LESSER TOE DISORDERS
proximal, middle, and distal phalanx. In the case of the fifth toe,
sometimes the middle and distal phalanx fail to separate (7).
Barriers to deformities include the medial and lateral collateral
ligaments of the metatarsophalangeal (MP) joints, as well as of the
proximal and distal interphalangeal joints. The plantar plate helps to
passively return the MP joints to a neutral position when the joints
are dorsiflexed during ambulation.
Dorsiflexion of the MP joint is accomplished by the extensor digitorum
longus tendon, whereas flexion of that joint is accomplished by the
intrinsic lumbrical and interossei musculature. The interossei attach
to the dorsal hood over the proximal phalanx, and through this they
work to act as extensors of the proximal and distal interphalangeal
joints. The proximal interphalangeal (PIP) joint is plantar flexed by
the flexor digitorum brevis, and the distal interphalangeal joint is
plantar flexed by the flexor digitorum longus (FDL) tendon. Because the
strength of the extrinsics is significantly greater than that of the
intrinsics, deformities are most commonly that of dorsiflexion at the
MP joint and plantar flexion at the proximal and distal interphalangeal
joints.
is often a tight FDL tendon; if the deformity persists for a sufficient
duration, it can become fixed. A disproportionately long lesser toe or
a shoe with a tight toe box can also cause a fixed hammer-toe
deformity. Further causes of hammer-toe deformity can be poor shoe wear
or the formation of a hallux
valgus deformity, which can push the second toe into a “hammered” or overlapped position.
or at the tip of the toe where the toe hits the sole of the shoe. If
the hammer toe produces sufficient distal migration of the plantar
fatty cushion, pain under the metatarsal head can result. Shoe
modifications, including extradepth shoes, soft insoles, and metatarsal
pads, can help to alleviate symptoms.
 |
|
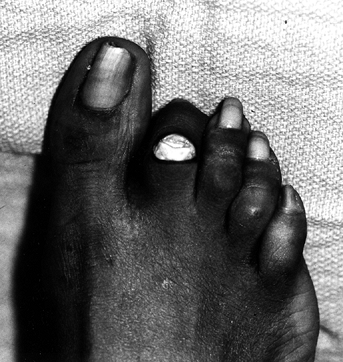
Figure 113.1. A patient with a symptomatic second hammer toe. A: Oblique view. B: Top view.
|
such as a tight FDL tendon or a hallux valgus deformity, is important
prior to any surgical treatment. A hallux valgus deformity can reduce
the space lateral to the hallux, which prevents reduction of a second
toe into a reduced position. If this condition exists, a hallux valgus
repair should be strongly considered as a concomitant surgical
procedure.
consists of the resection of the distal condyle of the proximal
phalanx. It results in a fibrous ankylosis that allows approximately 15
° or 20° of motion. An alternative is bony arthrodesis of the PIP joint.
-
Make a dorsal elliptical incision over the PIP joint. Sharply remove the skin, extensor tendon, and capsule (Fig. 113.2).
![]() Figure 113.2. Removal of an ellipse of skin above the proximal interphalangeal joint.
Figure 113.2. Removal of an ellipse of skin above the proximal interphalangeal joint. -
Release the medial and lateral collateral
ligaments, and, after exposing the distal condyle of the proximal
phalanx, remove the condyle using a bone cutter (Fig. 113.3). Take care to remove the entire condyle and make the cut so that it is perpendicular to the shaft of the proximal phalanx. Figure 113.3.
Figure 113.3.
The soft tissues have been elevated off the distal condyle of the
proximal phalanx, and a bone cutter is about to remove the distal
condyle. Note that the blades are perpendicular to the shaft of the
phalanx. -
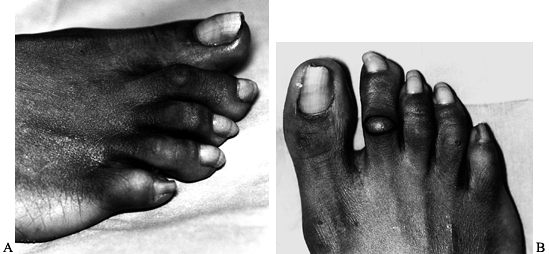
Then stabilize the toe with a 0.045-inch,
double-ended Kirschner (K-) wire brought out distally from the PIP
joint and then advanced in a retrograde fashion across the joint into
the shaft of the proximal phalanx (Fig. 113.4). If stabilization of the MP joint is also desired, use a 0.062-inch K-wire to decrease the chance of breakage of the K-wire.![]() Figure 113.4.
Figure 113.4.
A K-wire has been placed from the PIP joint out through the tip of the
distal toe, and it will be brought into the proximal phalanx in a
retrograde fashion. -
Close the skin with vertical mattress sutures (Fig. 113.5).
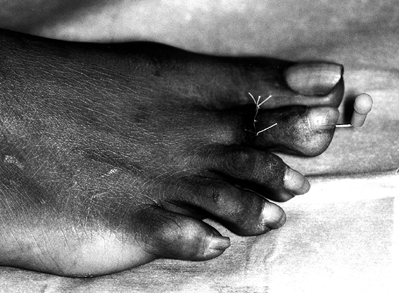 Figure 113.5.
Figure 113.5.
The K-wire has been advanced to the proximal phalanx, bent, and cut.
The extensor mechanism of the toe has been repaired as well as the skin.
Allow the patient to ambulate with full weight bearing in a
postoperative shoe 3 weeks after surgery. Splint the toe into neutral
with tape for 3 weeks after removal of the pin. Advise the patient to
use an open-toed shoe or one with a roomy toe box.
hammer-toe surgery. This usually decreases over the course of 6 months.
Recurrence of a hammer-toe deformity
is
sometimes noted, and a floppy toe can result if too much of the shaft
of the proximal phalanx is removed along with the distal condyle.
Migration of the intermedullary pin can occur if the end is not bent or
if a fixation device is not attached to the distal aspect of the pin.
completely eliminated with plantar flexion of the MP joint or of the
ankle. These deformities are usually caused by tightness of the FDL
tendon. Treat a flexible hammer toe with a Girdlestone-Taylor (11)
flexor tendon transfer if surgery is indicated. This transfer, often
combined with the release of deforming forces at the MP joint, can
produce satisfactory results. An arthroplasty of the PIP joint is
sometimes combined with the tendon transfer if there is some element of
a fixed component.
-
Make a transverse incision under the
proximal aspect of the proximal phalanx and carry dissection bluntly
down to the flexor tendon sheath. Then open the flexor tendon sheath
with a longitudinal incision using a #11 blade. -
Identify the FDL tendon and apply gentle traction by placing a curved hemostat beneath the tendon.
-
Then make a second plantar transverse
incision at the level of the distal plantar flexion crease at the
distal interphalangeal joint. -
Free up the FDL tendon distally, transect
it near its insertion, and bring it out through the proximal plantar
transverse incision. Then split the tendon along its raphe. -
Make a longitudinal incision dorsally
over the dorsal MP joint extending out to the distal condyle of the
proximal phalanx, and release the extensor tendon and collateral
ligaments if necessary. -
Excise the distal condyle of the proximal phalanx as in a fixed hammer-toe repair if there is noncorrectable deformity.
-
Bring up each half of the FDL tendon from
plantar to dorsal along both sides of the shaft of the proximal
phalanx, and suture it into the extensor hood. Do this with the PIP
joint of the toe extended and with the MP joint in slight flexion. -
Close all wounds and hold the toe in
neutral position with a postoperative dressing. Fix the toe with a
0.062-inch K-wire if a fixed PIP joint deformity was treated.
pressure or swelling around the area of the tendon transfer, producing
vascular or neurologic compromise. Other difficulties, such as swelling
and recurrence of deformity,
can also occur. Minimize these risks with gentle precise surgical technique.
These usually consist of a fixed dorsiflexion deformity, although
subluxation or dislocation of the joint can occur. Mild dorsiflexion
deformities often can be treated with extensor tenotomy. Should the
deformity be of such a magnitude that this treatment is not sufficient,
however, an open release of the joint capsule may be necessary. An open
extensor tenotomy and capsulotomy will correct many subluxation
deformities, although it is important to ensure release of the medial
and lateral collateral ligaments also. Take care to avoid injury to the
neurovascular bundles on either side of the joint. After correcting the
soft-tissue deforming forces, hold the toe in a neutral position and
insert an intermedullary K-wire of at least 0.062 inches in diameter.
Protect the foot with a wooden postoperative shoe until the pin is
removed, 2–3 weeks after surgery.
procedure is often not adequate, and an arthroplasty of the MP joint is
necessary. Decompression of the joint will allow its reduction, and the
conversion of a diarthrodial joint to a fibrous joint will provide
stability.
-
Make a dorsal longitudinal incision over
the MP joint and perform a dorsal capsulotomy with release of the
collateral ligaments. Do a dorsal extensor tenotomy if necessary. -
Plantar flex the toe, and resect
approximately 2–4 mm of bone off the distal metatarsal head. Use a
rongeur, power saw, or osteotome to bevel the plantar and dorsal
surfaces of the distal metatarsal head. -
Allow the toe to return to a neutral
position, and repetitively move the ankle dorsally and plantarly to
check the stability of the MP joint. The amount of bone that requires
resection can be estimated by evaluating the overlap seen
preoperatively on a lateral radiograph of the MP joint. -
After obtaining satisfactory stability,
stabilize the joint with a K-wire of at least 0.062 inches. Position
the wire by inserting it into the proximal phalanx and drilling it out
the tip of the toe. Then align the joint and insert the wire across the
joint into the metatarsal head in a retrograde fashion. Bend the pin to
prevent its proximal migration, and cut it. Hold the toe in a slightly
plantar-flexed position during pin fixation.
wooden postoperative shoe. Remove the pin prior to return to regular
shoes, after 3 weeks or so. There will be a loss of up to 50% of normal
motion. This arthrofibrosis, however, helps to provide stability and
prevent dislocation.
complication of this procedure. Thorough release of the soft tissues is
the best method of preventing redislocation. Neurologic or vascular
compromise can occur if the toe stays reduced without adequate
soft-tissue release, or if the vascular supply is compromised prior to
the procedure. Occasionally, removal of the K-wire may be necessary to
improve postoperative vascular status. Redislocation often occurs after
K-wire removal; however, this is preferable to necrosis of all or part
of the toe.
on the second toe and lead to dorsal subluxation or dislocation of the
second toe, placing the great toe adjacent to the third toe (1,2,3 and 4).
This results in attenuation of the second MP joint’s fibular collateral
ligament, and possibly even the formation of a rent in it. The tibial
collateral ligament can sometimes contract. As the deformity
progresses, dorsal subluxation and possibly dislocation of the second
MP joint can occur.
Grasp the proximal phalanx of the lesser toe between the thumb and
index finger and stabilize the metatarsal with the other hand. Then
manipulate the toe in a vertical fashion. If instability exists, there
is subluxation at the MP joint, and pain may exist.
-
Make a dorsal longitudinal incision over the second MP joint.
-
Perform extensor tenotomy as well as dorsal capsulotomy and collateral ligament release as described in the previous paragraphs.
-
Hold the toe in a reduced position with a 0.062-inch intramedullary K-wire for 4–6 weeks after surgery.
-
For severe deformity, MP joint arthroplasty, as previously
P.3030
described, may be necessary to both decompress the joint and allow reduction of the proximal phalanx. A Girdlestone-Taylor (11)
flexor tendon transfer may also be necessary. Reefing of the lateral
capsule may also be used to strengthen the reconstruction and decrease
the chances of recurrence of the deformity. -
Perform correction of the hallux valgus
deformity at the same time as repair of the second toe to allow for
proper placement and reduction of the toe, and to prevent the hallux
from again displacing the second toe (see Chapter 112).
swelling of the toe as well as recurrence of the first and second toe
deformity. Loss of motion at the MP joint from postsurgical scarring
and fibrous arthrodesis is a common complication. Occasional
neurovascular compromise from stretching of the neurovascular bundle
with reduction of the toe at the MP joint is also a possibility. Avoid
this by adequate soft-tissue release, avoiding overlengthening, and
gentle surgical technique.
together with a flexion deformity of either the proximal or distal
interphalangeal joints. The PIP joint is involved much more frequently
than the distal interphalangeal joint in a claw-toe deformity. When
evaluating a claw toe, examine both the MP and the involved
interphalangeal joint to determine whether the involved deformity is
fixed or flexible at each joint. In addition, carefully evaluate the
hallux for a valgus deformity, which could prevent reduction of the
second toe into its normal position. If there is a hallux valgus
deformity that might interfere with the second toe, correct it
simultaneously.
-
At the PIP joint, make a dorsal
elliptical incision and perform a resection of the distal condyle of
the proximal phalanx with the creation of a fibrous arthroplasty as
described for the surgical treatment of hammer toe. -
Then make a longitudinal incision over
the MP joint, and perform extensor tenotomy and capsulotomy, with
release of the medial and lateral collateral ligaments as necessary.
This is often enough to correct all deformities; however, a flexor
tendon transfer, as described in the treatment of flexible hammer toe,
is sometimes also required. -
If severe subluxation or dislocation of
the MP joint is present, release of the soft tissues will often not be
sufficient to allow a stable reduction, and a resection arthroplasty of
the MP joint might be necessary. Accomplish this by decompressing the
joint with the removal of 2–3 mm of the distal metatarsal head as
described previously. This is often adequate to allow reduction of the
joint and produce postoperative stability. Some beveling of the dorsal
and plantar condyles with a rongeur produces a smoother surface, which
permits easier dorsiflexion of the toe. -
Test the toe for stability in neutral
position as well as during dorsiflexion. After treatment of all bony
and soft-tissue deformities, stabilize the digit with a 0.062-inch
K-wire. The technically least demanding method is to insert the K-wire
from the PIP joint distally, out through the tip of the toe, and bring
it back in a retrograde fashion through the proximal phalanx into the
proximal metatarsal. Take care to ensure proper position of the toe
while placing the internal fixation. -
Close all wounds and bend the K-wire protruding from the toe.
Allow the patient to ambulate with weight bearing as tolerated in a
stiff postoperative shoe. At this point, begin gentle mobilization of
the MP joint. Arthrofibrosis often occurs at the MP joint after this
surgery, and loss of range of motion up to 50% is common. Avoid
proximal phalangectomy. The stability offered by the presence of the
wide base of the proximal phalanx is important. This flared area will
help to form a stable fibrous joint, allowing articulation with the
shortened and reshaped metatarsal head.
complication of this procedure. It can result from inadequate
shortening of the MP head or stiffness from inadequate rehabilitation
after pin removal. Incomplete soft-tissue release may also be a factor
contributing to recurrence. Compromise of the vascular supply at the
toe can occur from tension or spasm of the interdigital vessels, and
postoperative monitoring is strongly recommended. If vascular
compromise appears to jeopardize the viability of the toe, removal of
the K-wire will sometimes help to improve the digital blood supply.
Unfortunately, this usually also allows dislocation of the MP joint.
rubs on the inner sole of the shoe. Mallet toe is usually a fixed deformity and is less common than hammer toe.
-
Mallet toes that are flexible can occasionally be treated with percutaneous tenotomy of the FDL tendon.
-
With a fixed deformity, it is necessary
to decompress the distal interphalangeal joint. Excise an ellipse of
skin from the dorsal aspect of the distal interphalangeal joint, and
after release of the extensor apparatus and the collateral ligaments,
excise the distal condyle of the middle phalanx with a bone cutter.
This technique is similar to that described for correction of rigid
hammer toe. -
Hold the toe in a neutral position with a 0.045-inch K-wire.
-
Close the skin with interrupted vertical mattress sutures.
for 3 weeks, and then remove the pin and sutures. Then hold the toe in
a neutral position with a half-inch adhesive tape wrapping for another
3 weeks. Take care to avoid any injury to the proximal nail matrix.
pressure between the distal condyle of the proximal phalanx of the
fifth toe and the side of the shoe. Nonsurgical treatment for this
problem consists of protecting the skin with a donut device made of
soft material. In addition to this, wider, roomy shoes that minimize or
eliminate a confined toe box are also quite effective. Shaving of the
keratotic lesion can also help alleviate symptoms. If surgery is
necessary, the underlying principle is to remove the offending condyle
to relieve pressure on the skin.
 |
|
Figure 113.6. A: A hard hyperkeratotic region over the PIP joint of the fifth toe. B: The radiograph of the toe.
|
-
When the hard corn is on the dorsolateral
fifth toe, make a longitudinal incision over the fifth toe and dissect
around the PIP joint to expose it. -
Release the collateral ligaments and
resect the distal condyle of the proximal phalanx perpendicular to the
shaft using a bone cutter (Fig. 113.7).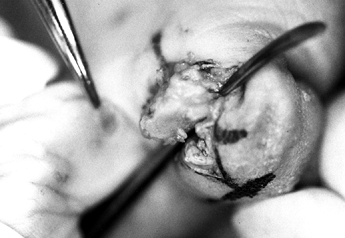 Figure 113.7.
Figure 113.7.
The distal condyle of the proximal phalanx, which has been exposed. A
freer elevator ensures that the soft tissues from underneath the
proximal phalanx have been released. -
Make certain all remaining bony surfaces are smooth (Fig. 113.8). Use a rasp as necessary.
![]() Figure 113.8. Radiograph of the toe after removal of the bony prominence.
Figure 113.8. Radiograph of the toe after removal of the bony prominence. -
Close the skin with interrupted sutures.
allowing full weight bearing in a postoperative shoe. At approximately
3 weeks after surgery, allow the patient to go to wide, laced shoes,
and stabilize the toe by buddy taping it to the fourth toe for
approximately 3–4 weeks.
usually resolve over approximately 3–6 months. Stiffness of the PIP
joint often occurs but is usually not symptomatic. If excess bone is
removed, a floppy toe may result. If the condyle is resected at a
significant angle to the shaft, a spike of bone may cause discomfort in
the adjoining fourth toe.
This hyperkeratotic skin reaction is caused by excess pressure in the
web space between the toes, often caused by a constricted toe box. The
moisture present in the region between the toes results in the
maceration of the keratotic lesion. The location of the corn is usually
at the area where one bony prominence is pushed into the adjoining toe.
 |
|
Figure 113.9. A: A soft corn between the fourth and fifth toes on the fibula side of the fourth toe. B: Area between the toes approximately 5 weeks postoperatively, with the soft corn almost completely resolved.
|
toes. If this is not satisfactory, removal of the offending condyle can
resolve the problem. If there is any question as to which is the
offending condyle, identify it by placing a small lead marker over the
soft corn, and obtain a radiograph (Fig. 113.10). This condyle may be on the toe with the lesion or on the adjacent digit.
 |
|
Figure 113.10.
A lead marker placed on the lesion demonstrates it to be at the level of the distal condyle of the proximal phalanx of the fifth toe. |
-
Resect the distal condyle as previously described for hammer toe.
-
If surgery is done on the fifth toe, use a longitudinal incision. Surgery on two adjacent toes is occasionally necessary.
for hammer toe, mallet toe, or a hard corn, depending on which joint or
digit is involved.
3–6 months. Excessive resection of the proximal phalanx can result in a
floppy toe, or if the remaining piece of bone is angulated, this can
result in malalignment of the toe. Surgery on the wrong toe
occasionally occurs; any doubt as to which digit is the offending toe
should be resolved prior to surgery.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.