Sensory Localization
sensation may occur because of lesions involving the peripheral nerves,
nerve roots, spinal cord, brainstem, or higher centers of the brain, as
may abnormal sensations, such as pain or paresthesia. Localization
depends on the pattern and distribution of the sensory abnormality.
disease involving peripheral nerve, spinal root, or sensory pathways
within the central nervous system (CNS). When the primary modalities
are normal in a particular body region, but the cortical modalities are
impaired, a parietal lobe lesion may be responsible. When some primary
modalities are involved more than others, the sensory loss is said to
be “dissociated.” The pathways conveying pain and temperature (the
spinothalamic tracts) run in a different location than the pathways
conveying touch, pressure, position, and vibration (the posterior
columns and medial lemniscus). After running divergently through much
of their central course, the sensory pathways converge again as they
approach the thalamus and remain together in the thalamocortical
projections. When the pathways are close together, such as in the
peripheral nerve, spinal root, or thalamus, disease processes tend to
affect all primary modalities to an approximately equal degree. When
the pathways are remote from each other, such as in the spinal cord and
brainstem, a disease process may affect one type of sensation and not
another, producing dissociated sensory loss. A common example of
dissociated sensory loss is lateral medullary stroke, or Wallenberg
syndrome. There is a very characteristic pattern of sensory loss, which
only involves pain and temperature and completely spares light touch.
The pain and temperature loss involves the ipsilateral face because of
involvement of the spinal tract of cranial nerve V, and the
contralateral body because of damage to the lateral spinothalamic
tract, sparing the light touch pathways that are running in the midline
in the medial lemniscus. A classic but not common cause of dissociated
sensory loss is syringomyelia. The pain and temperature sensory fibers
crossing in the anterior commissure are affected; light touch sensory
fibers running in the posterior columns are well removed from the site
of the pathology and remain intact. As a result, syringomyelia
characteristically causes sensory loss to pain and temperature with
preservation of light touch. Anterior spinal artery stroke is another
example of dissociated sensory loss. The infarction involves the
anterior two-thirds of the cord, sparing the posterior columns, which
are perfused by the posterior spinal arteries. The patients have dense
motor deficits and dense sensory loss to pain and temperature, but
normal touch, pressure, position, and vibration. Patients with
Brown-Séquard syndrome have extreme dissociation of modalities, with
loss of pain and temperature on one side of the body and loss of touch,
pressure, position, and vibration on the other side of the body.
nerve trunk or a spinal root tend to involve all of the sensory fibers
traveling in that nerve or root. The sensory loss involves all
modalities. Occasionally, generalized polyneuropathies may have a
predilection for large or small fibers, and can cause some differential
involvement of pain and temperature as opposed to touch and pressure.
These neuropathies are uncommon and tend to be generalized. When there
is marked sensory dissociation affecting one body region, the pathology
is virtually always going to be in the CNS, specifically in those
regions where the different sensory pathways run in widely divergent
locations.
sensory loss, in addition to the modalities involved, is the
distribution of the abnormality. Deficits in a “hemi” distribution
obviously suggest CNS disease, likely involving either the cortex or
the thalamus. Crossed deficits, affecting the face on one side and the
body on the opposite side, suggest brainstem disease. Deficits
involving both sides of the body below a certain level (e.g., T5)
suggest spinal cord disease. A spinal cord level with “sacral sparing”
suggests intraparenchymal spinal cord pathology rather than a
myelopathy due to external pressure. Deficits due to generalized
peripheral nerve disease typically involve the most distal body regions
in a “stocking-glove” distribution. Sensory loss due to dysfunction of
a peripheral nerve, nerve root, or nerve plexus follows the innervation
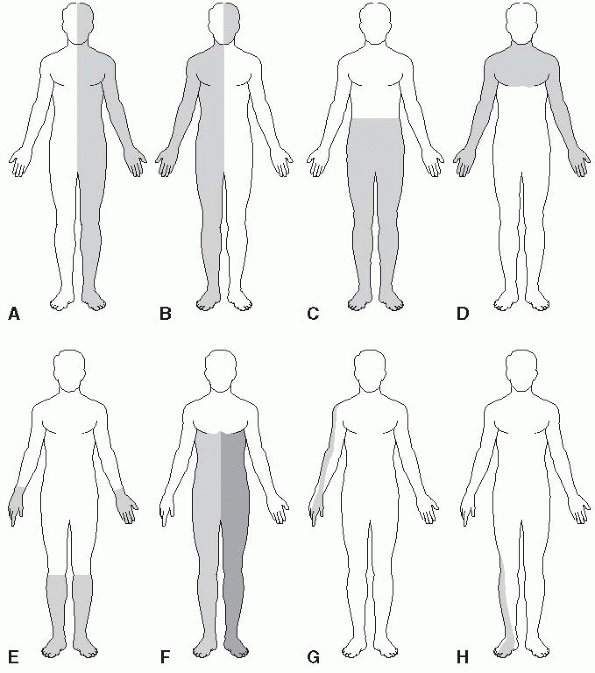
pattern of that particular structure. Figure 26.1
depicts some of the commonly seen patterns of sensory loss. In
hemi-distribution sensory loss there is a certain amount of
side-to-side crossing or overlap of innervation along the anterior
midline, which is greater on the trunk than on the face. Because of
this midline overlap, organic sensory loss usually stops short of the
midline,
while nonorganic sensory loss may “split the midline” (see further on).
Sacral sensation is not tested as part of a routine neurologic
examination. In some instances, sensation in the saddle distribution
should be examined (e.g., when a conus medullaris or cauda equina
lesion is a possibility; when there is evidence of a myelopathy; or
when there is bladder, bowel, or sexual dysfunction).
 |
|
FIGURE 26.1 • Some common patterns of sensory loss. A. Hemisensory loss due to a hemispheric lesion. B. Crossed sensory loss to pain and temperature due to a lateral medullary lesion. C. Midthoracic spinal cord level. D. Suspended, dissociated sensory loss to pain and temperature due to syringomyelia. E. Distal, symmetric sensory loss due to peripheral neuropathy. F. Crossed spinothalamic loss on one side with posterior column loss on the opposite side due to Brown-Sequard syndrome. G. Dermatomal sensory loss due to cervical radiculopathy. H. Dermatomal sensory loss due to lumbosacral radiculopathy.
|
and severe motor disabilities may occur because of impaired sensation.
This is particularly evident with parietal lobe lesions, but motor
dysfunction may also occur with lesions involving the posterior roots,
peripheral nerves, posterior columns of the spinal cord, or the other
central sensory pathways. Conversely, motor dysfunction may affect
sensory discrimination. When equal weights are placed in a patient’s
hands, she may underestimate the weight on the side with cerebellar
dysfunction and overestimate it on the side with extrapyramidal
dysfunction.
pathology involving the sensory receptors, but this does not often
arise in primary neurologic illnesses. Pain and pruritus due to skin
irritation, traumatic denudements, and burns may result from
abnormalities of the receptors or the nerve filaments to them, and
decreased sensation in callosities and scars may result from
involvement of the end-organs and smaller filaments.
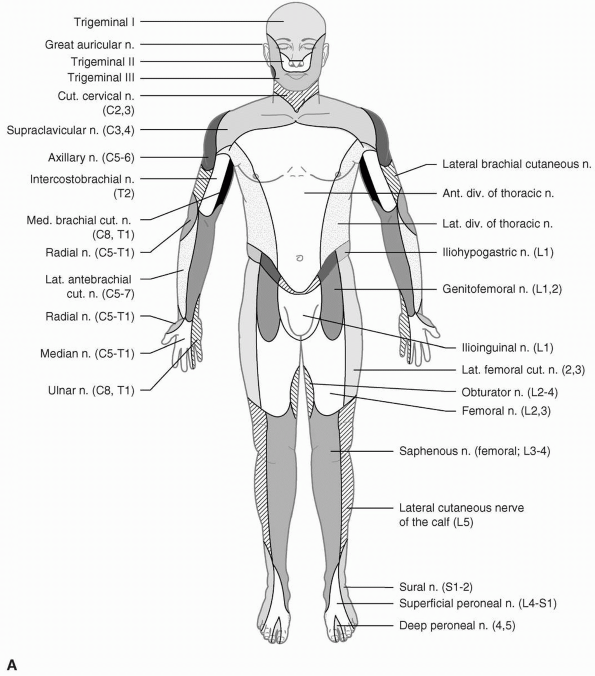
abnormality corresponds to the distribution of the specific involved
nerve. The areas of skin supplied by various nerves are shown in Figure 26.2. Within the involved area, all sensory modalities are affected. Sensory distributions
may vary slightly from individual to individual, and the mapped area
may not correspond precisely to a published text or atlas. An excellent
source for a pictorial/graphic demonstration of peripheral nerve
distributions is http://www.neuroguide.com/nerveindex.html.
 |
|
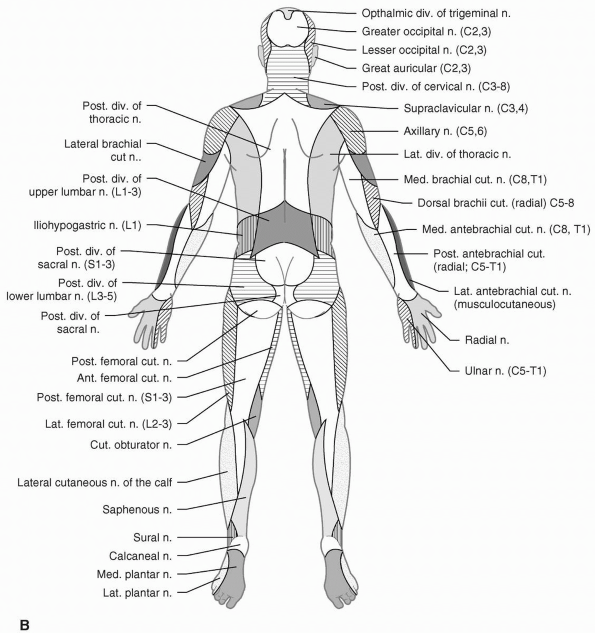
FIGURE 26.2 • The cutaneous distribution of the peripheral nerves. A. On the anterior aspect of the body.
|
 |
|
FIGURE 26.2 • (Continued) B. On the posterior aspect of the body.
|
typically smaller than the area of light touch loss, and smaller than
the published peripheral nerve or dermatome distributions. The deficit
to light touch usually corresponds more closely to a nerve distribution
than the pinprick loss. In a patient with a focal nerve or root lesion,
it may be possible with careful testing to identify a dense zone of
severe sensory loss, surrounded by areas of milder sensory loss.
Occasionally, there is spread of sensory loss beyond the field of an
injured nerve.
often the first modality affected, but in severe cases all
exteroceptive, proprioceptive, and combined modalities are impaired.
Most axonopathies are length dependent, and the distribution of sensory
loss usually involves predominantly the distal segments, causing a
stocking-glove distribution of blunted sensation. However, the margins
of the involved area may be poorly demarcated, with no sharp border
between the normal and hypesthetic areas. Some generalized neuropathies
have a predilection to involve predominantly large or small fibers.
Peripheral nerve disease may also cause paresthesias, or pain that is
either constant or lancinating in character. The nerves themselves may
be sensitive and tender to palpation, and there may be pain on brisk
stretching of the affected nerves and increased susceptibility to
ischemia. There sometimes is hyperalgesia or allodynia in the involved
area, even though the sensory threshold is raised.
corresponding cranial nerve ganglia, is also associated with sensory
changes. Although classically a remote effect of small cell carcinoma
of the lung, sensory neuronopathy is associated with a number of other
conditions, including pyridoxine intoxication, Sjögren syndrome, and
lymphoma. In herpes zoster, there is severe, lancinating pain in the
distribution of the affected ganglia.
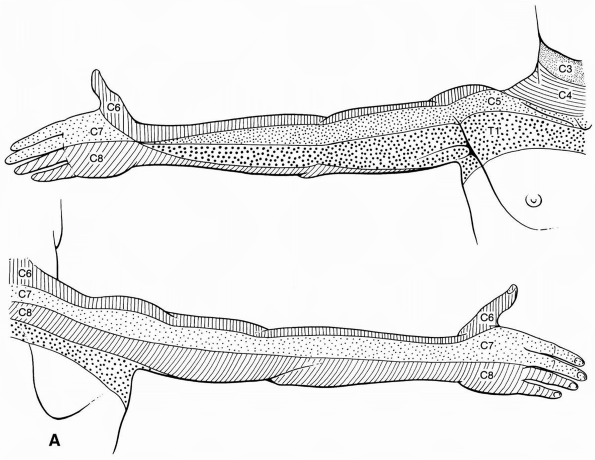
compression, are accompanied by diminution or loss of sensation, pain,
or paresthesias, but the distribution is segmental and corresponds to
the involved dermatome (Figure 26.3). As with
focal neuropathy, in compressive radiculopathy the touch deficit is
larger and often corresponds better to the published dermatome than the
pinprick deficit. Pain may be either constant or intermittent, and is
often sharp, stabbing, and lancinating. It is increased by movement,
coughing, or straining. There may be either hypalgesia or hyperalgesia.
Because of dermatome overlap, sensory changes may be difficult to
demonstrate if only one root is involved.
impairment of one or more modalities of sensation, or perversions of
sensation in the form of either pain or paresthesias, may develop. The
area of sensory involvement may involve all levels below the lesion,
but occasionally the sensory level is well below the level of the
lesion; a sensory level on the trunk has been reported in lesions of
the lower brainstem. Sensory loss is usually dissociated, with
impairment of certain modalities and sparing of others. Because of the
redundancy of the touch pathways, pain and temperature testing may be
more useful than tactile sensation in evaluating CNS disease. Testing
for the ability to detect the direction of skin movement above and
below the level of the lesion and searching for a vibratory level may
be helpful.
medulla may impair kinesthetic sensation in the upper extremities more
than in the lower. Patients with pontine, medullary, or spinal cord
lesions occasionally experience “central” pain. Lhermitte sign, sudden
electric-like or painful sensations spreading down the body or into the
back or extremities on flexion of the neck due to involvement of the
posterior columns, may occur with focal lesions of the cervical cord,
multiple sclerosis, or other degenerative processes.
 |
|
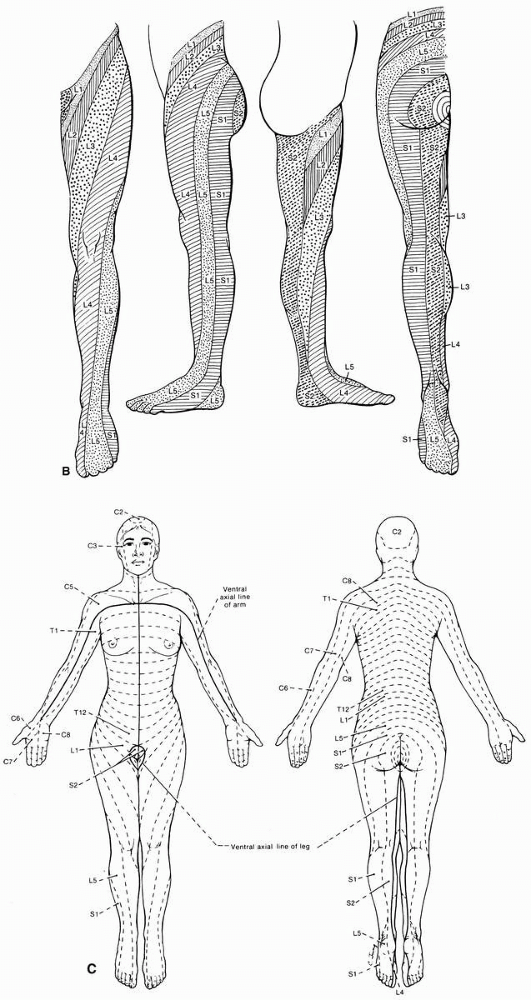
FIGURE 26.3 • The segmental innervation. A. The upper extremity.
|
 |
|
FIGURE 26.3 • (Continued) B. The lower extremity. C. The anterior and posterior aspects of the entire body. (Modified from Keegan JJ, Garrett FD. Anat Rec 102:409-437, 1943.)
|
lesions is variable; the impairment may recede downward in a segmental
manner; the return may start in the sacral distribution and ascend, or
there may be a gradual recovery of function over the entire affected
area. Pressure sensation returns first and its recovery is usually the
most complete, followed, in turn, by tactile, pain, cold, and heat
sensibilities.
interpretation by the parietal cortex must first pass through the
thalamus. The thalamus is thought to be the end-station for pain, heat,
cold, and heavy contact, where sensory impulses produce a crude,
uncritical form of perception. Thalamic lesions usually cause
impairment of all sensory modalities on the opposite side of the body.
A severe and extensive lesion may cause gross impairment of all forms
of sensation. Marked loss of appreciation of heavy contact, posture,
passive movement, and deep pressure perception occurs, and the
thresholds for light touch, pain, and temperature sensations are
raised. Thalamic lesions are often associated with sensory perversions,
such as paresthesias and hyperesthesias, or painful hyperpathias. In
the thalamic pain (Dejerine-Roussy) syndrome, there is blunting, or
raising of the threshold, of all forms of sensation on the opposite
side of the body, without true anesthesia. Suprathreshold stimuli
excite unpleasant sensations, and any stimulus, even the lightest, may
evoke a disagreeable, often burning, pain. Slight hot and cold stimuli,
or light cutaneous sensations, cause marked discomfort. The
overreaction is termed hyperpathia. Impairment of sensation accompanied
by intractable pain in the hypesthetic regions is called anesthesia
dolorosa. In addition to the sensory changes, hemiparesis and
hemianopia usually occur and, less frequently, hemiataxia,
choreoathetosis, and unmotivated emotional responses. Pain of central
origin is most often associated with thalamic lesions, but may
occasionally result from involvement of other central pain pathways.
Occasionally, pleasurable stimulation, such as application of a warm
hand to the skin on the affected side, may be markedly accentuated.
This overreaction is due to a thalamic lesion or to release of thalamic
function from normal cortical control by damage to higher centers.
Every stimulus acting on the thalamus produces an excessive effect on
the abnormal half of the body, especially as far as the affective
element—the pleasant or unpleasant character in its appreciation—is
concerned.
limb of the internal capsule causes variable, sometimes extensive,
impairment of all types of sensation on the opposite side of the body.
Because the sensory fibers are crowded closely together, the sensory
loss is more severe than with isolated cortical lesions. The changes
are similar to those that follow a thalamic lesion, but pain is rare.
loss of sensation, but there is a raising of the threshold for both
exteroceptive and proprioceptive sensations of the opposite side of the
body. Sensation is often disturbed more in the upper than in the lower
extremity, trunk, or face. The distal parts of the extremities are
affected more than the proximal portions, with a gradual transition to
more normal perception approaching the shoulder and hip. Parietal
lesions primarily cause disturbances in discriminatory sensation.
Detailed and critical examination of sensory functions may be necessary
to detect parietal lobe lesions. The threshold for pain stimuli is
raised very little in parietal lesions, although a prick may feel less
sharp than on the normal side; with deeper lesions the threshold is
more definitely raised. Qualitative appreciation of heat and cold are
present, but there is loss of discrimination for slight variations in
temperature, especially in the intermediate ranges. Light touch
perception is little disturbed, but tactile discrimination and
localization may be profoundly affected. There often is severe
impairment of position sense resulting in sensory ataxia and
pseudoathetosis, but vibratory sensation is only rarely affected
(another instance where vibration and position sense loss are
dissociated). Astereognosis is common, but both small and large objects
may have to be used to detect the deficit; sometimes a delay in
answering when objects are placed in the affected hand, with no delay
with the other hand, may be a clue to minimal involvement. Bilateral
simultaneous testing for stereognostic sense, placing identical objects
in both hands, may be useful. Sensory inattention, or extinction, is
often an early and important diagnostic finding in parietal lobe
lesions. Other possible findings include baragnosis, agraphesthesia,
impairment of two-point discrimination, autotopagnosia, anosognosia, or
Gerstmann syndrome.
The
ability to distinguish two cutaneous stimuli to the same side of the
body but separated by a brief time interval is also impaired with
parietal lobe lesions. Spontaneous discharges from the parietal cortex
frequently cause contralateral paresthesias that may constitute a focal
sensory seizure or the sensory aura preceding a jacksonian motor
convulsion. Only rarely do spontaneous discharges from the parietal
cortex cause pain.
decreased sensibility. Areas of hypesthesia, hypalgesia, anesthesia,
and analgesia are commonly encountered that may be complete or partial,
affect all modalities or be dissociated. Even normal individuals, or
those with organic sensory loss, may be suggestible and have spurious
sensory findings.
is failure to follow any sort of anatomical distribution. The
demarcation between normal and abnormal often occurs at some strategic
anatomical point that has no neurologic significance, such as a joint
or skin crease, causing a finding such as numbness circumferentially
below the elbow, wrist, shoulder, ankle, or knee. Nonorganic facial
sensory loss often stops at the hairline and angle of the jaw, a
nonanatomic distribution. A real spinal sensory level on the trunk
slants downward from back to front; a functional level may be perfectly
horizontal. The term stocking-glove sensory loss is used to describe
both hysteria and peripheral neuropathy. The key to understanding this
confusing usage is the type of stocking. When sensory loss due to
length-dependent peripheral neuropathy extends to about the level of
the knees it appears in the hands, causing loss in a glove-knee sock
distribution; with hysteria the impairment may be distal to the wrists
and ankles: a glove-ankle sock distribution. The border between normal
and abnormal is usually abrupt and well demarcated, more discrete than
in organic sensory loss, and may vary from examination to examination,
or even from minute to minute. Sensation may be different on the
ventral and dorsal surfaces. Responses are typically inconsistent. In
spite of complete loss of cutaneous sensibility, the patient may have
intact stereognosis and graphesthesia, or in spite of complete loss of
position sense may be able to perform skilled movements and fine acts
without difficulty, and have no Romberg sign. On finger-to-nose
testing, the examiner may touch one finger of the “anesthetic” hand and
ask the patient to touch her nose with it; a patient with organic
exteroceptive sensory loss will not know which finger was touched,
while those with organic proprioceptive loss can’t find their nose. The
hand wandering widely before eventually finding the nose suggests
histrionic tendencies. In the search test, the patient holds the
involved hand in the air and searches for it with the unaffected hand.
In nonorganic loss there may be no difficulty, but with bona fide
proprioceptive loss, performance is poor with either hand.
sensory loss is nonorganic. The author has seen all of these “tricks”
fail (i.e., indicate the sensory loss is not real when it is), at one
time or another, save one: the SHOT syndrome. In the SHOT syndrome, the
patient claims to have no Sight in the eye, no Hearing in the ear, no
Olfaction in the nose, and no Touch sensation on the body, all on the
same side. This pattern is of course utterly impossible on an anatomic
basis and its presence reliably indicates that hemi-body numbness is
nonorganic. Another sometimes helpful technique to bring out nonorganic
sensory loss is the “yes if you feel it/no if you don’t” maneuver.
After demonstrating the patient is unable to feel a given stimulus in a
given distribution, instruct her to close her eyes and say “yes” every
time she feels a stimulus and “no” when she does not; the gullible will
respond with “no” every time the alleged anesthetic region is
stimulated.
the absence of organic changes by checking sensation while the hands
are in some bewildering position where it is difficult to tell which
side is which, such as crossed behind the back or intricately entwined.
A commonly used technique is to have the patient cross the
hyperpronated forearms and hold the hands with little fingers up, palms
together, and fingers interlocked. The hands are then rotated downward
and inward, then upward, so that the little fingers are facing the
chest. Anyone who has ever done this knows how
difficult
it is to tell which finger belongs to which hand. The patient responds
as digits are stimulated randomly. It matters little whether eyes are
open or closed, and in fact the test may work better with eyes open.
The patient with nonorganic hemianalgesia may make errors, while the
one with organic loss will not. The nonorganic patient may respond
slowly, delay answering, or betray signs of the effort required. It is
of course imperative that the examiner accurately keep track of which
side is which. With practice, performance improves rapidly, so the test
is most conclusive the first time it is done.
distribution, almost invariably on the left side. Sensory changes along
the midline may provide useful clues. Because of the overlap along the
midline of the trunk, organic sensory loss does not usually extend to
the midline, and, when stimulating from the hypesthetic to the normal
side, sensation begins to return slightly before the midline is
reached. With nonorganic loss, the change may take place abruptly at
the midline or even beyond it. This finding is not reliable on the
face, where organic sensory loss does more accurately obey the midline.
With nonorganic hemi-anesthesia, the midline change may include the
penis, vagina, and rectum, a finding rare with organic lesions. There
may even be midline splitting of vibration, so that the patient claims
to perceive a difference in the intensity of vibration when the fork is
placed just to right or left of the midline over the skull, sternum, or
symphysis pubis, each a single bony structure, or comparing the medial
ends of the clavicles or the medial incisor teeth. In all these
locations, the vibration is transmitted to both sides, and patients
with organic hemi-anesthesia do not perceive any difference in
vibration along the midline. Somatosensory evoked potential studies may
aid in differentiating organic from nonorganic sensory loss.
