Heel Pain (Plantar Fasciitis)
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Heel Pain (Plantar Fasciitis)
Heel Pain (Plantar Fasciitis)
Dhruv B. Pateder MD
Description
-
Plantar fasciitis is the most common cause of plantar heel pain.
-
Other causes include:
-
Compression of the 1st branch of the LPN
-
Fat pad atrophy of the heel
-
Pain and enthesopathy associated with seronegative spondyloarthropathies
-
Tarsal tunnel syndrome
-
Calcaneal stress fracture
-
Geriatric Considerations
Plantar heel pain in geriatric patients often is
secondary to atrophy of the heel pad or degenerative changes of the
plantar fascia origin.
secondary to atrophy of the heel pad or degenerative changes of the
plantar fascia origin.
Pediatric Considerations
-
Heel pain in pediatric patients usually
is secondary to apophysitis of the calcaneus (Sever disease), a
self-limited condition related to tension of the insertion area of the
Achilles tendon. -
It usually responds to rest, NSAIDs, restriction from running or sports, and short-term immobilization with a cast.
-
It virtually always resolves once skeletal maturity is achieved, resulting in fusion of the calcaneal apophysis.
Pregnancy Considerations
-
Heel pain often is secondary to plantar
fasciitis or enthesopathy from hormonal changes or mechanical stress
secondary to weight gain during pregnancy. -
It also can occur from nerve compression of the tarsal tunnel or 1st branch of the LPN because of increased fluid retention.
-
It often improves once pregnancy ends.
General Prevention
The condition is not always preventable, but it may be
limited by avoiding excessive weight gain, prolonged standing, and
sudden increases in running or jumping stresses.
limited by avoiding excessive weight gain, prolonged standing, and
sudden increases in running or jumping stresses.
Epidemiology
Incidence
-
Extremely common in adults
-
Most common in the 3rd to 5th decades
Risk Factors
-
Decreased ankle dorsiflexion/tight heel cord
-
Obesity/body mass index >30
-
Prolonged standing
-
Running
-
Jumping sports
-
Lupus or inflammatory spondyloarthropathy
-
Diabetes
-
Thyroid dysfunction
Etiology
-
The term “fasciitis” represents a
misnomer; fasciitis is a degenerative condition without histologic
evidence of chronic inflammation (Fig. 1). -
May have repetitive contracture and adhesions of the plantar fascia, with painful microscopic tearing with daily activity
Associated Conditions
-
Flatfoot
-
Achilles contracture or tight heel cord
-
Inflammatory arthropathies
-
Obesity
-
Cavus foot that results in contracture of plantar fascia and plantar soft tissues
Signs and Symptoms
History
-
Plantar fasciitis commonly is diagnosed with the history and physical examination.
-
Patients commonly complain of heel pain that is worse in the morning with the “1st step” or after prolonged sitting.
-
Symptoms may ease as the person walks and “loosens up.”
-
Symptoms may worsen as the day progresses.
-
Pain is described as sore, aching, burning, or stabbing.
Physical Exam
-
Assess alignment for planus or cavus foot deformity.
-
Assess ankle dorsiflexion with the knee flexed and extended to rule out contracture of Achilles tendon or gastrocnemius.
-
Palpate to localize tenderness to the plantar-medial heel at the origin of the plantar fascia.
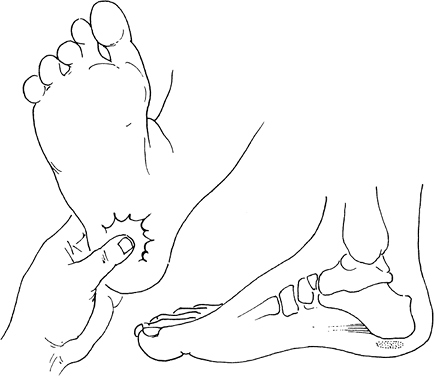 Fig.
Fig.
1. In a patient with plantar fasciitis, the area of tenderness is in
the insertion of the plantar fascia into the calcaneus. -
Tenderness may worsen with the toes passively dorsiflexed by the examiner, a maneuver that stretches the plantar fascia.
-
Palpate and percuss (Tinel sign) over the
tarsal tunnel and 1st branch of the LPN deep to the abductor hallucis
muscle to identify nerve compression. -
Pain central and directly plantar under
the calcaneal tuberosity, along with thinning of the heel pad, may
indicate fat pad atrophy. -
Medial-lateral compression may be suggestive of calcaneal stress fracture.
Tests
Lab
-
Chronic cases may necessitate lab tests,
including rheumatoid factor, antinuclear antibody screen, thyroid
function, blood glucose and hemoglobin A1C levels. -
HLA-B27 determination may be obtained if spondyloarthropathy is suspected.
Imaging
-
Radiography:
-
Standing radiographs of the foot should be obtained for patients with persistent pain.
-
The presence of a heel spur at the
calcaneal tuberosity is not diagnostic; the spur is located within the
flexor hallucis brevis muscle rather than the plantar fascia. -
In addition, the literature reports a high incidence of spur in asymptomatic patients.
-
-
Bone scans may show increased uptake at
the origin of the plantar fascia; more diffuse uptake may indicate
calcaneal stress fracture. -
MRI:
-
May show thickening and degenerative changes of the plantar fascia origin, along with bony edema adjacent to it.
-
In calcaneal stress fracture, MRI shows more extensive bony edema.
-
P.169
Pathological Findings
-
Chronic degeneration is noted at the plantar fascia origin.
-
Usually no evidence of inflammation is present.
Differential Diagnosis
-
Calcaneal apophysitis (Sever disease) in children
-
Calcaneal stress fracture
-
Central heel pad atrophy
-
Tarsal tunnel syndrome or entrapment of the 1st branch of LPN
-
Inflammatory enthesopathy
-
Spinal radiculopathy
General Measures
-
Nonoperative treatment is the cornerstone for this problem, and surgery rarely is indicated.
-
Stretching exercises of the heel cord should be performed multiple times daily and before and after sports.
-
NSAIDs
-
Off-the-shelf gel heel pad or wedge may improve cushioning of the heel.
-
A dorsiflexion night splint has been shown to alleviate symptoms in chronic cases (1).
-
An orthotic arch support may be indicated if the patient has pes planus.
-
Deep tissue massage and ice application may help symptoms.
-
Immobilization in a walking cast or fracture boot may rest the plantar fascia.
-
Injections into the plantar fascia origin can be administered if the pain does not respond to other measures.
-
The patient should be immobilized for 1–2 weeks in a boot or cast to prevent rupture after injection.
-
-
After successful treatment, the patient
may be allowed to resume activities gradually, taking care not to
resume running or jumping sports too quickly or too strenuously. -
Extracorporeal shock-wave treatment shows promise in the treatment of recalcitrant plantar fasciitis
-
Success rates of ~80%, with low complications (2)
-
May prove to be an alternative or last resort before surgical treatment (2)
-
-
A calcaneal stress fracture or
apophysitis (Sever disease) usually responds to rest, restriction from
sports, NSAIDs, and short-term immobilization for severe symptoms. -
Heel pad atrophy is treated with a comfortable shoe with absorptive heel cushioning or off-the-shelf gel cushion.
Special Therapy
Physical Therapy
Physical therapy may be helpful in teaching patients to stretch and in supervising their return to physical activity.
Medication
NSAIDs are useful for patients with severe pain.
Surgery
-
Indicated only after nonoperative methods have failed for at least 6–9 months
-
Consists of partial release of plantar fascia origin
-
Some authors recommend removal of a bone spur, although most believe doing so is not necessary in most cases.
-
-
For resistant tarsal tunnel syndrome or
entrapment of the 1st branch of the LPN, decompression of the nerve is
indicated at the time of partial plantar fascia release (3). -
Contraindicated in patients with Sever disease.
Prognosis
>90% of cases respond to nonoperative treatments, with generally good prognosis for return to activities (4).
Complications
Rupture of the plantar fascia after a steroid injection
or excessive (total) surgical release can result in arch collapse and
painful mechanical overload of the lateral midfoot (5).
or excessive (total) surgical release can result in arch collapse and
painful mechanical overload of the lateral midfoot (5).
References
1. Wapner KL, Sharkey PF. The use of night splints for treatment of recalcitrant plantar fasciitis. Foot Ankle 1991;12:135–137.
2. Ogden JA, Alvarez RG, Marlow M. Shockwave therapy for chronic proximal plantar fasciitis: a meta-analysis. Foot Ankle Int 2002;23:301–308.
3. Baxter DE, Pfeffer GB. Treatment of chronic heel pain by surgical release of the first branch of the lateral plantar nerve. Clin Orthop Relat Res 1992;279:229–236.
4. Gill LH. Plantar fasciitis: diagnosis and conservative management. J Am Acad Orthop Surg 1997;5:109–117.
5. Acevedo JI, Beskin JL. Complications of plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int 1998;19:91–97.
Additional Reading
Pfeffer GB. Plantar heel pain. In: Myerson MS, ed. Foot and Ankle Disorders. Philadelphia: WB Saunders, 2000:834–850.
Riddle DL, Pulisic M, Pidcoe P, et al. Risk factors for plantar fasciitis: a matched case-control study. J Bone Joint Surg 2003;85A:872–877.
Codes
ICD9-CM
-
355.5 Tarsal tunnel syndrome
-
355.8 First branch lateral plantar nerve entrapment
-
726.73 Heel pain
-
728.71 Plantar fasciitis
-
732.5 Sever’s disease/apophysitis
-
733.95 Calcaneal stress fracture
Patient Teaching
-
Instruct the patient about the anatomy of the plantar fascia and its role in stabilizing the foot.
-
Review the pathophysiology and degenerative nature of this condition, with its tendency for recurrent episodes.
-
Remind the patient about the importance of stretching and of moderation during a return to sports.
-
Reassure patients that, in most cases, this condition is self-limited.
FAQ
Q: What is the most common cause of heel pain in children?
A:
Sever disease, or apophysitis of the calcaneus at the insertion of the
Achilles tendon. This self-limited condition resolves once the
apophysis fuses to the remainder of the calcaneus at skeletal maturity.
Sever disease, or apophysitis of the calcaneus at the insertion of the
Achilles tendon. This self-limited condition resolves once the
apophysis fuses to the remainder of the calcaneus at skeletal maturity.
Q: What is the pathophysiology of plantar fasciitis?
A:
This condition is degenerative rather than inflammatory. Microscopic
tears and adhesions of the plantar fascia result in pain with
weightbearing activity.
This condition is degenerative rather than inflammatory. Microscopic
tears and adhesions of the plantar fascia result in pain with
weightbearing activity.
Q: When is surgery indicated for plantar fasciitis?
A: Only after a trial of nonsurgical methods for 6–9 months has failed.
