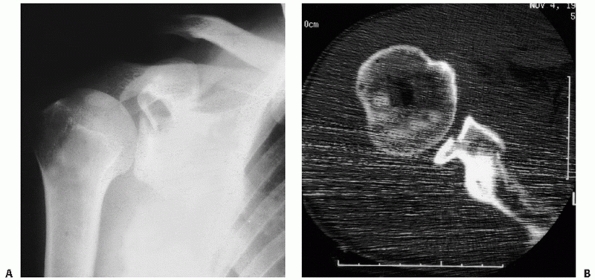
fracture of the coracoid process rather than by disruption of the
coracoclavicular ligaments. Although the fracture of the coracoid
process
is difficult to visualize on routine radiographs, its presence should
be suspected because of the presence of a complete AC separation and a
normal coracoclavicular distance, as compared with the uninjured
shoulder. The best special view for visualizing the coracoid fracture
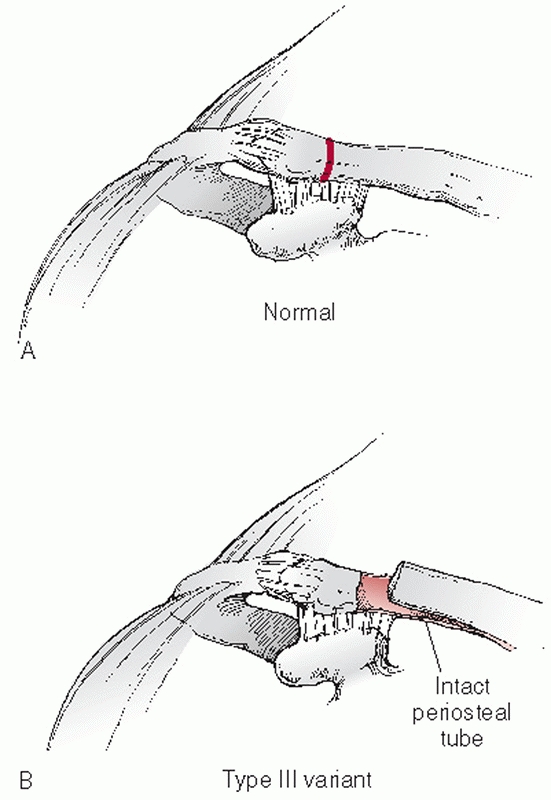
is the Stryker notch view (Fig. 39-10).
The technique for obtaining this view is described above. A few unusual
injury patterns uncommonly occur and are variations of type III
injuries. Most often, complete separation of the articular surfaces of
the distal clavicle and acromion is accompanied by complete disruption
of the AC and coracoclavicular ligaments. Children and adolescents
usually sustain a variant of complete AC dislocation. Radiographs
reveal displacement of the distal clavicular metaphysis superiorly with
a large increase in the coracoclavicular interspace. These injuries are
most often Salter-Harris type I or II injuries in which the epiphysis
and the intact AC joint remain in their anatomic locations while the
distal clavicular metaphysis is displaced superiorly through a dorsal
rent in the periosteal sleeve (Fig. 39-11).11,30,40,43,66
The lateral epiphysis of the clavicle is barely visible because it is
thin and appears and fuses over a short time period at approximately 19
years of age.
 |
|
FIGURE 39-9
X-ray appearance of a grade III injury. Not only is the right AC joint displaced compared with the left, but, more significantly, notice the great increase in the coracoclavicular interspace on the injured right shoulder compared with the normal left shoulder. |
 |
|
FIGURE 39-10
Radiographs of a patient with a type III variant injury involving the AC joint and a fracture of both the base and the tip of the coracoid. A. An anteroposterior radiograph of the injured right side. The coracoid injury is not visualized. B. A radiograph of the uninjured left side demonstrating that the coracoclavicular distance is equal on the injured and unaffected sides. C. An axillary view shows the tip fracture, but the fracture at the base is not easily detected. D. The West Point view clearly shows the fracture at the tip of the coracoid process. (continues) |
 |
|
FIGURE 39-10 (continued) E. The Stryker notch view clearly shows the fracture at the base of the coracoid. F. Nonoperative treatment in this case led to an excellent result as evidenced by full overhead elevation. G. The patient regained near-normal internal rotation.
|
reported on 25 AC injuries in children treated surgically. In all
patients younger than 13 years of age, there was a lateral
Salter-Harris clavicular fracture rather than a true AC dislocation.
The importance of recognizing this injury is that the intact
coracoclavicular ligaments remain attached to the periosteal sleeve.
Nonoperative management most often results in healing of the clavicular
fracture and thus reestablishment of the integrity of the
coracoclavicular ligaments. Those authors who recommend surgical repair
in selected instances emphasize the importance of repairing the dorsal
rent in the periosteal sleeve.40,43
complete separation of the AC articular surfaces combined with a
fracture of the coracoid process.20,76,91
This is an extremely uncommon injury. In most cases the
coracoclavicular ligaments have remained intact and attached to the
displaced coracoid process fracture, which most often occurs through
the base. There are only two reported cases of complete AC
separation—coracoclavicular ligament disruption and coracoid process
fracture.150,154 According to the authors, the mechanism of injury for this “triple lesion” is a simultaneous blow to the acromion and forcible
elbow flexion against resistance. In both of these reported cases, the patients underwent operative repair.
 |
|
FIGURE 39-11 A.
In children and adolescents, the distal clavicular physis lies medial to the AC capsular reflection. Injuries in this age group are often type II Salter-Harris fractures involving the physis rather than AC dislocations. B. The coracoclavicular ligaments remain attached to the intact periosteal sleeve while the medial clavicular fragment displaces through a dorsal periosteal rent. |
have been described for combined AC dislocation and coracoid process
fracture with intact coracoclavicular ligaments. Results seem to be
similar in both groups. Therefore, most authors recommend nonoperative
treatment. Most often, the coracoid process fracture is
extra-articular. However, we have encountered instances in which the
coracoid fragment contains a significant portion of the glenoid fossa.
The conjoined tendon rotates the coracoid process and glenoid
inferolaterally and can result in substantial articular displacement.
In this situation, open reduction and internal fixation may be
necessary and is predicated on the amount of displacement of the
articular fragment (Fig. 39-12).
 |
|
FIGURE 39-12 Coracoid fracture with intra-articular extension. A. Anteroposterior radiograph showing the fracture through the coracoid. B. A CT scan showing the glenoid displacement necessitating open reduction and internal fixation of the glenoid.
|
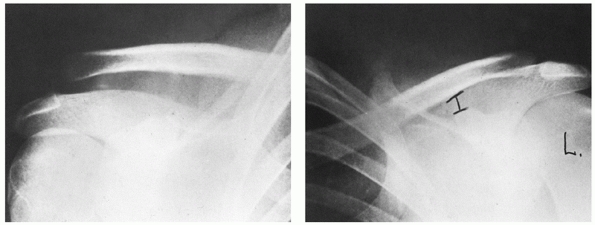
associated with a type IV injury include a relative upward displacement
of the clavicle from the acromion and an increase in the
coracoclavicular interspace, the most striking feature is the posterior
displacement of the distal clavicle, as seen on the axillary lateral
radiograph (see Fig. 39-13). In patients with
heavy, thick shoulders or in patients with multiple injuries in whom an
axillary lateral view of the shoulder or a scapular lateral
radiographic view cannot be taken, a CT scan may be of great value in
helping to confirm clinical suspicions of a posteriorly dislocated AC
joint.
of type V injuries is a marked increase (100% to 300%) in the
coracoclavicular interspace. The clavicle appears to be grossly
displaced superiorly away from the acromion (Fig. 39-14).
However, radiographs reveal that the clavicle on the injured side is
actually at approximately the same level as the clavicle on the normal
side, and the scapula is displaced inferiorly.
dislocation: subacromial and subcoracoid. In the subacromial type,
radiographs reveal a decreased coracoclavicular distance (i.e., less
than the normal side), and the distal clavicle is in a subacromial
location. The subcoracoid dislocation is characterized by a reversed
coracoclavicular distance, with the clavicle displaced inferior to the
coracoid process (Fig. 39-15). Because this injury
usually is the result of severe trauma, it often is accompanied by multiple other fractures of the clavicle and ribs.
 |
|
FIGURE 39-13 Type IV posterior dislocation of the AC joint. A. Axillary lateral radiograph of the right shoulder. B. Axillary view with the distal clavicle and acromion outlined.
|
according to the extent of damage inflicted by a given force. However,
unlike other joints, the differential diagnosis of sprains of the AC
joint is based on the severity of injury sustained by the capsular
ligaments (AC ligaments) and extracapsular ligaments (coracoclavicular
ligaments), as well as the supporting musculature (deltoid and
trapezius muscles). Therefore, injuries to the AC joint are graded
according to the amount of injury to the AC and coracoclavicular
ligaments. Injuries in this anatomic area have always been referred to
as “AC joint injuries,” although the injuries have varying degrees of
disruption between the scapula and the clavicle, not limited to the one
particular joint.
 |
|
FIGURE 39-14
An anteroposterior radiograph of a type V dislocation shows the marked increase in the coracoclavicular interspace. The clavicle appears to be grossly displaced away from the acromion. |
ability to predict prognosis or the need for surgical intervention.
Rockwood’s group154 developed the most widely accepted classification system, based on the original work of Tossy et al.144
in 1963. It is an expanded, accurate classification system based on the
anatomic severity of the injury. The modified classification is
described below and is summarized in Table 39-1 and illustrated in Figure 39-16.
 |
|
FIGURE 39-15
Type VI AC dislocation. The distal end of the left clavicle is in the subcoracoid position. The high-energy trauma causing this injury is evidenced by the bilateral chest tubes in this patient. (From Rockwood CA, Young DC. Disorders of the acromioclavicular joint. In: Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders, 1990:447. Courtesy of R.C. Erickson and D. Massillion.) |
|
TABLE 39-1 Modified Acromioclavicular Joint Injuries Classification
|
|||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||
produces a minor strain to the fibers of the AC ligaments. The
ligaments remain intact, and the AC joint remains stable.
is severe enough to rupture the ligaments of the AC joint. The distal
end of the clavicle is unstable in the horizontal plane (i.e.,
anteroposterior), but vertical (i.e., superoinferior) stability is
preserved by virtue of the intact coracoclavicular ligament. The
scapula may rotate medially, producing a widening of the AC joint.
There may be a slight, relative upward displacement of the distal end
of the clavicle secondary to stretching of the coracoclavicular
ligaments.
shoulder which tears the AC and coracoclavicular ligaments resulting in
a complete AC dislocation. The distal clavicle appears to be displaced
superiorly as the scapula and shoulder complex droop inferomedially.
Radiographic findings include a 25% to 100% increase in the
coracoclavicular space in comparison to the normal shoulder.121
clavicle, or a type IV AC dislocation, is relatively rare. The clavicle
is posteriorly displaced into or through the trapezius muscle as the
force applied to the acromion drives the scapula anteriorly and
inferiorly. Posterior clavicular displacement may be so severe that the
skin on the posterior aspect of the shoulder becomes tented. The
literature concerning posterior AC dislocations consists mostly of
small series and case reports.5,64,89,107,135 Some5,89,135 refer to this injury as a “posterior dislocation of the clavicle,” and others64,107 prefer the term “anterior dislocation of the AC joint.”
version of the type III injury. The distal clavicle has been stripped
of all its soft tissue attachments (i.e., AC ligaments,
coracoclavicular ligament, and the deltotrapezius muscle attachments)
and lies subcutaneously at the displaced AC joint. When combined with
superior displacement of the clavicle owing to unopposed pull of the
sternocleidomastoid muscle, the severe downward droop of the extremity
produces a marked disfiguration of the shoulder. Radiographically, the
coracoclavicular space is increased greater than 100% in comparison to
the opposite, normal shoulder.121
series of three patients is the largest one reported in the literature.
The injury is often the result of severe trauma and is frequently
accompanied by multiple injuries. The mechanism of dislocation is
thought to be severe hyperabduction and external rotation of the arm,
combined with retraction of the scapula. The distal clavicle occupies
either a subacromial or a subcoracoid location.
clavicle has become lodged behind an intact conjoined tendon. The AC
ligaments are disrupted in either a subacromial or subcoracoid
dislocation. The coracoclavicular ligament, however, is intact in a
subacromial dislocation and completely disrupted in a subcoracoid
dislocation. Likewise, the integrity of the deltoid and trapezius
muscle attachments depends on the degree of clavicular displacement.
retrospectively reviewed the medical records of the Massachusetts
General Hospital and found 52 AC joint injuries among 1603 shoulder
girdle injuries. Most occurred in the second decade of life. Thorndike
and Quigley141 reported AC joint
involvement in 223 of 578 athletes with shoulder injuries. AC injuries
are among the most common injuries affecting hockey and rugby players.31,35 AC dislocation is more common in males (5:1 to 10:1) and is more often incomplete than complete (approximately 2:1).
lateral end of the clavicle and the medial margin of the acromion
process of the scapula. The articular surfaces initially are hyaline
cartilage. A fibrocartilaginous disk of varying size and shape exists
inside the joint. Viewed from the anterior-posterior direction, the
inclination of the joint may be almost vertical, or it may be inclined
from downward medially, with the clavicle overriding the acromion by an
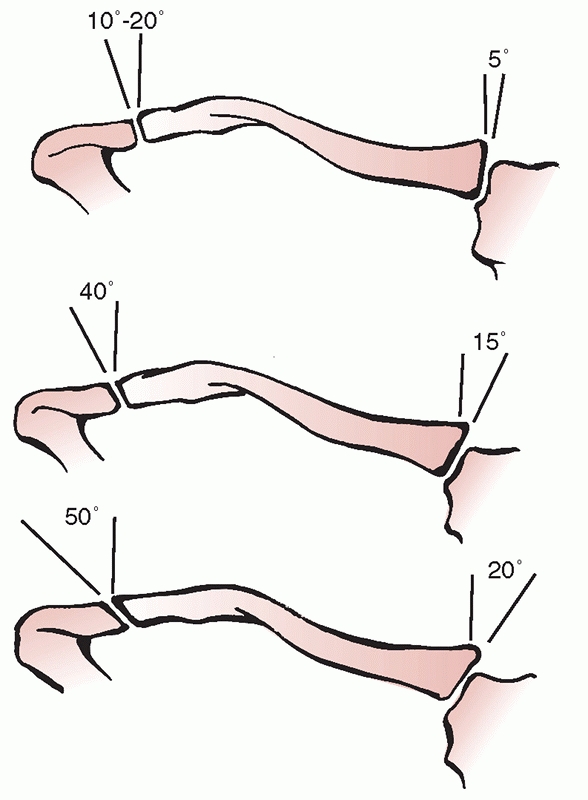
angle as large as 50 degrees (Fig. 39-17).
There may be an underriding type of inclination, with the clavicle
facet under the acromion process. The articular surface of the clavicle
overrides the articular surface of the acromion approximately 50% of
the time, and the articular surfaces are incongruent.
intra-articular disks—complete and partial (meniscoid). The disk varies
greatly in size and shape.33 With age, the meniscus undergoes degeneration until it is essentially no longer functional beyond the fourth decade.33,114,125 The nerve supply to the AC joint is from branches of the axillary, suprascapular, and lateral pectoral nerves.
above, below, anteriorly, and posteriorly by the superior, inferior,
anterior,
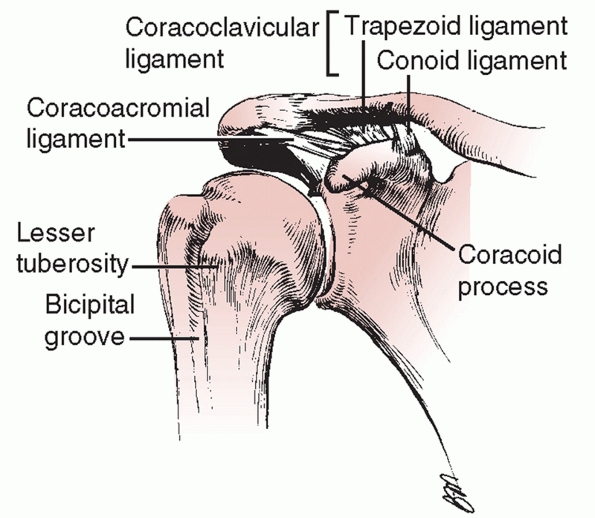
and posterior AC ligaments (Fig. 39-18).
The fibers of the superior AC ligament, which is the strongest of the
capsular ligaments, blend with the fibers of the deltoid and trapezius
muscles, which are attached to the superior aspect of the clavicle and
the acromion process. These muscle attachments are important in that
they strengthen the weak and thin ligaments, thereby adding stability
to the AC joint. The AC ligaments stabilize the joint in an
anteroposterior direction (the horizontal plane).32,125,146
Recent studies have shown the distance from the lateral clavicle to the
insertion of the superior AC ligament and capsule to range from 5.2 to
7 mm in women and approximately 8 mm in men, much less than previously
thought.13,130 An AC resection that extends medial to the capsular insertion leads to instability in the horizontal plane.12
 |
|
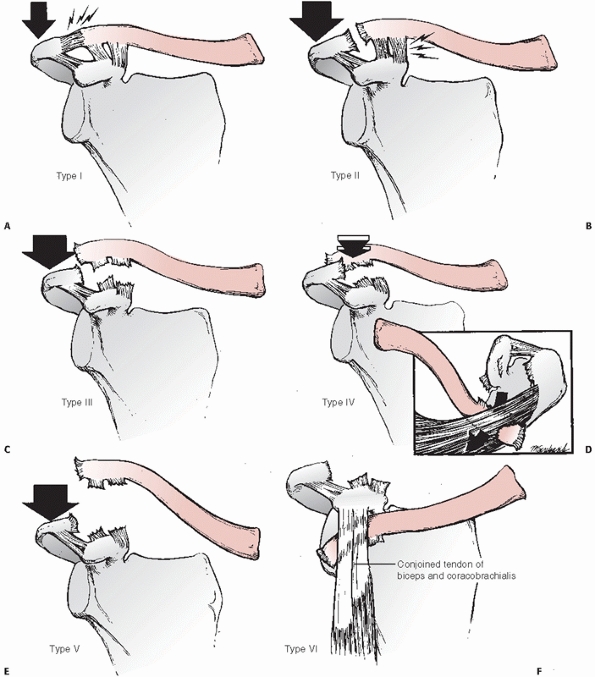
FIGURE 39-16 Schematic drawings of the classification of ligamentous injuries to the AC joint. A.
In the type I injury, a mild force applied to the point of the shoulder does not disrupt either the AC or the coracoclavicular ligaments. B. A moderate to heavy force applied to the point of the shoulder will disrupt the AC ligaments, but the coracoclavicular ligaments remain intact (type II). C. When a severe force is applied to the point of the shoulder both the AC and the coracoclavicular ligaments are disrupted (type III). D. In a type IV injury, not only are the ligaments disrupted, but the distal end of the clavicle is also displaced posteriorly into or through the trapezius muscle. E. A violent force applied to the point of the shoulder not only ruptures the AC and coracoclavicular ligaments but also disrupts the muscle attachments and creates a major separation between the clavicle and the acromion (type V). F. This is an inferior dislocation of the distal clavicle in which the clavicle is inferior to the coracoid process and posterior to the biceps and coracobrachialis tendons. The AC and coracoclavicular ligaments are also disrupted (type VI). |
 |
|
FIGURE 39-17
Variations of the inclination of the AC and the sternoclavicular joints. (Redrawn from DePalma AF. Surgery of the Shoulder. Philadelphia: JB Lippincott, 1973.) |
 |
|
FIGURE 39-18 Normal anatomy of the AC joint.
|
ligament whose fibers run from the outer, inferior surface of the
clavicle to the base of the coracoid process of the scapula. The
coracoclavicular ligament has two components: the conoid and the
trapezoid ligaments (see Fig. 39-18). A bursa
may separate these two portions of the ligament. The trapezoid ligament
measures from 0.8 to 2.5 cm in length and from 0.8 to 2.5 cm in width.
The conoid ligament varies from 0.7 to 2.5 cm in length and from 0.4 to
0.95 cm in width.125 The distance from the lateral clavicle to the lateral most fibers of the trapezoid ligament measures as little as 10 mm.13,62,63,120
shaped, with the apex of the cone attaching on the posteromedial side
of the base of the coracoid process. The base of the cone attaches onto
the conoid tubercle on the posterior undersurface of the clavicle. The
conoid tubercle is located at the apex of the posterior clavicular
curve, which is at the junction of the lateral third of the flattened
clavicle with the medial two thirds of the triangular shaft.
anterior and lateral to the attachment of the conoid ligament. This is
just posterior to the attachment of the pectoralis minor tendon. The
trapezoid ligament extends superiorly to a rough line on the
undersurface of the clavicle. This line extends anteriorly and
laterally from the conoid tubercle.
(ligamentous) stability, dynamic stability, and AC joint motion. This
has been a topic of research for many years, and recently more
sophisticated techniques in biomechanic research have elucidated the
role of the various structures about the joint.
axial skeleton is through the clavicular articulations at the AC and
sternoclavicular joints. Bearn7
stressed the importance of the sternoclavicular ligaments in supporting
the distal end of the clavicle. Through anatomic dissections and
selective divisions of the sternoclavicular ligaments, he demonstrated
how these ligaments prevent downward displacement of the distal end of
the clavicle. Hence, in the erect position, the strong sternoclavicular
ligaments support the clavicles out, away from the body, like the wings
off the body of an airplane. Furthermore, just as the jet engines are
suspended from the underside of the wings, the upper extremities are
suspended from the distal clavicles through the coracoclavicular
ligament. Thus, the coracoclavicular ligament is the prime suspensory
ligament of the upper extremity.
surrounding ligamentous structures, specifically the coracoclavicular
ligaments (conoid and trapezoid) and the AC capsule and ligaments.
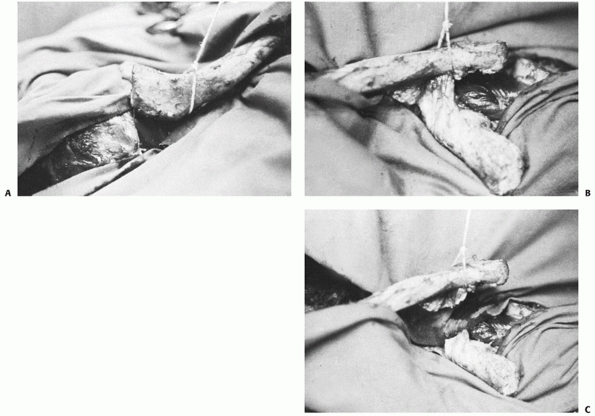
that the distal clavicle could be completely dislocated anteriorly and
posteriorly away from the acromion process following excision of the AC
joint capsule. Only after the coracoclavicular ligaments were
transected did vertical displacement of the clavicle relative to the
acromion occur (Fig. 39-19). Fukuda and colleagues48
performed load-displacement tests with a fixed displacement after
sequential ligament sectioning in order to determine individual
contributions of the various
ligaments
to AC stability. The contribution of the AC, trapezoid, and conoid
ligaments was determined at small and large displacements. At small
displacements, the AC ligaments were the primary restraint to both
posterior (89%) and superior (68%) translation of the clavicle—the most
common failure patterns seen clinically. At large displacements, the
conoid ligament provided the primary restraint (62%) to superior
translation, while the AC ligaments remained the primary restraint
(90%) to posterior translation. The trapezoid ligament served as the
primary restraint to AC joint compression at both large and small
displacements.
 |
|
FIGURE 39-19 The importance of the AC and coracoclavicular ligaments for stability of the AC joint, demonstrated in a fresh cadaver. A.
With the muscles and AC capsule and ligaments resected and with the coracoclavicular ligaments intact, the clavicle can be displaced anteriorly, as shown, or posteriorly from the articular surface of the acromion. B. However, because the coracoclavicular ligaments are intact, the clavicle cannot be displaced significantly upward. C. Following the transection of the coracoclavicular ligaments, the clavicle can be displaced completely above the acromion process. This suggests that the horizontal stability of the AC joint is accomplished by the AC ligaments, and vertical stability is obtained through the coracoclavicular ligaments. |
has a greater role in resistance to posterior displacement of the
clavicle and the conoid has a greater role in anterior displacement.82,133 The role of the AC joint capsule and ligaments has been studied extensively with respect to distal clavicle resection.15,32,45,46
Posterior abutment of the clavicle against the acromion is avoided with
only 5 mm of bone removal. This preserves the capsule and ligaments,
maintaining anteroposterior stability of the AC joint. Larger
resections have been shown to result in excessive posterior translation.12,75 Together, these experiments have led to the following conclusions:
-
The horizontal stability is controlled by the AC ligament.
-
The vertical stability is controlled by the coracoclavicular ligaments.
motion and translations that occur at the AC joint are likely to be
much more complicated than biplanar. Further work is clearly needed in
this area.
glenohumeral abduction and flexion to scapular rotation on the thorax.
Full overhead elevation cannot be accomplished without combined and
synchronous glenohumeral and scapulothoracic motion.22,70,73
As the clavicle rotates upward, it dictates scapulothoracic rotation by
virtue of its attachment to the scapula—the conoid and trapezoid
ligaments.
clavicle rotates upward 40 to 50 degrees with elevation of the shoulder.
showed that there was only 5 to 8 degrees of rotation of the clavicle
relative to the acromion. Although the clavicle rotates 40 to 50
degrees during full overhead elevation, this rotation is combined with
simultaneous scapular rotation rather than with pure AC joint motion.
This “synchronous scapuloclavicular” motion was originally described by
Codman22 and more recently by Flatow.45
position. It is important to make sure that all potential points of
pressure are well padded. A small roll or a 1 liter intravenous fluid
bag is placed under the ipsilateral scapula to bring the shoulder
forward. This allows good access to the superior aspect of the
shoulder. The skin incision is approximately 6 cm in length and is made
in Langer skin lines 2 to 3 cm medial to the AC joint. Full-thickness
subcutaneous flaps are developed medially and laterally to expose the
deltoid and trapezius aponeuroses the AC joint and the lateral 2 to 3
cm of the distal clavicle.
deltotrapezius fascia parallel to the longitudinal axis of the clavicle
in a medial-lateral orientation at the junction between the anterior
one third and the posterior two thirds of the lateral clavicle (see Fig. 39-24).
The incision starts approximately 2 to 3 cm medial to the AC joint and
extends laterally to the acromial attachment of the AC capsule. The
lateral clavicle is exposed subperiosteally by carefully elevating the
deltotrapezius fascia, periosteum, and AC capsule in one layer starting
at the medial-lateral incision and extending anteriorly and
posteriorly. In most type III injuries, the AC capsule has been avulsed
from the clavicle, leaving the acromial attachment intact. As the
anterior and posterior subperiosteal flaps are being elevated from the
lateral clavicle, the intact acromial attachment of the capsule is
preserved. The specifics to further surgical procedures will be
discussed later in the chapter.
intact AC ligaments and normal coracoclavicular ligaments. There is no
role for operative management in the acute setting.
coracoclavicular ligaments are stretched but intact. Nonoperatively
treated type I and II injuries may lead to more chronic disability than
previously recognized.29 A recent series reported by Mouhsine et al.107
found that 52% of patients with types I and II injuries remained
symptomatic at an average 6 year follow-up. Radiographic changes at the
AC joint were common.
nonoperatively. The arm should be placed in a sling for 10 to 14 days
or until the symptoms subside. This is followed by an early and gradual
rehabilitation program. With this method of treatment, the subluxation
is ignored. Heavy lifting or unprotected contact sports should be
avoided for 8 to 12 weeks to allow complete ligament healing, because a
second injury before complete ligament healing could convert the
subluxation into a complete dislocation. However, an earlier return to
sports may be facilitated by using a protective pad over the AC joint.
result of posttraumatic osteolysis of the clavicle, posttraumatic
arthritis, recurrent anteroposterior subluxation, torn capsular
ligaments trapped within the joint, loose pieces of articular
cartilage, or a detached intraarticular meniscus. Meniscal derangement
is uncommon and is characterized by displacement in and out of the
joint like a torn meniscus in the knee. The type of operative treatment
recommended for symptomatic, chronic type II injuries depends on the
cause of the persistent symptoms. Surgical options include isolated
meniscal débridement, distal clavicle excision, and AC reconstruction.
AC reconstruction is only rarely indicated in instances of persistently
painful anterior-posterior instability.
and operative methods of treatment of the complete AC dislocation have
enjoyed cyclical popularity. During the 1950s, 1960s, and 1970s,
surgical repair gained widespread popularity. In 1974, Powers and Bach117
polled all chairmen of approved residency training programs in the
United States about their treatment of complete AC injuries and
reported the following findings; the majority of program chairmen
treated type III injury by open reduction. Surgical treatment varied,
but 60% used temporary AC fixation and 35% used coracoclavicular
fixation. Nonoperative treatment was rarely advocated. As a result of
these findings, Powers and Bach117 concluded that surgical repair was the most popular method of treatment for complete AC dislocations.
A complete dislocation was described as a rupture of the
coracoclavicular ligaments, the AC ligament, the capsule of the joint,
and the fibers of the deltoid and trapezius musculature. This had been
described as a “freefloating clavicle.” This classification does not
allow distinction between complete dislocations with varying degrees of
soft tissue injury, such as disruption of AC ligaments and
coracoclavicular ligaments with and without injury to the surrounding
musculature. It was not until later that Rockwood121
introduced his classification system, distinguishing among the severity
of these injuries. This presents a problem when comparing the older
literature to the new, because in older reports, a complete
dislocation, or Tossy type III injury, likely includes what we now
consider types III, IV, and V together.
study of 1974. Cox mailed surveys to two groups of orthopaedic
surgeons: one group of 62 orthopaedic surgeons participating in the
care of athletes on a regular basis, and the second group of 231
chairmen of orthopaedic residency training programs in North America.
Fifty-one of the 59 orthopaedic surgeons in group 1 who responded
(86.4%) preferred nonoperative management of type III AC dislocations.
Of the surgeons, 30 preferred symptomatic treatment over attempts at
manual reduction. Also, 135 of the 187 orthopaedic chairmen who
responded (72.2%) preferred nonoperative management of type III
injuries, and 97 of these advocated symptomatic treatment rather than
attempts at closed manipulation. Most recently, Nissen et al.108
in 2007 presented a similar study that included a mail-in survey sent
to all members of the American Orthopaedic Society for Sports Medicine
(AOSSM) and approved Accreditation Council for Graduate Medical
Education orthopaedic program residency directors. Of the 664
respondents, 81% (71/87 AOSSM members) to 86% (502/577 directors)
continue to treat uncomplicated type III AC separations conservatively.
According to Cox27,28 and Nissen et al.,108
the current preference for treatment of type III AC injuries is
nonoperative, involves symptomatic treatment, and represents a shift
toward nonoperative treatment since the Powers and Bach117 survey of 1974.
reported good to excellent results in the vast majority of patients
treated conservatively in both type II and type III (complete)
injuries. Dias et al.34 followed 44
patients with a complete dislocation for 5 years. At that point,
results were satisfactory in all the patients. In 1996, at an average
of 12.5 years after injury, 30 of the original 44 patients were again
reviewed.119 All had a good outcome.
The results of nonoperative treatment were equal if not superior to
those of operative treatment. The nonoperative group had earlier return
to work and sports. In a review of all AC injuries, Post116 stated that almost all type III AC dislocations could be treated without operative intervention. Taft et al.139
compared a group of patients treated nonoperatively with sling, taping,
or a Kenny-Howard sling to a group treated operatively with AC or
coracoclavicular fixation. Subjective ratings of pain and stiffness and
objective ratings of strength and range of motion were similar in both
groups. There was a much higher complication rate in the operative
group. Press and colleagues118 found
benefits to both operative and nonoperative treatment, but earlier
return to work and sports with nonoperative treatment. There were no
significant differences with respect to shoulder range of motion,
manual muscle strength, and neurovascular findings between the two
groups.
versus operative treatment for AC dislocations have been performed. One
of the few was by Larsen et al.,81
who compared conservative treatment to operative treatment with AC
fixation using two 2-mm threaded Kirschner wires across the joint. The
rehabilitation period was significantly shorter with nonoperative
treatment, and after 13 months there was no difference in the clinical
results. They recommended operative treatment in thin patients who have
a prominent lateral end of the clavicle, in those who do heavy work,
and in patients whose work requires that the shoulder be held in
abduction and flexion quite often.
in which nonoperative treatment was compared to fixation with a
coracoclavicular screw. Conservatively treated patients regained
movement significantly more quickly and fully, returned to work and
sports sooner, and had fewer unsatisfactory results than those having
early operation. In patients with a severe dislocation, defined as
having displacement of greater than 2 cm, however, early surgery
produced better results. Bannister et al.4
later established a classification based on radiographic analysis.
Injuries in which the clavicle was displaced 2 cm or more were
associated with detachment of the origin of the anterior deltoid. These
patients benefited from early surgery.
difference in patients when compared to the opposite side with complete
AC separations who were treated nonoperatively.87,118,142,149,156 Wojtys and Nelson’s156
study is unique in that both strength and endurance were tested.
According to their study, both strength and endurance were comparable
to the noninjured side. However, there was a trend (not statistically
significant) toward a decrease in the expected strength and endurance
advantage on the dominant shoulder in patients whose dominant shoulder
was injured.
surveyed 42 team orthopaedists representing all major league baseball
teams to ascertain their treatment for a hypothetical starting rotation
pitcher who had sustained a grade III AC joint separation 1 week before
the start of the season. Twenty-nine (69%) reported they would treat
the injury nonoperatively, while 13 (31%) stated they would operate
immediately. Twenty (48%) of the physicians reported treating a total
of 32 such injuries in baseball players. Twenty (62.5%) were treated
nonoperatively, and 12 (37.5%) were treated operatively. There was not
a major difference in outcome between the two groups.
showed that a displaced AC joint injury in a polytrauma patient has a
greater effect on shoulder function than isolated AC joint injuries
when evaluated by both disease-specific and general health outcomes.
Standard treatment methods may be inadequate in this population.
dislocation is still somewhat controversial, although the majority of
current reports support nonoperative treatment. When reading the
literature, one must consider that in most comparison studies between
operative and nonoperative treatment the type of surgery varies. Rarely
is there consistency between study groups and methods. In most patients
with type III injuries, excellent functional results can be obtained
with nonoperative management. Younger, more active patients with more
severe degrees of displacement and laborers who use their upper
extremity above the horizontal plane may benefit from operative
stabilization.
AC dislocation have been reported including adhesive strapping, slings,
bandages, braces, traction, pressure dressings, and plaster casts. Most
commonly, patients are treated with short-term sling support followed
by early range of motion. Devices used to maintain reduction by closed
means are rarely used. They cause the patient much discomfort and have
never proven to maintain the reduction. There is also no correlation
between residual deformity and outcome.139
Nonoperative treatment more commonly consists of short-term (1 to 2
weeks) sling support, symptomatic treatment with nonsteroidal
anti-inflammatory medication, and early mobilization. Schlegel et al.128
prospectively followed a group of acute type III injuries, with 80%
favorable results. Of the 20 patients evaluated 1 year after injury, 4
felt their results were suboptimal. There was no difference in range of
motion in any of the patients. Strength tests revealed equal strength
between sides in all but the “bench press,” which revealed a 17%
decrease on the injured side.
During the 1800s and early 1900s, practically every conceivable
operation for AC dislocation was performed. These procedures included
AC repairs, coracoclavicular repairs, combined
AC
and coracoclavicular repairs, coracoclavicular fusion, and dynamic
muscle transfers using the tip of the coracoid process and attached
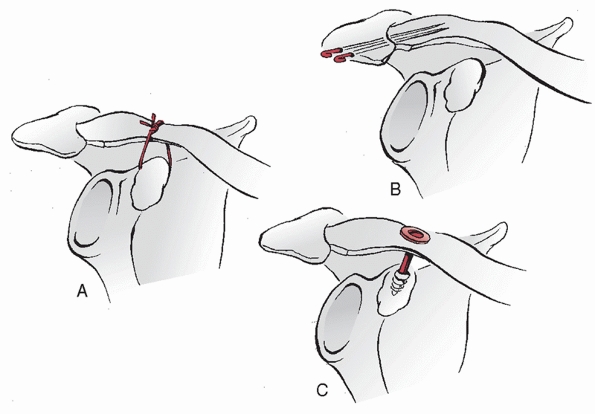
conjoined tendon.* Currently, the most popular methods of stabilization are coracoclavicular or intra-articular (i.e., AC) repairs (Table 39-2). Many of the specific procedures used today are combinations or modifications of previously described procedures (Fig. 39-20).
|
TABLE 39-2 Pros and Cons of Operative Treatment Options for Acromioclavicular Joint Dislocations
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
commonly used techniques employ some type of coracoclavicular fixation
or reconstruction. However, many methods using intra-articular fixation
are described in the literature. One should be cautious in using these
techniques, as the placement of hardware across the AC joint can be
problematic.
advocate the use of two 1.8-mm percutaneous Kirschner wires to
stabilize the joint, and they emphasized repair of the damaged deltoid
and trapezius. These pins can be inserted from the lateral edge of the
acromion through the joint and into the clavicle or from the joint out
through the acromion and then back across the joint into the clavicle.
Fama and Bonaga44 reported the use
of a smooth wire inserted laterally in the acromion, through the AC
joint, out the posterior cortex of the clavicle, and through the skin
posterior to the clavicle. The wire was then bent back on itself to
meet the other end of the wire. The two ends were then fastened
together like a safety pin to prevent migration. It must be emphasized
that despite the fact that the pin is bent, it can break, migrate, and
create serious consequences. (The section on complications, below,
discusses pin migration to the spinal cord, lung, subclavian artery,
pulmonary artery, mediastinum, heart, and other areas.)
 |
|
FIGURE 39-20 Various operative procedures for injuries to the AC joint. A. Suture between the clavicle and the coracoid process. B. Steinmann pins across the AC joint. C. A lag screw between the clavicle and the coracoid process.
|
They performed a prospective, randomized trial in 100 patients using
three types of AC fixation: (a) smooth pins, (b) threaded pins, and (c)
cortical screws. Thirteen of the 86 patients available for review
developed symptomatic osteolysis of the distal clavicle. Eight of the
13 cases of osteolysis occurred among the 25 patients who underwent
cortical screw fixation. In a 4-year follow-up on 70 of the 100 cases,
the results were graded as good in 67 of the 70 patients.42 These authors preferred the use of the threaded Kirschner wires.
authors report the use of other procedures as an adjunct to AC
fixation. Neviaser106 introduced
superior AC ligament reconstruction through transfer of the coracoid
attachment of the coracoacromial ligament to the superior aspect of the
clavicle. He did not
recommend repair of the coracoclavicular ligament. Ho and colleagues69
advocated reconstruction of the superior AC ligament using the
coracoacromial ligament and reconstruction of the coracoclavicular
ligament using Marlex tubing passed inferior to the coracoid and over
the clavicle. These procedures were done alone or in combination.
Paavolainen et al.113 described AC fixation in combination with AC and coracoclavicular ligament repair.
This technique has a high complication rate, and a second procedure is
always required to remove the plate. This plate does not offer any
benefit over more commonly used procedures.
of placing a screw between the clavicle and the coracoid was described
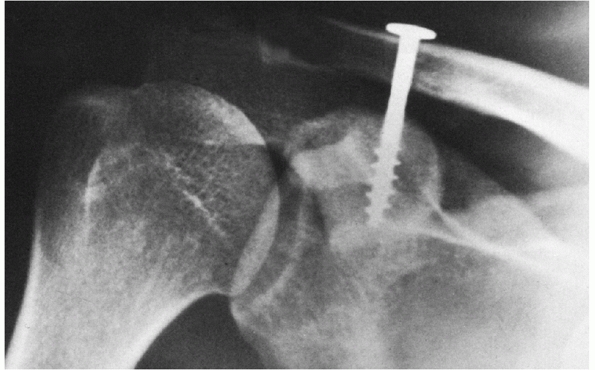
by Bosworth14 in 1941. The screw was placed percutaneously, using local anesthesia and fluoroscopic guidance (Fig. 39-21).
With the patient in a seated position, a stab wound was made on the
superior aspect of the shoulder, 3.8 cm medial to the distal end of the
clavicle. After a drill hole was made in the clavicle, an assistant
reduced the AC joint by depressing the clavicle and elevating the arm
using a special clavicledepressing instrument. An awl was used to
develop a hole in the superior cortex of the base of the coracoid
process, which was visualized using fluoroscopy. A regular bone screw
was then inserted. The screw was left indefinitely, unless specific
indications for removal developed. Bosworth14 did not recommend either repair of the coracoclavicular ligaments or exploration of the AC joint. Bosworth14 also developed a lag screw with a broad head, which he preferred to the original regular bone screw.
in 1989, who placed a guide pin fluoroscopically from the clavicle to
the coracoid process. After adequate positioning of the pin within the
coracoid had been confirmed radiographically, a cannulated drill bit
and screw were sequentially passed over the guide pin. Tsou145
reported a 32% technical failure rate in 53 patients with complete AC
dislocation using this technique. Accurate insertion of the screw is
difficult to perform percutaneously. Furthermore, the percutaneous
technique does not allow coracoclavicular ligament repair, deltoid and
trapezius reattachment, or AC joint débridement.
 |
|
FIGURE 39-21
Postoperative anteroposterior radiograph of the shoulder with a Bosworth screw in place. Note that the AC joint has been reduced and the coarse lag threads of the screw are well seated into the coracoid process. |
presented a technique for the chronic, symptomatic dislocated AC joint
in which the coracoacromial ligament was transferred from its acromial
insertion into the medullary canal of the clavicle, along with
temporary placement of a coracoclavicular screw to stabilize the
clavicle until the ligament healed. The screw is usually removed 8
weeks postoperatively, necessitating a second procedure. A
bioabsorbable screw may afford comparable strength to a steel screw,140 and may obviate the need for removal.
utilized a double Dacron velour ligament for fixation in a prospective
study in 28 consecutive patients with a mean follow-up of 5.1 years;
71% had good or excellent results. There was little correlation between
the end result and the degree of residual dislocation, coracoclavicular
ossification and posttraumatic arthritic changes, or osteolysis of the
distal clavicle. Browne and associates17 used 5-mm Mersilene (Ethicon, Somerville, NJ) tape for coracoclavicular fixation. Morrison and Lemos101
reported 12 of 14 good and excellent results when using a synthetic
loop placed through drill holes in the base of the coracoid and the
anterior third of the clavicle.
Most of these authors also reported AC joint débridement, AC joint
ligament repair or reconstruction, coracoclavicular ligament repair,
and imbrication of the deltotrapezius fascia—either alone or in
combination—in addition to the coracoclavicular fixation.
procedures accepted today involve ligament reconstruction with or
without augmentation with suture, tape, or hardware. The recent
literature has focused on anatomic coracoclavicular reconstruction to
more closely reproduce the intact ligamentous state, thus enhancing
stability.26,57,94,95 Costic et al.26
found that anatomic coracoclavicular reconstruction more closely
approximates the stiffness of the native ligamentous state than does a
standard Weaver-Dunn repair. Mazzocca et al.95
performed a biomechanic cadaver study comparing an anatomic
coracoclavicular ligament reconstruction using a semitendinosis graft
to
a
modified Weaver-Dunn procedure and an arthroscopic technique using
nonabsorbable suture material. Specimens were tested with a
directionally applied force (anterior, posterior, and superior) as well
as cyclic loading and load to failure to simulate physiologic states at
the AC joint. These were compared to the intact ligamentous state.
Results showed the anatomical coracoclavicular ligament reconstruction
had significantly less anterior and posterior translation when compared
to the other forms of reconstruction.95 Superior displacement during cyclic loading was equal among the groups.95
They concluded that anatomic ligamentous reconstruction more closely
approximated the intact state, thus providing more stability than the
other two forms of reconstruction. A similar study by Grutter et al.57
also showed superior biomechanic results of anatomic ligament
reconstruction when compared to a modified Weaver-Dunn technique when
specimens were loaded to failure in the coronal plane. The authors
further concluded that anatomic reconstruction recreated the tensile
strength of the intact state when a flexor carpi radialis tendon was
used.57
distal clavicle in a type IV injury, and the gross superior
displacement in the type V injury, most authors recommend surgical
repair.107,135
The posterior displacement of the clavicle into the trapezius in a type
IV injury will lead to discomfort with motion. Therefore, surgical
reduction of the deformity and stabilization of the clavicle are often
necessary. The posterior displacement produces significant stripping of
the deltotrapezial fascia from the distal clavicle. Its repair at the
end of the stabilization procedure is a crucial step in augmenting
distal clavicular stability.
stabilization because they result in significant deltotrapezial
stripping and resultant gross instability, which commonly leads to
chronic pain and disability. Again, meticulous repair of the
deltotrapezial fascia augments the repair.111
Initial attempts at closed reduction failed. In one instance, after
open reduction by lateral retraction of the scapula, the clavicle was
stabilized by suturing the deltoid and trapezius muscle avulsion and by
repairing the AC joint capsule. In one patient, whose shoulder was
operated on 2.5 months after injury, a Steinmann pin was used to
stabilize the AC joint. After immobilization for 3 to 5 weeks, both of
these patients had almost full range of motion and good power. One
patient with a recurrent subcoracoid dislocation was treated by
excision of the distal 1 cm of the clavicle, and at 5-year follow-up
the patient had no complaints or weakness. Gerber and Rockwood54
reported on using the extra-articular technique with a coracoclavicular
lag screw combined with repair of the ligaments and imbrication of the
deltotrapezius fascia over the top of the clavicle.
is not a common injury in adults. The mechanism of injury may be
essentially the same as for a type III AC dislocation, except the
coracoclavicular ligaments do not fail and a fracture occurs through
the base of the coracoid, allowing relative upward displacement of the
distal clavicle. It is important to recognize that, in order for the
coracoid fracture to be responsible for the AC displacement, the
fracture must occur through the base. If the fracture occurs at the tip
of the coracoid process, either concomitant coracoclavicular ligament
injury or a second fracture through the coracoid base has occurred,
allowing displacement of the AC joint (see Fig. 39-10).
The isolated coracoid tip fracture, when it occurs in conjunction with
an AC dislocation, is thought to result from a sudden pull on the
coracoid process by the conjoined tendons.150
recognize, and it is important that good radiographs be obtained to
look for this injury before surgical management. Although the axillary
radiographic view can suggest a fracture of the coracoid process, the
Stryker notch view or the CT scan can best indicate the site and degree
of displacement of the fracture (see Fig. 39-12).
of the coracoid base with intact coracoclavicular ligaments is
difficult. Therefore, the need for surgery is one of the few
indications for placement of pins across the AC joint. If the fracture
involves the tip of the coracoid and there is significant displacement,
then screw fixation may be indicated for the coracoid fracture and the
AC joint may be stabilized by a coracoclavicular loop.150
Conversely, fibrous unions of the tip of the coracoid process are often
asymptomatic. Consequently, a combined AC dislocation and fracture of
the tip of the coracoid process may be treated nonoperatively using
methods similar to those prescribed for isolated type III injuries.
reported 4 cases of combined AC dislocation and fracture of the
coracoid base and reviewed 13 cases from the literature. They concluded
that although surgery could produce good results, equally satisfactory
function and minimal residual deformity could be achieved by
immobilization of the shoulder in a sling for 6 weeks. Kumar76 had good short-term success with conservative treatment as well.
The meniscus and articular cartilage often sustain an injury that leads
to these degenerative changes. Chronic pain after types I and II
injuries is treated with mild analgesics such as nonsteroidal
anti-inflammatory medication, avoidance of painful activity or
positions, and intra-articular injection with corticosteroid
preparations. Many will resolve with this conservative treatment.
to conservative care may require operative excision of the distal
clavicle to provide relief of pain. This can be performed using an open
or an arthroscopic technique.47,51,52,58,103,134
The important aspect of either technique is preservation or repair of
the AC joint capsule to maintain anteroposterior stability of the joint.15
the initial conservative regimen is the same as for type I injuries. If
conservative, symptomatic treatment fails, surgery may be indicated.
Isolated distal clavicle excision after a type II injury may fail
because of anteroposterior instability of the distal clavicle and
resultant posterior abutment of the clavicle on the scapular
spine.
Therefore, the patient should be examined carefully for increased
anteroposterior translation of the clavicle relative to the acromion
during surgical planning. If indeed, anteroposterior instability
exists, distal clavicle excision may be combined with AC capsular
reconstruction or coracoacromial ligament transfer.152
dislocations (types III, IV, and V) should not be treated with isolated
distal clavicle excision. This merely shortens the clavicle without
stabilizing it and is often associated with persistent postoperative
symptoms. Therefore, distal clavicle excision should be combined with
stabilization in chronic, symptomatic, complete AC injuries. The most
popular reconstructive procedure is transfer of the acromial attachment
of the coracoacromial ligament to the resected surface of the distal
clavicle and concurrent coracoclavicular stabilization.
Coracoclavicular stabilization greatly increases the strength of the
construct.36,59,62,63,77,78,118,131,142,151,153
rest. The application of an ice bag for the first 12 to 24 hours,
whenever convenient, will help to ease the discomfort. A sling can be
worn to support the arm and to remind the patient and others that the
shoulder is injured. We encourage the patient to rest the shoulder and
to resume a normal range of motion as the symptoms subside. Heavy
stresses, lifting, and contact sports should be delayed until there is
a full range of motion and no pain to joint palpation. This usually
takes 2 weeks.
arthritis develops late as a result of a prior type I AC injury.
Surgery is also indicated after a type I injury in the absence of
radiographic degenerative findings when internal derangement of the
joint is suspected as the etiology of pain. If the patient has failed 3
to 6 months of nonoperative treatment (e.g., nonsteroidal
anti-inflammatory medication, rest, activity modification,
corticosteroid injections), distal clavicle excision is recommended.
This can be performed using either open or arthroscopic techniques.72
Overzealous excision of bone should be avoided in order to preserve the
AC ligaments. We prefer arthroscopic excision of 0.5 to 0.7 cm of bone.13,120
ice pack is used during the first 12 to 24 hours. The patient is given
a sling to rest and support the arm. The sling is worn for 1 to 2
weeks, depending on the age of the patient, the symptoms, and the
circumstances. We encourage the patient to begin gentle range-of-motion
exercises of the shoulder and allow use of the arm for dressing,
eating, and necessary activities of daily living when symptoms permit,
which is usually on about the seventh day. The typical patient is
instructed not to use the shoulder for any heavy lifting, pushing,
pulling, or contact sports for at least 6 weeks. We do not want the
patient to have another injury or stress the AC joint to convert a type
II problem to a type III problem. However, earlier return to athletics
can be facilitated through the use of protective padding over the
superior aspect of the joint. For the average patient who only
occasionally puts stress on the AC joint, the development of chronic
problems is uncommon and usually can be resolved with anti-inflammatory
drugs, moist heat, and judicious use of intra-articular corticosteroids.
II AC injuries. However, patients with symptomatic chronic type II
injuries that have not responded to 3 to 6 months of nonoperative
treatment are surgical candidates. If the primary complaint is pain,
radiographs reveal AC arthritis with a normal coracoclavicular
distance, and the pain is relieved with intra-articular injection of a
local anesthetic, we prefer isolated distal clavicle excision. Although
this can be accomplished by open as well as arthroscopic means,
arthroscopic excision allows for relative preservation of the soft
tissue envelope surrounding the distal clavicle and AC joint (i.e., the
deltotrapezius fascia and the AC capsule). Arthroscopic distal clavicle
excision can be performed by the direct superior approach.46
However, the subacromial approach is easier and more familiar to most
surgeons. It also allows inspection of the bursal side of the rotator
cuff.72 Regardless of the operative
technique utilized, however, excision of excessive amounts of bone may
result in symptomatic anteroposterior subluxation. Therefore, excision
is limited to 0.5 to 1.0 cm.
joint débridement without distal clavicle excision is rarely indicated.
It is unlikely that the meniscus could be damaged without some injury
occurring to the articular surfaces. Furthermore, patients with no
radiographic degenerative changes and chronic pain and tenderness over
the AC joint following a type II AC injury most commonly will
demonstrate anteroposterior subluxation and be candidates for AC
reconstruction.
late complication of an acute type II AC subluxation can be very
subtle. Moreover, the decision to perform surgical reconstruction of
the AC ligaments, as opposed to an isolated distal clavicle excision,
can be a difficult one. If the patient presents years after the
original injury, the type of AC injury originally sustained may not be
obvious. If the joint reveals advanced degenerative changes, with large
periarticular osteophytes, increased anteroposterior translation may
not be demonstrable on physical examination. Under these circumstances,
particularly if the coracoclavicular distance is radiographically
normal, isolated arthroscopic distal clavicle excision may be
indicated. However, if anteroposterior translation is increased
compared to the normal side, AC reconstruction is a better choice.
combined with distal clavicle excision. Transfer of the acromial
attachment of the coracoacromial ligament into the medullary canal of
the resected distal clavicle is most commonly
performed
for correction of superoinferior instability associated with chronic
disruption of the coracoclavicular ligaments. However, it can also be
used to correct recurrent anteroposterior subluxation associated with
chronic AC capsular disruption. The traditional technique is modified,
however, so that the coracoacromial ligament is transferred to the
posterior corner of the resected clavicle, rather than to the center of
the medullary canal. This places the transferred ligament in a more
anteroposterior orientation, which theoretically provides better
resistance to anteroposterior translation.
not known. However, subsequent development of rotator cuff
insufficiency in a patient who has undergone coracoacromial ligament
transfer potentially could result in anterosuperior subluxation of the
glenohumeral joint. Therefore, prior to transferring the coracoacromial
ligament, we attempt to perform plication of the AC joint capsule. If
the capsular repair is stable, we forgo coracoacromial ligament
transfer.
incision is made in Langer’s lines approximately 1.5 to 2.0 cm medial
to the AC joint (Fig. 39-22). Full-thickness
subcutaneous flaps are developed medially and laterally to expose the
AC joint, deltoid and trapezius aponeuroses, and the distal 2 cm of the
lateral clavicle. With care, it is possible to separate the deltoid and
trapezius aponeuroses from the underlying posterior, superior, and
anterior AC capsule. The AC capsule is then exposed by sharply,
individually dissecting the deltoid and trapezius away from the capsule
and distal clavicle.
the capsule into the articular space. The periosteum of the lateral
clavicle is scored with an electrocautery perpendicular to the long
axis of the clavicle approximately 1.5 cm medial to the joint line. The
AC capsule is then incised in a medial to lateral direction at the
midportion of the joint. The clavicular attachment of the capsule along
with the periosteum up to the previously placed score mark are sharply
elevated with a #15 scalpel in one continuous layer. This detachment
starts at the medial-lateral capsular incision and continues anteriorly
and posteriorly to expose the AC joint and distal clavicle. Typically,
the capsule remains strongly attached to the acromion. Additionally,
the capsule is usually redundant anteriorly and posteriorly because of
recurrent anteroposterior subluxation.
microsagittal saw and an osteotome. Our goal is to resect 0.5 to 1.0 cm
of bone with as little disruption of the inferior capsule as possible.
Therefore, a small drill is used to perforate the distal clavicle in
two or three places. A microsagittal saw is then used to saw through
the clavicle up to the inferior cortex. An osteotome is placed in the
osteotomy site and twisted. This will crack the inferior cortex through
the previously placed drill holes. The lateral fragment is excised and
a power burr is used to smooth the cortical margins of the resected
distal clavicle.
they are of adequate quality and length to plicate and reattach to the
resected distal clavicle. If the capsule is of sufficient quality and
will reach to the resected surface of the distal clavicle, a series of
four small, unicortical drill holes are made along the lateral margin
of the resected distal clavicle approximately 2 to 3 mm from the edge.
Nonabsorbable sutures are passed through these drill holes and exit the
medullary canal just inferior to the superior cortical surface. The
posterior capsular flap is shifted anteriorly and sutured to the edge
of the distal clavicle with the two most posterior sutures; the
anterior capsular flap is shifted posteriorly and sutured to the edge
of the distal clavicle using the two most anterior sutures. After the
knots are tied, the free ends of the most anterior and posterior
sutures are used to reattach the reflected deltoid and trapezius
aponeuroses, respectively. The excess suture is then excised.
plication and secure reattachment to the resected surface of the distal
clavicle, the acromial attachment of the coracoacromial ligament must
be transferred (Fig. 39-23). A small portion of
the anterior deltoid is released from the anterior acromion to expose
the acromial attachment of the coracoacromial ligament. The ligament is
then released from the acromion and mobilized distally to its
attachment on the coracoid process. Two sutures are placed in the free
end of the ligament. Two unicortical drill holes are placed in the
posterosuperior surface of the distal clavicle. These drill holes exit
the medullary canal of the clavicle and are oriented from a
posterosuperior to an anteroinferior direction. The coracoacromial
ligament sutures are then passed through these clavicular drill holes
and tied over the posterosuperior cortical bridge. Additional drill
holes are placed along the superior and anterosuperior surfaces of the
clavicle for reattachment of the deltoid and trapezius aponeuroses.
the method of reconstruction. The arm is immobilized in an abduction
orthosis or abduction pillow for 3 weeks. Pendulum and passive external
rotation exercises are then initiated and continued for 2 to 3 weeks.
The arm continues to be supported in the abduction pillow or orthosis
until 5 to 6 weeks postoperatively. Passive mobilization in all planes
along with active and active assisted range of motion are instituted 5
to 6 weeks postoperatively. When active range of motion is 80% to 85%
of the normal side (usually 6 to 8 weeks postoperatively),
strengthening exercises are begun. Return to sports activities is
allowed at 4 to 6 months postoperatively.
majority of acute type III injuries. A sling is used for comfort for 1
to 2 weeks. Ice and rest during the first 24 to 48 hours after injury
decrease the discomfort associated with the soft tissue injury.
Patients are encouraged to remove the sling and use the shoulder
actively within their limits of pain. Patients will often avoid
overhead use of the arm for the first week to 10 days. Within 3 to 4
weeks, the range of motion is usually within 80% of the opposite
shoulder and strengthening exercises are instituted. Return to full
activity may take as long as 3 to 4 months. However, athletic activity
may be allowed
much sooner, if necessary, through the use of a protective pad over the AC joint or specifically modified athletic equipment.
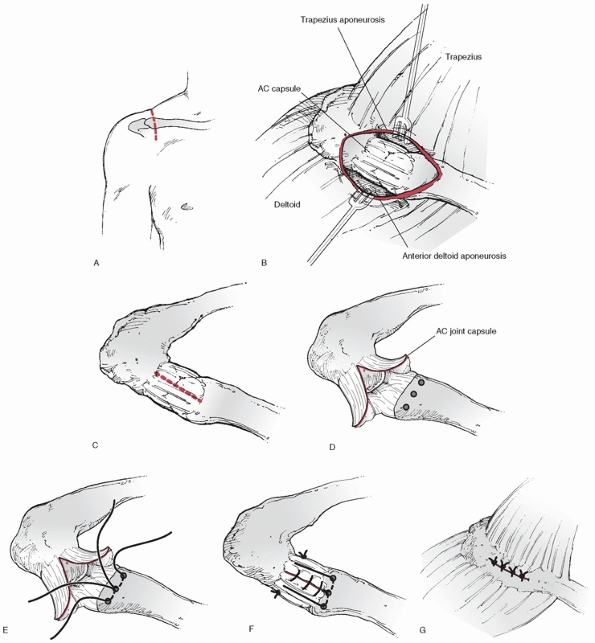 |
|
FIGURE 39-22 Surgical repair of a chronic type II AC joint injury. A. A 5- to 6-cm skin incision is made in Langer lines approximately 1.5 to 2 cm medial to the AC joint. B. The anterior deltoid aponeurosis is reflected anteriorly off of the AC joint capsule. C. The AC joint capsule is incised in a medial to lateral direction at the midportion of the joint. D.
Anterior and posterior flaps are elevated to expose the AC joint and distal clavicle. Drill holes are placed 5 mm from the articular margin and 5 mm of distal clavicle is excised using a microsagittal saw. E. Additional drill holes are placed 1 to 2 mm medial to the resectional margin; sutures are placed through the drill holes. F. The capsule is repaired back to the distal clavicle. G. The deltoid and trapezius are repaired over the capsule. |
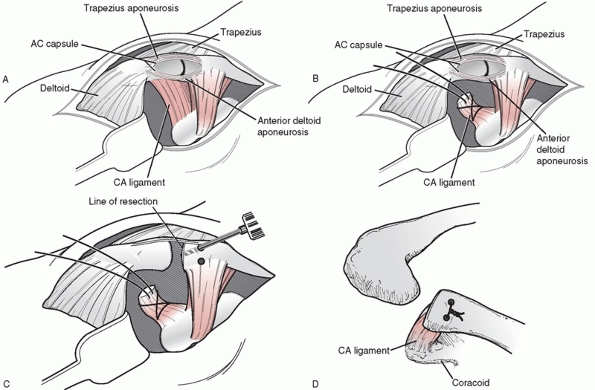 |
|
FIGURE 39-23 Transfer of the acromial attachment of the coracoacromial ligament. A. A small portion of the anterior deltoid is reflected from the anterior acromion to expose the coracoacromial ligament. B. The ligament is released from the acromion and sutures are placed in the end. C.
Two unicortical drill holes are placed in the posterosuperior surface of the distal clavicle, exiting through the medullary canal. D. The coracoacromial ligament is transferred to the medullary canal. The sutures are placed through the drill holes and tied over the top of the clavicle. |
injuries is considered in heavy manual laborers, patients with a
concomitant brachial plexus injury, or overhead athletes when the
injury involves the dominant arm. In order for surgical intervention to
occur, the patient must understand that return to full activities will
not be permitted for 4 to 6 months postoperatively. In addition, the
postoperative protocol, including the use of an abduction pillow for 3
to 6 weeks, is discussed in detail. If the patient agrees, operative
stabilization is performed. This represents 5% or less of all type III
AC injuries seen by our service.
detailed earlier in this chapter under “Common Surgical Approaches.”
Once the dissection is complete with the distal clavicle and AC joint
exposed, any remnant of the intra-articular disk is excised. The distal
clavicle is delivered into the wound and the articular surface is
inspected (Fig. 39-24). If the articular
surface is intact, the distal clavicle is not excised. This is the
exception rather than the rule, and if there is any concern, the
meniscus is removed and the distal clavicle is excised in order to
eliminate it as a potential source of chronic pain. The anterior
deltoid, which has been elevated from its clavicular origin with the
anterior subperiosteal flap, is retracted anteriorly. The clavicle is
retracted posteriorly to expose the coracoid process. If the torn
coracoclavicular ligaments can be identified, they are preserved for
later repair. The base of the coracoid process protrudes almost
perpendicularly from the scapula. After a short distance, it makes a
direct lateral turn and proceeds laterally to its termination at the
tip. The base of the coracoid process is exposed subperiosteally. Two
bone anchors are loaded with heavy nonabsorbable sutures, one through
each anchor. It is important that the nonabsorbable sutures are passed
through drill holes in the clavicle and not around the clavicle.
Passage around the clavicle has been associated with erosion, fracture,
and loss of fixation. Use of suture anchors in the base of the coracoid
to achieve coracoclavicular fixation is a recent development replacing
the passage of sutures around the undersurface of the coracoid. After
the periosteum
at
the base of the coracoid has been removed for exposure, the holes are
drilled and the anchors inserted according to the manufacturer’s
instructions. We typically use Mitek (DePuy Mitek, Inc., Raynnam, MA)
G4 anchors (Fig. 39-25).
The strength of suture anchors was compared to sutures around the base
of the coracoid for the treatment of AC joint separations in a cadaver
study by Breslow et al.16 They found
no difference in laxity between the two methods after repeated cycling.
Suture anchors offer the advantages of a decreased risk of
neurovascular injury and reduced surgical time.
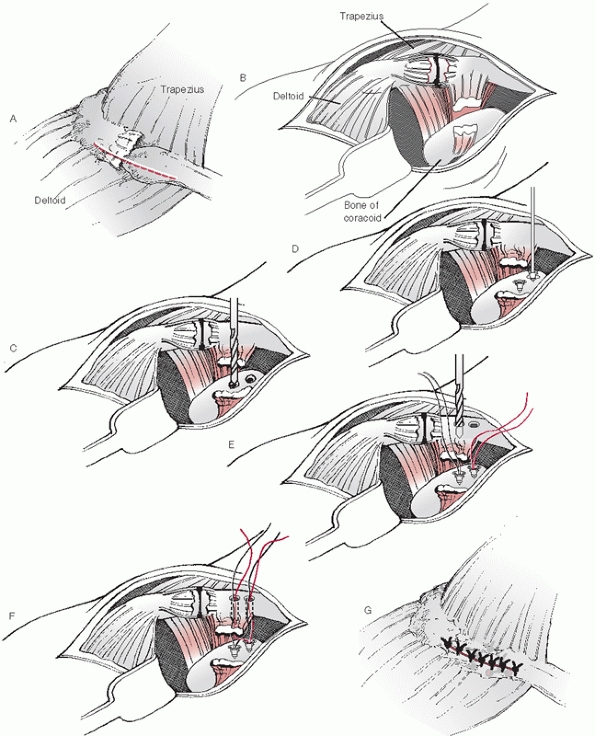 |
|
FIGURE 39-24 Operative stabilization of an acute type III AC joint injury. A. The deltotrapezius fascia is incised in a medial-lateral orientation superior to the AC joint. B. The clavicle is delivered into the wound after reflecting the anterior deltoid and trapezius. C. Two holes are drilled in the base of the coracoid in preparation for anchor insertion. D. Suture anchors are inserted in the base of the coracoid. E. Two drill holes are placed through the clavicle for passage of the sutures. F.
Two to three suture anchors are placed along the lateral clavicular margin. The sutures are used to reattach the AC joint capsule and the deltotrapezial aponeurosis. G. The deltotrapezial aponeurosis is repaired. |
the coracoid, the coracoclavicular interspace is inspected for any
remnants of the coracoclavicular ligaments. If any portions of the
ligaments can be identified and are of sufficient quality, a suture is
passed between the torn ends, but is not tied until after the clavicle
has been reduced and fixed.
The AC joint is reduced by pushing up on the elbow to bring the
acromion to the clavicle. With the joint reduced, the entry points for
the drill holes are identified. The drill holes should be bicortical
and placed at the junction of the anterior one third and posterior two
thirds of the clavicle in the anterior-posterior direction. A suture
passer is then used to pass one limb of the suture from each anchor
through each hole so that there are two sutures through each hole. Each
suture is then tied to itself over the bone bridge between the drill
holes. It is helpful to color the ends of one suture with a skin marker
before passing them through the bone; the colored suture facilitates
differentiation between the two once they are passed through the
clavicle. The AC joint is held in a reduced or slightly overreduced
position by applying an axial, compressive load to the humerus. The
coracoclavicular sutures are then tied. If any sutures were placed in
the coracoclavicular ligament remnants, they are also tied.
the tissue is imbricated over the superior aspect of the joint. Suture
anchors placed along the lateral clavicular margin in an anterior to
posterior direction approximately 5 mm from the articular surface may
facilitate reconstruction of the capsule (see Fig. 39-24).
These anchors are then used to reattach the medial (clavicular) aspect
of the AC capsule, as well as the deltoid and trapezial aponeuroses, to
the lateral aspect of the clavicle. The deltotrapezius aponeurosis and
clavicular periosteum, medial to the reattached AC capsule, are also
closed. The subcutaneous tissue and skin are then closed in a standard
fashion.
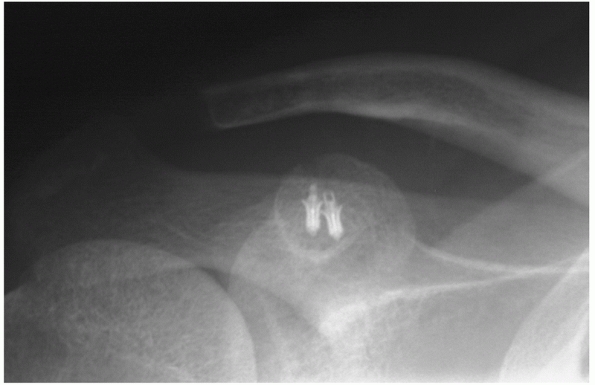 |
|
FIGURE 39-25 Postoperative radiograph after reconstruction using suture anchors at the base of the coracoid.
|
minimize stress across the repair. The shoulder is immobilized in a
sling for 6 weeks, with removal for elbow, wrist, and hand range of
motion. Overhead elevation, both active and passive, is contraindicated
for 6 weeks to avoid rotational forces across the AC joint. The
procedure is extra-articular, therefore, long-term stiffness of the
glenohumeral joint is unusual.
injuries are asymptomatic. However, when symptoms are present, they
typically take the form of trapezius fatigue, AC joint pain, and
brachial plexus irritation. Under these circumstances, AC
reconstruction is indicated.
described for reconstruction of the chronic type II injury. The
detailed incision and approach has also been described in the surgical
approach section of this chapter.
medial to the AC joint. Full-thickness flaps are developed both
medially and laterally to expose the deltotrapezial fascia. Adequate
exposure should include the AC joint as well as 2 to 3 cm of the distal
clavicle for optimal visualization. Electrocautery is used to incise
the periosteum and deltotrapezial fascia in a parallel fashion to the
longitudinal axis of the clavicle (Fig. 39-26).
The incision should start approximately 2 to 3 cm medial to the AC
joint and extend laterally to the acromial portion of the AC joint. The
lateral clavicle is exposed subperiosteally by carefully elevating the
deltotrapezial fascia, periosteum, and AC capsule in one layer starting
at the medial-lateral incision and extending anteriorly and
posteriorly. Any remnant of the intra-articular disk is excised.
excision of roughly 1 cm of the distal clavicle is performed with a
saw. The anterior deltoid, which has been elevated from its clavicular
origin, with the anterior subperiosteal flap is retracted anteriorly.
The clavicle is retracted posteriorly to
allow
exposure of the coracoid. The base of the coracoid is exposed
subperiosteally. It is important to make sure good exposure both
medially and laterally are achieved to aid in the passage around the
base of the coracoid. A Satinsky vascular clamp is placed around the
undersurface of the coracoid, in a medial to lateral fashion, staying
on bone all the way around in order to protect the neurovascular
structures below. A suture is placed into the open clamp and pulled
around the base of the coracoid (see Fig. 39-26). This suture is used to shuttle three heavy nonabsorbable sutures and a biologic graft around the base of the coracoid (see Fig. 39-26).
We often use a semitendinosus allograft, but the surgeon can use any
autograft or allograft tendon of similar strength. A whipstitch is
placed in both ends of the graft to aide in passage of the tendon.
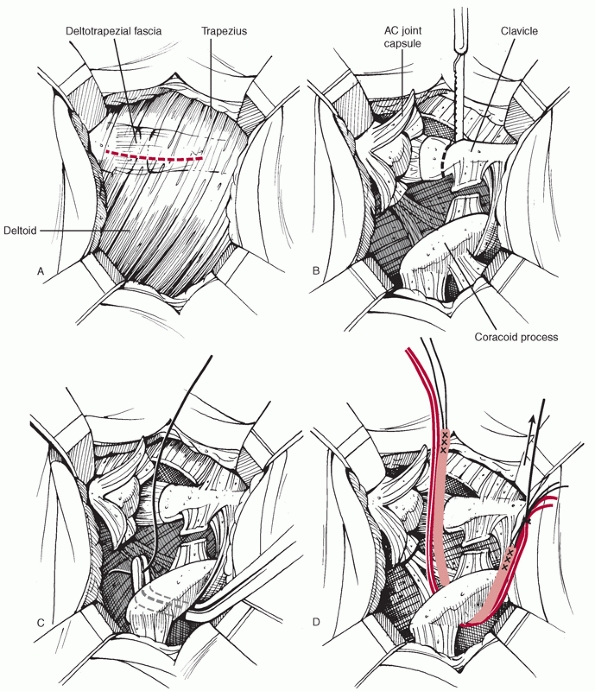 |
|
FIGURE 39-26
Treatment of a chronic type III AC joint injury with distal clavicle resection and anatomic coracoclavicular ligament reconstruction. A. The deltotrapezial fascia is incised parallel to the longitudinal axis of the clavicle. B. Excision of roughly 1 cm of the distal clavicle is performed with a saw. C. A Satinsky vascular clamp is placed around the undersurface of the coracoid and a shuttle stitch is passed. D. Nonabsorbable sutures and a biological graft are shuttled around the base of the coracoid. (continues) |
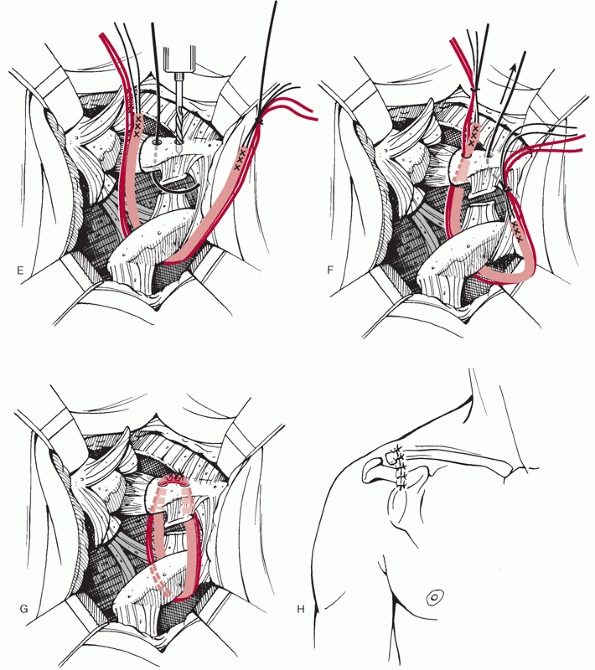 |
|
FIGURE 39-26 (continued) E. Two drill holes are placed in the clavicle with a roughly 1.5-cm bridge. F. The shuttle suture is used to bring the sutures and graft through the holes in clavicle. G. The two nonabsorbable sutures are then tied to each other to hold the clavicle reduced and then the graft is secured. H. The subcutaneous tissue and skin are repaired as described previously.
|
base of the coracoid, two drill holes are placed in the clavicle for
passage of the sutures and graft. One drill hole is placed around 1 cm
from the lateral edge of the clavicle and one is placed around 2.5 cm
from the lateral edge (see Fig. 39-26). These
holes are also drilled from slightly anterior to posterior through the
clavicle, which will help translate the clavicle slightly anteriorly
when it is secured. After the holes are drilled, sutures are placed
through the holes in the clavicle and used to shuttle the respective
suture ends up through the clavicle. The AC joint is then reduced by
pushing up on the elbow to bring the acromion to the clavicle. The two
nonabsorbable sutures are then tied to each other to hold the clavicle
securely reduced before securing the graft. The third nonabsorbable
suture is not tied and is used as a backup shuttle stitch as needed.
The graft can be secured by one of two methods. Bioabsorbable anchors
can be placed adjacent to the graft in each tunnel or the graft may be
tied over itself in a simple fashion and the knot sutured with
nonabsorbable material for security. Either method provides adequate
security of the graft while it heals to the bone tunnels. Only moderate
tension is needed when securing the graft as the heavy sutures are
supplying the main source of tension.
Closure of the incised deltotrapezial fascia is performed in a
pants-over-vest fashion using heavy nonabsorbable sutures. Any
remaining AC joint capsule should be repaired as well whenever
possible. The subcutaneous tissue and skin are repaired as described
previously.
treatment. The surgical technique and aftercare are similar to the
methods described for the acute or chronic type III injury above as
dictated by the timing of the surgery after injury. The subcoracoid
subtype of the type VI injury may require a deltopectoral incision to
extricate the dislocated clavicle. The reconstruction then proceeds as
previously described.
approach. They nearly always recover without incident, and rarely have
any further sequelae. AC injuries associated with fractures of the
coracoid process are treated nonoperatively in most cases. The
fractures usually occur at the tip or the base of the coracoid. As long
as the deltotrapezial fascia is not disrupted to a large extent, and
there is not severe coracoid displacement, we treat them in the same
manner as a type III injury (see Fig. 39-10).
intra-articularly into the glenoid, we consider surgery. This depends
largely on the amount of intra-articular displacement. We use 5 mm or
more of glenoid displacement as our criterion for surgical treatment. A
CT scan is often helpful in evaluating this fracture as the glenoid
component is much more easily appreciated with this study (see Fig. 39-13).
anatomy is essential to the safe and effective treatment of AC joint
injuries. Table 39-3 lists some tips that may
help assist the surgeon during reconstruction of the AC joint as well
as help to stay away from some of the common pitfalls associated with
this procedure.
dorsum of the acromion most often results in injury to the AC
articulation, the sternoclavicular articulation, or the shaft of the
clavicle. However, combined injuries have been reported. Wurtz and
associates158 and Lancourt80
have reported combined AC dislocation and clavicle fracture. Several
reports exist of simultaneous dislocations of both the sternoclavicular
and AC ends of the clavicle or bipolar dislocations.2,25,39,53,71,127
Bipolar clavicular dislocation (i.e., combined AC and sternoclavicular
dislocation) is a rare injury that has been sparsely reported in the
literature.2,127
When this injury does occur, it is most often a posterior or type IV AC
dislocation associated with an anterior sternoclavicular dislocation.127
This underscores the importance of a thorough evaluation of any patient
with an AC joint injury with particular attention being paid to the
sternoclavicular joint.
dislocations. Besides the obvious wound infection and osteomyelitis
that might develop from the operative procedure, several other
complications occur (e.g., a fracture through a drill hole, loss of
purchase of the internal fixation, metal failure, and migration of the
fixation device to other parts of the body). The incidence of recurrent
deformity is probably higher than routinely expected. This should not
be very surprising. There is nowhere else in the body where the weight
of an entire extremity is supported through so little fixation (Fig. 39-27).
In addition, the potential planes of motion at the injured AC joint are
numerous and result in complex loading of the reconstruction. For these
reasons, we advocate longer and more aggressive immobilization than is
commonly described.
|
TABLE 39-3 Pearls and Pitfalls
|
|
|---|---|
|
interesting history of migration into remote, life-threatening
locations such as the lung,93 the spinal cord,109 the neck84 posterior to the carotid sheath, and the pleura or close to it.38 Vessels in the thorax and neck have also been the recipients of pin migration injury (Fig. 39-28).
bending a hook on the portion of the pin that protrudes from the
acromion process. However, the pins can break, and then part of the pin
is free to migrate. Patients must be prepared and forewarned of the
possible necessity of pin removal and the complications of pins that
are not removed.
reviewed 37 reports of pin migration in operations about the shoulder.
They recommended that pin use should be avoided in operations about the
shoulder. When pins are utilized, they should be bent or have
restraining devices to decrease the risk of migration. The patient
should be informed of the risks. Close follow-up should be performed
and the pins should be removed at the conclusion of therapy or whenever
migration is noted. Pin migration may have devastating consequences.
Eight patients have died.
joint, the simple repair of the coracoclavicular and AC ligaments
without the additional support of coracoclavicular sutures, screws, or
internal fixation, the AC fixation will likely fail. This is
particularly true in chronic injury to the AC and coracoclavicular
ligaments, and there is often a major separation between the clavicle
and the coracoid. Transfer of the acromial attachment of the
coracoacromial ligament onto or into the medullary canal of the distal
clavicle alone is not strong enough. It must be supplemented with
additional fixation as recommended in the treatment section.
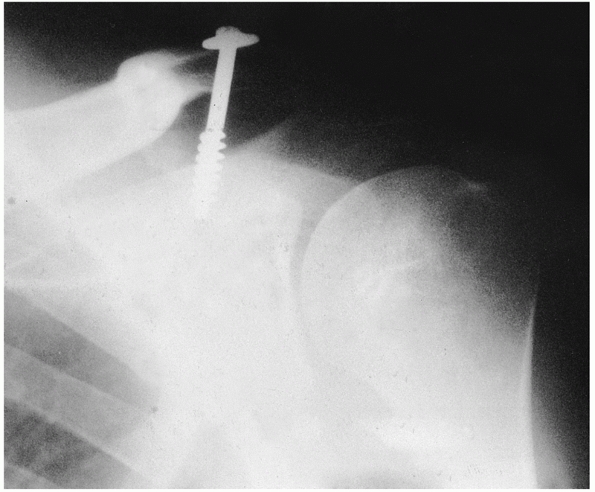 |
|
FIGURE 39-27 Radiograph showing failure of fixation of a coracoclavicular screw.
|
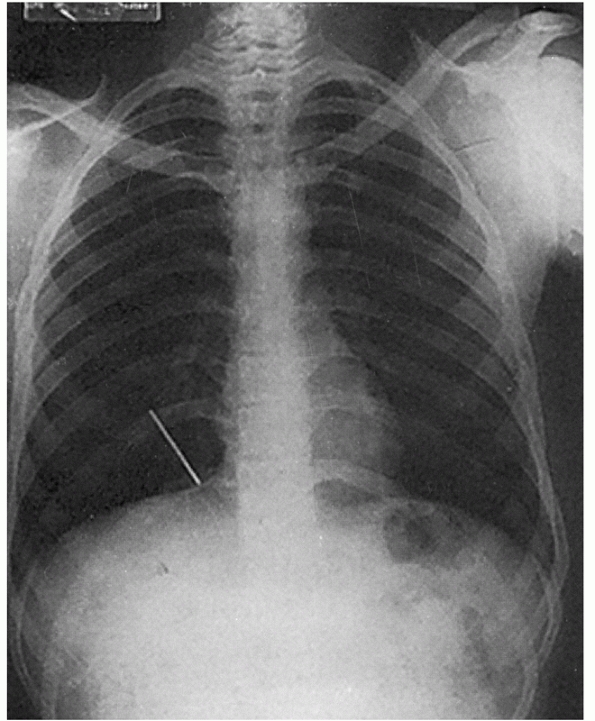 |
|
FIGURE 39-28 A broken Steinmann pin has migrated into the right lung field from its previous location in the right AC joint.
|
suture breakage, suture anchor pullout, or screw breakage. If failure
is noticed early in the postoperative period, reoperation to correct
the problem is usually indicated. If failure occurs weeks to months
after surgery, infection should be suspected and ruled out.
material has been associated with various complications. Goldberg and
colleagues55 recognized erosion of a Dacron graft through the distal clavicle in some cases (Fig. 39-29). Moneim and Balduini100
noted a coracoid fracture after reconstruction of the coracoclavicular
ligaments through two drill holes in the clavicle. Fractures of the
distal clavicle secondary to the use of loop sutures between the
coracoid and the distal clavicle have been reported.37,90 Other complications include aseptic foreign body reactions23 and infections.105 Neault et al.105
reported three cases in which nonabsorbable tape or suture was directly
related to a postoperative infection. Two infections occurred within a
year, but one was 5 years after repair of a type III injury. Colosimo
et al.23 reported two cases of
aseptic foreign body reactions to Dacron graft material 2 and 4 years
after surgery. Microscopic examination revealed chronic
inflammation
with a foreign body giant cell reaction. Both patients improved after
removal of the Dacron material and were back to work in 10 days.
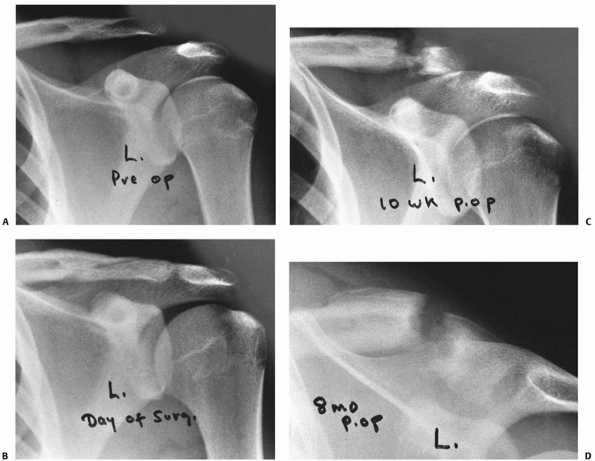 |
|
FIGURE 39-29
Complications from using cerclage material as a loop around the top of the clavicle and under the coracoid process for treatment of complete AC dislocations. A. Preoperative radiograph demonstrating the type III dislocation of the AC joint. B. The postoperative radiograph demonstrates near anatomic reduction using a 6-mm soft Dacron vascular graft loop. C. Gradual erosion of the Dacron graft completely through the distal clavicle can be seen. D. Note the superior migration of the shaft of the clavicle. |
recommended distal clavicle excision and transfer of the coracoacromial
ligament for both acute and chronic AC separations. In a review
article, Cook and Heiner24 recommend
distal clavicle excision as part of the acute surgical management of
patients with AC separations. They reported that postoperative
degenerative changes in the AC joint may be as high as 24% and that
primary excision of the distal clavicle was associated with little
morbidity. Conversely, the vast majority of series reporting the
results of surgical management of AC separations do not advocate
primary excision of the distal clavicle.66
Therefore, there is no consensus regarding primary distal clavicle
excision and coracoacromial ligament transfer for acute AC injuries.
use of arthroscopy in the treatment of AC joint injuries. Wolf and
Pennington155 described an
all-arthroscopic technique of AC joint reconstruction. The coracoid is
visualized through the subcoracoid recess in the anterior aspect of the
joint. An anterior cruciate ligament guide is used to drill a hole
through the clavicle and coracoid, and SecureStrand cable (Surgical
Dynamics, Norwalk, CT) is used for fixation. They reported a series of
4 patients with no recurrence of deformity. Lafosse et al.80
published an all-arthroscopic technique for coracoclavicular ligament
reconstruction, which releases the coracoacromial ligament from the
undersurface of the acromion and transfers it to the inferior clavicle.
Proponents of arthroscopic reconstruction claim the benefits of this
more minimally invasive technique
are less violation of deltotrapezial fascia, faster postoperative recovery, less pain, and fewer complications.
been proposed, few clinical outcome studies have been published.
Chernchujit et al.21 published a
series of 13 patients who had an arthroscopic reconstruction following
AC joint disruption using suture anchors and a titanium plate. These
patients were followed for a mean of 18 months. Twelve patients
returned to work without pain within 3 months after the operation and
the average constant score at last follow-up was 95. Postoperative
radiographs confirmed an anatomic reduction in 10 patients, residual
subluxation in two patients, and redislocation of the joint in one
patient. Given this, as well as evolving surgical techniques, we may
see an expanding role for arthroscopy in the future for the management
of these injuries.
GC, Wallace WA, Stableforth PG, et al. A classification of acute
acromioclavicular dislocation: a clinical, radiological, and anatomical
study. Injury 1992;23:194-196.
GC, Wallace WA, Stableforth PG, et al. The management of acute
acromioclavicular dislocation. A randomized prospective controlled
trial. J Bone Joint Surg 1989;71B:848-850.
JG. Direct observations on the function of the capsule of the
sternoclavicular joint in clavicular support. J Anat 1967;101:159-170.
JA, Andrish JT, Clancy WG. Evaluation of the acromioclavicular joint
following first and second-degree sprains. Am J Sports Med
1978;6:153-159.
TNJ, Brunet ME, Haddad RJ. Fractured coracoid process in
acromioclavicular dislocations: report of four cases and review of the
literature. Clin Orthop 1983;175: 227-232.
H, Hovelius L, Thorling J. Acromioclavicular separations treated
conservatively. A 5-year follow-up study. Acta Orthop Scand
1983;54:743-745.
GB, McPherson JAM, Reed MH. Traumatic pseudodislocation of the
acromioclavicular joint in children: a 15-year review. Am J Sports Med
1991;19:644-646.
PE, Iannotti JP, Williams GR. Anteroposterior instability of the distal
clavicle after distal clavicle resection. Clin Orthop 1998;348:114-120.
TC. The relation of the coracoclavicular ligament insertion to the
acromioclavicular joint. A cadaver study of relevance to lateral
clavicle resection. Acta Orthop Scand 2003;74(6):718-721.
TP, Burdette HL, Shahriari AS, et al. The role of the acromioclavicular
ligaments and the effect of distal clavicle resection. Am J Sports Med
1996;24:293-297.
MJ, Jazrawi LM, Bernstein AD, et al. Treatment of acromioclavicular
joint separation: suture or suture anchors? J Shoulder Elbow Surg
2002;11(3):225-229.
JE, Stanley RF, Tullos HS. Acromioclavicular joint dislocations:
comparative results following operative treatment with and without
primary distal clavisectomy. Am J Sports Med 1977;5:258-263.
B, Tischer T, Imhoff AB. Arthroscopic reconstruction of the
acromioclavicular joint disruption: surgical technique and preliminary
results. Arch Orthop Trauma Surg 2006;126:575-581.
EA. Rupture of the supraspinatus tendon and other lesions in or about
the subacromial bursa. In: Codman EA, ed. The Shoulder. Boston: Thomas
Todd, 1934: 32-65.
AJ, Hummer CD 3rd, Heidt RS Jr. Aseptic foreign body reaction to Dacron
graft material used for coracoclavicular ligament reconstruction after
type III acromioclavicular dislocation. Am J Sports Med 1996;24:561-563.
RS, Labriola JE, Rodosky MW. Biomechanical rationale for development of
anatomical reconstructions of coracoclavicular ligaments after complete
acromioclavicular joint dislocations. Am J Sports Med 2004;32:1929-1936.
RE, Parsons IM, Woo SL, et al. Effect of capsular injury on
acromioclavicular joint mechanics. J Bone Joint Surg Am
2001;83A:1344-1351.
JJ, Steingold RF, Richardson RA, et al. The conservative treatment of
acromioclavicular dislocation. Review after 5 years. J Bone Joint Surg
1987;69B:719-722.
C, Sautet A, Man M, et al. Acromioclavicular dislocations: treatment by
coracoacromial ligamentoplasty. J Shoulder Elbow Surg 1995;4:130-134.
WN, Lenczner EM. Stress fracture of the clavicle leading to nonunion
secondary to coracoclavicular reconstruction with Dacron. Am J Sports
Med 1989;17:128-129.
R, Serletti J. Computerized axial tomography: a method of localizing
Steinmann pin migration. Orthopedics 1981;4:1357-1360.
BS, Donati RB, Powell CE. Bipolar clavicular dislocation treated
surgically: a case report. J Bone Joint Surg 1988;70A:1251-1253.
A, Vainionpaa S, Korkala O, et al. Acute complete acromioclavicular
dislocation. A prospective randomized trial of fixation with smooth or
threaded Kirschner wires or cortical screw. Ann Chir Gynaecol
1987;76:323-326.
A, Vainionpaa S, Korkala S, et al. Four-year outcome of operative
treatment of acute acromioclavicular dislocation. J Orthop Trauma
1991;5:9-13.
EL. The biomechanics of the acromioclavicular, sternoclavicular, and
scapulothoracic joints. Instr Course Lect 1993;42:237-245.
EL, Cordasco FA, Bigliani LU. Arthroscopic resection of the outer end
of the clavicle from a superior approach: a critical, quantitative,
radiographic assessment of bone removal. Arthroscopy 1992;8:55-64.
EL, Duralde XA, Nicholson GP, et al. Arthroscopic resection of the
distal clavicle with a superior approach. J Shoulder Elbow Surg
1995;4:41-50.
K, Craig EV, An KN, et al. Biomechanical study of the ligamentous
system of the acromioclavicular joint. J Bone Joint Surg
1986;68A:434-440.
SH, Hupel TM, Beaton DE, et al. Functional outcome of acromioclavicular
joint injury in polytrauma patients. J Orthop Trauma 1998;12:159-163.
RD, Hawkins RJ, Grainger RW. A comparative analysis of operative versus
nonoperative treatment of grade III acromioclavicular separations. Clin
Orthop 1985; 193:150-155.
GM, Combs AH, Davis PF, et al. Arthroscopic acromioclavicular joint
resection. An anatomical study. Am J Sports Med 1991;19:2-5.
C, Rockwood CA. Subcoracoid dislocation of the lateral end of the
clavicle: a report of three cases. J Bone Joint Surg 1987;69A:924-927.
JA, Viglione W, Cumming WJ, et al. Review of coracoclavicular ligament
reconstruction using Dacron graft material. Aust NZ J Surg
1987;57:441-445.
PW, Petersen SA. Anatomical acromioclavicular ligament reconstruction:
a biomechanical comparison of reconstructive techniques of the
acromioclavicular joint. Am J Sports Med 2005;33:1723-1728.
FB. The treatment of complete dislocation of the outer end of the
clavicle: a hitherto undescribed operation. Ann Surg 1941;113:1094-1098.
DK, Wirth MA, Griffin JL, et al. Reconstruction of chronic and complete
dislocations of the acromioclavicular joint. Clin Orthop
1998;347:138-149.
H, Schmid L, Walch G. [Management of acromioclavicular joint
dislocation with the Wolter hook-plate. One year follow-up of 35
cases]. Unfallchirurgie 1993; 19:33-39.
H, Weinstabl R, Schmid L, et al. A crook plate for treatment of
acromioclavicular joint separation: indication, technique, and results
after 1 year. J Trauma 1993; 35:893-901.
RI, Vu DH, Sonnabend DH, et al. Anatomic variance of the
coracoclavicular ligaments. J Shoulder Elbow Surg 2001;10(6):585-588.
RI, Wallace AL, Harper GD, et al. Structural properties of the intact
and the reconstructed coracoclavicular ligament complex. Am J Sports
Med 2000;28(1): 103-108.
RJ, Warren RF, Noble JS. Suture Repair Technique for Acute and Chronic
Acromioclavicular Dislocations. Rosemont, IL: American Academy of
Orthopaedic Surgeons videotape series, 2005.
M, Gotzen L, Gehling H. Acromioclavicular reconstruction augmented with
polydioxanonsulphate bands. Surgical technique and results. Am J Sports
Med 1995; 23:552-556.
M, Gotzen L, Gehling H, et al. [Results of reconstruction of
acromioclavicular joint rupture with PDS implants]. Unfallchirurg
1997;100:193-197.
W-P, Chen J-Y, Shih C-H. The surgical treatment of complete
acromioclavicular joint dislocation. Orthop Rev 1988;27:1116-1119.
H, Claes L, Burri C, et al. The stabilizing effect of various implants
on the torn acromioclavicular joint. A biomechanical study. Arch Orthop
Trauma Surg 1986;106: 42-46.
JJ, Williams GR, Sher JS, et al. The acromioclavicular capsule as a
restraint to posterior translation of the clavicle: a biomechanical
analysis. J Shoulder Elbow Surg 1999;8:119-124.
S, Sethi A, Jain AK. Surgical treatment of complete acromioclavicular
dislocation using the coracoacromial ligament and coracoclavicular
fixation: report of a technique in 14 patients. J Orthop Trauma
1995;9:507-510.
HP, Kotz RI. Bone-ligament transfer of coracoacromial ligament for
acromioclavicular dislocation. A new fixation method used in six cases.
Acta Orthop Scand 1997;68:246-248.
L, Baier GP, Leuzinger J. Arthroscopic treatment of acute and chronic
acromioclavicular joint dislocation. Arthroscopy 2005;21:1017-1028.
JB. Acromioclavicular dislocation with adjacent clavicular fracture in
a horseback rider: a case report. Am J Sports Med 1990;18:321-322.
E, Bjerg-Nielsen A, Christensen P. Conservative or surgical treatment
of acromioclavicular dislocation. A prospective, controlled, randomized
study. J Bone Joint Surg 1986;68A:552-555.
KW, Debski RE, Chen CH, et al. Functional evaluation of the ligaments
at the acromioclavicular joint during anteroposterior and
superoinferior translation. Am J Sports Med 1997;25:858-862.
RW, Gutowski WT. Migration of a broken pin following fixation of the
acromioclavicular joint. Orthopedics 1986;9:413-416.
A, Marco L, Cebrian R. Acute dislocation of the acromioclavicular
joint. Traumatic anatomy and the importance of deltoid and trapezius. J
Bone Joint Surg 1994; 76B:602-606.
PB, Alexander MJ, Frejuk J, et al. Comprehensive functional analysis of
shoulders following complete acromioclavicular separation. Am J Sports
Med 1988; 16:475-480.
C, Grassi G, Oretti D. Posterior dislocation of the acromioclavicular
joint: a rare or an easily overlooked lesion? Ital J Orthop Traumatol
1978;4:79-83.
T, Rodriguez-Merchan C, Munuera-Martinez L. Fracture of the coracoid
process: presentation of seven cases and review of the literature. J
Trauma 1993;30: 1597-1599.
LS, Simonson BG, Wolock BS. Osteolysis of the distal clavicle in a
female body builder: a case report. Am J Sports Med 1992;21:50-52.
RJ. Migration of a Kirschner wire from the shoulder region into the
lung: a report of two cases. J Bone Joint Surg 1943;25A:477-483.
AD, Santangelo SA, Johnson ST. A biomechanical evaluation of an
anatomical coracoclavicular ligament reconstruction. Am J Sports Med
2006;34:236-246.
EG, Blivin SJ, Doehring CB, et al. Treatment of grade III
acromioclavicular separations in professional throwing athletes:
results of a survey. Am J Orthop 1997; 26:771-774.
RJ, Zuckerman JD, Nainzadeh N. Type III acromioclavicular joint
separation associated with late brachial plexus neurapraxia. J Orthop
Trauma 1992;6:370-372.
EC. Osteolysis of the distal clavicle in a woman: case report and a
review of the literature. Ital J Orthop 1992;18:561-563.
MS, Balduini FC. Coracoid fracture as a complication of surgical
treatment by coracoclavicular tape fixation. A case report. Clin Orthop
1982;168:133-135.
DS, Lemos MJ. Acromioclavicular separation. Reconstruction using
synthetic loop augmentation. Am J Sports Med 1995;23:105-110.
E, Garofalo R, Crevoisier X, et al. Grade I and II acromioclavicular
dislocations: results of conservative treatment. J Shoulder Elbow Surg
2003;12(6):599-602.
MA, Nuber GW, Marymont JV. Infections after surgical repair of
acromioclavicular separations with nonabsorbable tape or suture. J
Shoulder Elbow Surg 1996;5: 477-478.
JS. Acromioclavicular dislocation treated by transference of the
coracoacromial ligament: a long-term follow-up in a series of 112
cases. Clin Orthop 1968;58:57-68.
CW, Chatterjee A. Type III acromioclavicular separation: results of a
recent survey on its management. Am J Orthop 2007;36;89-93.
H, Llewellyn RC. Migration of a threaded Steinmann pin from an
acromioclavicular joint into the spinal canal. J Bone Joint Surg
1965;47A:1024-1026.
GW, Bowen MK. Disorders of the acromioclavicular joint:
pathophysiology, diagnosis, and management. In: Iannotti JP, Williams
GR, eds. Disorders of the Shoulder: Diagnosis and Management.
Philadelphia: Lippincott Williams & Wilkins, 1999: 739-764.
GW, Bowen MK. Disorders of the acromioclavicular joint:
pathophysiology, diagnosis, and management. In: Iannotti JP, Williams
GR, eds. Disorders of the Shoulder: Diagnosis and Management.
Philadelphia: Lippincott Williams & Wilkins, 1999: 739-762.
S, Virtanen K, Holopainen YVO. Posttraumatic osteolysis of the distal
ends of the clavicle: a report of three cases. Ann Chir Gynaecol
1984;73:83-86.
P, Bjorkenheim JM, Paukku P, et al. Surgical treatment of
acromioclavicular dislocation: a review of 39 patients. Injury
1983;14:415-420.
J, Zuckerman JD, Gallagher M, et al. Treatment of grade III
acromioclavicular separations. Operative versus nonoperative
management. Bull Hosp Jt Dis 1997;56: 77-83.
ML, Dias JJ. Long-term results of conservative treatment for
acromioclavicular dislocation. J Bone Joint Surg 1996;78B:410-412.
CA. Injuries to the acromioclavicular Joint. In: Rockwood CA, Green DP,
eds. Fractures in Adults. Vol 1. 2nd ed. Philadelphia: JB Lippincott,
1984:860.
CA, Williams GR, Young CD. Injuries to the acromioclavicular joint. In:
Rockwood CA, Green DP, Bucholz RW, Heckman JD, eds. Fractures in
Adults. Vol 2. 4th ed. Philadelphia: Lippincott-Raven, 1996:1341-1414.
EG, Nasca RJ, Shelley BS. Anatomical observations on the
acromioclavicular joint and supporting ligaments. Am J Sports Med
1987;15:199-206.
TF, Burks RT, Marcus RL, et al. A prospective evaluation of untreated
acute grade III acromioclavicular separations. Am J Sports Med
2001;29(6):699-703.
A, Schmid F. [Use of arthrosonography in diagnosis of Tossy III lesions
of acromioclavicular joints]. Aktuel Traumatol 1988;18:957-962.
H, Roth C, Chuinard R. Bone block transfer of coracoacromial ligament
in acromioclavicular injury. Clin Orthop 1986;208:272-277.
E, Schwarz N, Hocker K, et al. Repair of complete acromioclavicular
separations using the acromioclavicular-hook plate. Clin Orthop
1995;314:134-142.
S, Lundblad R, Dullerud R. Coracoid process transfer for
acromioclavicular dislocation. Acta Orthop Scand 1988;59:180-182.
JT, Perry JFJ. Brachial plexus injuries from blunt trauma—a harbinger
of vascular and thoracic injuries. Ann Emerg Med 1987;16:404-406.
N, Patel DV, Porter DS. Stabilization of acute acromioclavicular
dislocation by a modified Bosworth technique: a long-term follow-up
study [published erratum appears in Injury 1992;23(5):359]. Injury
1992;23:189-193.
TN, Wilson FC, Oglesby JW. Dislocation of the acromioclavicular joint.
An endresult study. J Bone Joint Surg 1987;69A:1045-1051.
TW, Green JR 3rd, Mukherjee DP, et al. Bioabsorbable screw fixation in
coracoclavicular ligament reconstruction. J Long Term Eff Med Implants
2003;13(4): 317-323.
J, Sellers R, Tonino P. Strength testing after third-degree
acromioclavicular dislocations. Am J Sports Med 1992;20:328-331.
TG, Oyen JF, Eggen PJ. A modified technique of reconstruction for
complete acromioclavicular dislocation. Am J Sports Med 2003;31:655-659.
JD, Mead NC, Sigmond HM. Acromioclavicular separations: useful and
practical classification for treatment. Clin Orthop 1963;28:111-119.
PM. Percutaneous cannulated screw coracoclavicular fixation for acute
acromioclavicular dislocations. Clin Orthop 1989;243:112-121.
MR. Complete dislocation of the acromioclavicular joint: the nature of
the traumatic lesion and effective methods of treatment with an
analysis of 41 cases. J Bone Joint Surg 1946;28:813-837.
E, Casteleyn PP, De Boeck H, et al. Surgical treatment of acute type V
acromioclavicular injuries. A prospective study. Acta Orthop Belg
1992;58:176-182.
E, DeBoeck H, Haentjens P, et al. Surgical treatment of acute type-V
acromioclavicular injuries in athletes. Arch Orthop Trauma Surg
1993;112:189-192.
K, Hsu K, Shih C. Coracoid process fracture combined with
acromioclavicular dislocation and coracoclavicular ligament rupture: a
case report and review of the literature. Clin Orthop 1994;300:120-122.
CD, Ward MW. Operation for acromioclavicular dislocation. A review of
29 cases treated by one method. J Bone Joint Surg 1987;69B:715-718.
JK, Dunn HK. Treatment of acromioclavicular injuries, especially
complete acromioclavicular separation. J Bone Joint Surg
1972;54A:1187-1194.
DM, McCann PD, McIlveen SJ, et al. Surgical treatment of complete
acromioclavicular dislocations. Am J Sports Med 1995;23:324-331.
GR, Nguyen VD, Rockwood CR. Classification and radiographic analysis of
acromioclavicular dislocations. Appl Radiol 1989;12:29-34.
LD, Lyons FA, Rockwood CA Jr. Fracture of the middle third of the
clavicle and dislocation of the acromioclavicular joint. A report of
four cases. J Bone Joint Surg 1992;74A:133-137.
LO, Lyons FA, Rockwood CA. Fracture of the middle third of the clavicle
and dislocation of the acromioclavicular joint. J Bone Joint Surg
1992;74A:133-136.
